- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Why publish with EJCN?
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Materials and methods.
- < Previous
Components of heart failure management in home care; a literature review
- Article contents
- Figures & tables
- Supplementary Data
Tiny Jaarsma, Maaike Brons, Imke Kraai, Marie Louise Luttik, Anna Stromberg, Components of heart failure management in home care; a literature review, European Journal of Cardiovascular Nursing , Volume 12, Issue 3, 1 June 2013, Pages 230–241, https://doi.org/10.1177/1474515112449539
- Permissions Icon Permissions
Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and secondary care. Although guidelines on optimal HF care exist, no specific description of components that are applied for optimal HF care at home exist. The objective of this review was to describe which components of HF (home) care are found in research studies addressing homecare interventions in the HF population.
The Pubmed, Embase, Cinahl, and Cochrane databases were searched using HF-, homecare services-, and clinical trial-related search terms.
The literature search identified 703 potentially relevant publications, out of which 70 articles were included. All articles described interventions with two or more of the following components: multidisciplinary team, continuity of care and care plans, optimized treatment according to guidelines, educational and counselling of patients and caregivers, and increased accessibility to care. Most studies ( n =65, 93%) tested interventions with three components or more and 20 studies (29%) used interventions including all five components.
There a several studies on HF care at home, testing interventions with a variety in number of components. Comparing the results to current standards, aspects such as collaboration between primary care and hospital care, titration of medication, and patient education can be improved.
Patients with heart failure (HF) constitute a large group within health care worldwide. The prevalence of symptomatic HF is estimated to 2% of the population, approximately 15 million in Europe. 1 The mean age of HF patients is around 75 years and HF is a leading cause of hospitalization for elderly patients at high healthcare costs. 1 Patients with HF often need complex care due to their older age, poor social support, cognitive decline, comorbidities, and polypharmacy. 2 In addition, the prognosis of HF patients is poor and half of the patients die within 4–5 years after their diagnosis. 1 All these aspects are challenges when planning HF care. A growing number of HF patients will be in need of lifelong care with regular follow up to achieve and maintain optimal treatment and support self-care management. Ideally, long-term follow up should be integrating the primary and secondary care interfaces to facilitate clinical continuity. 3 – 7 Clinical continuity of care can be defined as a consistent and coherent approach to the management of health conditions that is responsive to patients’ needs including a seamless transition over time between various healthcare providers in different settings. 3 , 5 – 9 The concept of continuity of care has been linked to quality of care and has especially been advocated in the management of chronic conditions such as HF.
Home-based interventions have been found to reduce mortality 4 , 10 and morbidity 11 and preserve physical and mental health 6 in patients’ suffering from HF. HF clinics are common in several European countries 7 and, also, in primary care the number of specialized HF clinics is increasing. 5 However, HF clinics are often situated at the hospital or at a primary healthcare centre. 7 , 12 When exploring the prevalence of home-based care in Europe, we found that very few of the HF management programmes offered home care and that collaboration across the primary–secondary care interface was unsatisfactory. 7
In a meta-analysis on the effectiveness of disease management programmes, the authors separated the multidisciplinary HF clinics from the programmes that provided specialized follow up in a non-clinical setting. They concluded that programmes in a home-based setting were found to be as effective in reducing mortality and rehospitalization as the clinic setting. However, no information was available on the specific components of the homecare intervention. In general, no specific description of components for HF care at home exists. In developing and further testing of disease management programmes in home care, an overview of the components that are included in these programmes can be helpful. Therefore the purpose of this review was to describe which components of HF (home) care are found in research studies addressing homecare interventions in the HF population. In this study, home care is defined as health care or supportive care provided in the home by licensed healthcare professionals.
Search strategy
A comprehensive search was conducted through the Pubmed, Embase, Cinahl, and Cochrane databases of medical literature published until April 2011 with a customized search strategy for each database. The search strategy consisted of HF- and homecare-related search terms ( Table 1 ). After consultation with literature search experts from the university library, we tailored the search strategy to each database to be as specific as possible. We specified our search strategy by including Mesh terms, specific terms in title and abstract, no review and editorials, type of trials, and language English and excluding transplantation. Not all databases however allowed use of MESH terms and therefore, in these cases search engine specific terms were used (e.g. “exp” in Embase). The thesaurus of each database was also different so the term “home care” needed to be adapted per database.
Bibliographic search strategy
Components of homecare studies
MDT, multidisciplinary team; CP, care plan; OT, optimized treatment; ES, educational strategies; IAC, increased access to care, APN, advanced practice nurse; DM, disease management; HF, heart failure; Prosp., prospective research; Quasi exp., Quasi experimental: RCT, randomized clinical trial; TM, telemonitoring.
Selection of articles
The literature search identified 703 potential relevant publications: Pubmed ( n =181), Embase ( n =254), Cinahl ( n =91), and Cochrane ( n =177). Several articles ( n =236) were simultaneously present in more than one database. To be included in the present review, publications were assessed by two independent reviewers using the following inclusion criteria: The articles had to: (1) describe a clinical trial in a homecare setting; (2) describe studies performed in patients with HF with an age over 18 years; (3) be published in English; and (4) be original, full-text articles published in peer-reviewed journals. Exclusion criteria were: (1) addressing end-of-life care only; (2) not caring for HF patients; (3) not addressing a programme of disease management; and (4) not reporting on an intervention. In total, 379 articles were excluded: 21 articles assessing palliative care or end-of-life care; 24 articles not addressing patients but caregivers or professionals; 68 articles addressing a medical agent, an instrument, or only exercise and not a disease management programme or other components (e.g. meditation, relaxation); 25 articles addressing predictors or relationships; five articles addressing design of the study only; 32 articles addressing pilot studies; four articles performing beta-testing of equipment; 87 articles not addressing patients with HF or did not consist of a primary HF population; one article not describing a homecare intervention; another 112 articles not fulfilling the inclusion criteria; and 18 papers describing the same study. Figure 1 shows the flowchart of inclusion.

Flowchart of inclusion
Assessment of articles
For the purpose of describing components of the homecare programmes, all articles were read and organized in a table describing the following components. 13 The list of components was derived partly from earlier described key components and guidelines: 1 , 13
multidisciplinary team
continuity of care and care plans
optimized treatment according to guidelines
educational and counselling of patients/families/caregivers
increased accessibility to care.
We also added a separate column ‘other components’ on our data analysis sheet.
In total, 70 articles were summarized in a table describing components of home care in HF patients (see Appendix 3). Most studies ( n =65, 93%) tested interventions with three components or more. Only five (7%) studies tested interventions with two components and 20 studies (29%) included all five components in their intervention. We did not find additional components. The following paragraphs describe the findings per component within the different studies.
Multidisciplinary team
Most studies ( n =69, 99%) reported care provided by a multidisciplinary team but a great deal of heterogeneity regarding the professionals involved was described. Collaboration between primary care and secondary care was scarcely reported.
Team members
In almost all studies, nurses played a coordinating or leading role. They were described as homecare nurses, hospital nurses, HF nurses, cardiac rehabilitation nurses, research nurses, practice nurses, and/or district nurses, but description of the specialization or clinical background were lacking. Almost all programmes also had physicians involved, which could be cardiologists, and/or primary care physicians or other specialists such as geriatricians or internists. Two studies specifically reported collaboration between the primary care physician and cardiologist. 14 , 15 In one study, the team existed of a trained doctor’s assistant and a primary care physician. 16 In another study, the team existed of a physician, physiotherapist, ECG technician, and a psychologist. In these teams, nurses were not involved. 17
Additionally, other professionals (psychologist, dietician, physical therapist, social worker, pharmacist) were involved in the programmes, 18 – 23 mostly as member of the multidisciplinary team or occasionally as the main provider of an intervention (e.g. a pharmacist). 24 , 25
Education of the team members
In general, the specific training of the team members was not well described in the manuscript. Specific training for nurses was mostly described in general terms such as for example: ‘as a specific HF programme based on AHCPR guidelines’ or ‘trained nurses’ 26 or ‘advanced practice nurse’ 27 or ‘a one day training course’ or ‘Nurses underwent brief training programme regarding problems and treatment options associated with this particular group of patients’. 11 , 28 , 29 In one study, nurses participated in an interactive practitioner training as well as role playing and audio taping, to help the nurse increase their skills in communicating with and motivating their patients to adherence to treatment instructions. 29 In another study, advanced practice nurses participated in a 2-month orientation and training programme focused on developing their competencies related to detection of deterioration in HF in elderly patients, how HF is complicated by common comorbid conditions, and optimal therapeutic management. 19 Furthermore, the advanced practice nurses participated in a training programme focused on educational and behavioural strategies in the home to address patients and caregivers unique learning skills. 19 For other healthcare providers, specific training even less well described such as ‘the health coaches underwent a highly scripted “training process”’ or ‘the study pharmacist had combined experience as hospital and community pharmacist, had a doctor or pharmacy degree and completed a one-year clinical residency in home care’.
Continuity of care and care plans
Several studies introduced a specific care plan or clinical pathways for the study. 11 , 22 , 29 – 51 In total, 47 (67%) of the studies described a care plan as part of their intervention. From the description in the publication, it was not always clear if the care plan was integrated between primary and secondary care. However, in other studies, specific descriptions of the goals and responsibility of the care plan were described. 30 , 32 In one study, the hospital physician provided a written management plan regarding pharmacological treatment and monitoring to the primary care physicians. 35 In another study, the intervention specifically focused on the transition of care with improved intersector linkages using a joint care plan. 43 In that study, linkages were created by including a nursing transfer letter, a telephone outreach, a notification of who was responsible for the care, and a patient-held documentation.
Optimized medical treatment according to guidelines
Optimized treatment according to guidelines (e.g. medication, implementation of devices) was reported in 31 (44%) of the 70 studies. Optimization of drug treatment was more explicitly described as one of the components of the intervention programme in 23 (33%) of the 70 studies. It was carried out by health professionals in the hospital (14 studies) 14 , 19 , 21 , 28 , 34 , 36 , 41 , 53 – 58 or by primary care nurses or physicians within primary care (six studies). 20 , 25 , 37 , 46 , 51 , 52 In three studies, it was not clear who performed the optimization of the medications. 40 , 59 , 60
Drugs were prescribed and titrated to optimal doses either following guidelines and protocols or following a tailored recommendation for optimization of medical therapy with individual titration plan. Some studies reported methods for adjustment of diuretics and recommendations for discontinuation of inappropriate medications. 21 , 25 , 37 , 46 , 52 , 59 , 60
Methods of drug titration and adjustment of diuretics
A few studies described their method used for the titration of HF medication. 14 , 19 , 20 , 28 , 33 , 34 , 37 , 46 One study reported that the nurse evaluated the data transmitted by the patient (i.e. weight, blood pressure, heart rate) and subsequently titrated medication. 34
Other studies described nurses following an established protocol in close collaboration with the family physician or cardiologist, especially when it was necessary to start new treatment or adjust existing medication. 14 , 17 In these studies, no precise description of the protocols was given. In another study, all patients were given a management plan by the investigator that described the pharmacological treatment they should receive, in what order, and how it should be monitored. 38 The pharmacological treatment focused on appropriate doses of angiotensin-converting enzyme inhibitors and beta-blockers. If severe symptoms were present, an aldosterone antagonist was prescribed according to regional guidelines. The study consists of three different strategies; usual care, nurse telephone support, and home telemonitoring. 38 In three studies, it was mentioned that strict treatment protocols or accepted guidelines were used for titration of medication but no details on the content of the protocols were provided in the articles. 56 , 58 , 60
The methods for adjustment of diuretics were reported in four studies. 20 , 28 , 31 , 46 In one study, investigators developed a set of algorithms based on accepted national CHF guidelines including the appropriate use of potassium sparing diuretics, to help determine the adequacy of medication regimes. 46 Another study reported the application of infusion of diuretics in case of an emergency by the supervising physician. 28 One study described an intervention where, after liaison with the primary care nurse and the cardiologist, the cardiac nurse arranged a flexible diuretic regimen in response to the patient’s symptoms and weight. 20 Another study described an intervention where the nurse informed the patient about how to modify the dose of diuretics without waiting for a medical visit. 31
Responsible for medication adjustment
In five studies, the primary care physician was reported being responsible for the adjustment of HF medication. Nine studies reported the cardiologist as the supervisor of drug prescription and titration of drugs. In a few of these studies, the (community) nurse made adjustments of diuretics, angiotensin-converting enzyme inhibitors, or beta blockers under the supervision of a cardiologist. 41 , 59 In one study, the cardiologist in difficult cases (multiple comorbid conditions or concurrent medications) provided expert advice to the nurse by telephone. 54 In another study, optimization of medical therapy was performed by the HF cardiologist specialized in HF after consultation with the patient’s family and primary care providers. 55
Education and counselling of patients/families/caregivers
Education was described in 61 (87%) of the 70 studies. In these studies, education was mostly part of a larger programme.
Provider and methods
In most studies, the nurse provided patient education to patients (and families). In three programmes, other healthcare workers (e.g. pharmacists) provided patient education. 24 , 25 , 61
Almost all programmes used verbal educational strategies. In several educational programmes, booklets, diaries, education maps, reminder cards, pamphlets, or brochures were applied. Other strategies included a remote video system, email reminders, 44 , 62 educational modules via telehealth, or motivational messages. 63 Group training was mentioned in one programme. 55
Partners, family, or other caregivers when providing patient education were included in patient education in seven programmes. 19 , 23 , 32 , 33 , 60 , 64 , 65
Topics for patient education
Almost all programmes educated patients on HF in general, detection of deterioration, and advice and instruction on use of medication, diet, and physical activity/exercise training. Smoking cessation was addressed in three studies. 25 , 26 , 31 Four programmes reported education in coping with difficult emotions 19 , 47 , 61 , 66 and one study communicated with family and healthcare providers, using relaxation and cognitive symptom management techniques. 60 Education on alcohol intake, sexual activity, and necessity of vaccinations and capabilities of patients to travel or work was described in one study. 21 In one study, individual problems, often related to comorbid conditions, were given extra attention. 67
Increased access to care
Increased accessibility to care was provided in 65 (93%) of the 70 programmes, either by telephone support, home visits, or telemonitoring. Some programmes used a standardized approach to increased accessibility to care by planned visits to an outpatient clinic or planned telephone support. 14 , 23 , 24 , 31 – 35 , 43 , 45 , 50 , 57 , 58 , 61 – 63 , 66 , 68 – 76 Others opened a helpline for patients in case of questions or problems. 16 , 17 , 24 , 28 , 37 , 38 , 40 – 44 , 51 , 61 , 63 , 63 , 77 – 82 The opportunity to contact healthcare providers for patients varied and the healthcare provider is often available during office hours or, in some programmes, 24 hours a day.
A different variety of systems for telemonitoring was found, ranging from assessment of symptoms and/or vital signs to data transmission and automatic alarms.
This article provides an overview of studies evaluating homecare interventions in the HF population during the past decades. The aim of the study was to describe the components of the interventions and not focus on the outcomes and effectives, since that has been addressed in previous reviews. 83 – 86
Although most studies included several components, there was a large variety in the combinations of components. The most common component in the articles was a multidisciplinary team (99%). The least reported component with 44% was optimized treatment according to guidelines. All articles described studies on interventions with two components or more and 29% of the studies included interventions with five components. Although we did not aim to address the effectiveness of the separate components or the effectiveness of the number of components, the variety in programmes indicate that standards of care to HF management might be needed to further improve patient care. 2 It probably is not realistic to expect that components can be separated in explaining effectiveness of disease management programmes, since several components might be related to each other. However, for teams that aim to improve the quality of their existing programmes, the overview provided in this paper might be beneficial. The recently presented WHICH? trial contains all five components and is expected to provide important information about optimal HF care in hospital or at home. 87
Most programmes in this review reported working with a multidisciplinary team. The content of the team varied considerable per study and also the education of the professionals in the care for the patient with HF was not clearly described or, if described, very heterogeneous ranging from no additional HF training to, for example, a 2-month orientation on HF. The Heart Failure Association of European Society of Cardiology recently addressed the need for appropriate education and training of healthcare professionals. 2 Having a multidisciplinary composition of the team did not always mean that the collaboration involved different specialties, disciplines, and levels of HF care. Collaboration between primary care and secondary care were most often not clearly described. Within the studies found in our review, there were only two studies in which this collaboration between GPs and cardiologists was mentioned explicitly related to the care of patients with HF.
The role of primary care is not always clear, but in many countries primary practice is the most frequent point of consultation for patients with deterioration of signs and symptoms of HF. 2 , 12 Patients with HF also may consult other healthcare workers such as cardiologist and/or HF nurses. 12 To ensure the continuity and quality of care, it seems important that there is a close collaboration between different disciplines and between primary care and hospital care. In majority of studies, the cardiologist supervised the home care of patients with HF. The GP was only mentioned in five articles as being the supervisor of care. This reflects the current state of the art in disease management in HF, namely that there is a lack of continuity of care. The majority of HF disease management programmes are primarily hospital based with care delivered at outpatient clinics, occasionally with outreach to patient’s homes by HF nurses. 87
An important tool to ensure continuity of care is the care plan or clinical pathway. Within this review, 47 (67%) out of the 70 articles reported the use of care plans. Most of these care plans are designed within the hospital environment and implemented in primary care. Care plans are an important part of the continuity and coordination of care of patients with HF. 9 A care plan consist of the medical history of the patient, responsibility of health professionals, planned and reached patient’s goals, patient’s wellbeing, and the treatment plan. Care plans or clinical pathways consisted mainly of patient goals, patient’s wellbeing, and treatment plan and only seldomly the responsibility of health professionals.
Despite the ESC recommendations of including optimal medical treatment in a HF management programme, only 23 (33%) out of the 70 intervention studies described medication titration as part of the intervention. Medication titration was often performed by the cardiologist or HF nurse in the hospital and in five studies the GP was responsible for adjustment of medication. This might reflect both the age of some papers and also difference in practice, education, and legal aspects in some countries. However, an increasing role for medication uptitration in the patients’ home might be possible using new telemonitoring approaches. 89 – 91
An important component of optimal care for patients with HF is education and counselling of patients and families /caregivers. Education was a component in almost all programmes and topics for education mostly entailed: HF in general, detection of deterioration,and advice and instruction on use of medication, diet, and physical activity/exercise training. Only four studies specifically addressing coping as a topic of education.
To improve this adherence to treatment, social relations and a sufficient social network have proven to be very important. 1 , 2 Although the guidelines recommend that family members should be invited to participate in education programmes and decisions regarding treatment and first studies indicate the importance of including family support, only seven (10%) out of the 70 articles reported the families and caregivers being involved in education. 92
This study gives first insight in components included in homecare programmes but did not give information about effectiveness. This should be addressed in future reviews to help the reader understand which components should be further developed.
From this review, it is concluded that there are several studies that focus on aspects of optimal HF care at home, with a variety in number of components. Comparing the results to current standards, aspects such as collaboration between primary care and hospital care, titration of medication, and patient education can be improved.
This study was supported by the EU Seventh Framework (Homecare 222954).
Dickstein K , Cohen-Solal A , Filippatos G et al. .; ESC Committee for Practice Guidelines (CPG) . ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society Of Intensive Care Medicine (ESICM) . Eur J Heart Fail 2008 ; 10 ( 10 ): 933 – 989 .
Google Scholar
McDonagh T A , Blue L , Clark A L et al. .; Heart Failure Association Committee on Patient Care . European Society of Cardiology Heart Failure Association standards for delivering heart failure care . Eur J Heart Fail 2011 ; 13 ( 3 ): 235 – 241 .
Patel H , Shafazand M , Ekman I et al. . Home care as an option in worsening chronic heart failure – a pilot study to evaluate feasibility, quality adjusted life years and cost-effectiveness . Eur J Heart Fail 2008 ; 10 ( 7 ): 675 – 681 .
Morcillo C , Valderas J M , Aguado O et al. . Evaluation of a home-based intervention in heart failure patients. Results of a randomized study . Rev Esp Cardiol 2005 ; 58 ( 6 ): 618 – 625 .
Martensson J , Dahlstrom U , Johansson G et al. .; Heart Failure Working Group of the Swedish Society of Cardiology . Nurse-led heart failure follow-up in primary care in Sweden . Eur J Cardiovasc Nurs 2009 ; 8 ( 2 ): 119 – 124 .
Martensson J , Stromberg A , Dahlstrom U et al. . Patients with heart failure in primary health care: effects of a nurse-led intervention on health-related quality of life and depression . Eur J Heart Fail 2005 ; 7 ( 3 ): 393 – 403 .
Jaarsma T , Stromberg A , De Geest S et al. . Heart failure management programmes in Europe . Eur J Cardiovasc Nurs 2006 ; 5 ( 3 ): 197 – 205 .
McAlister F A , Stewart S , Ferrua S et al. . Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials . J Am Coll Cardiol 2004 ; 44 ( 4 ): 810 – 819 .
Jaarsma T , van der Wal M H , Lesman-Leegte I et al. .; Coordinating Study Evaluating Outcomes of Advising and Counseling in Heart Failure (COACH) Investigators . Effect of moderate or intensive disease management program on outcome in patients with heart failure: coordinating study evaluating outcomes of advising and counseling in heart failure (COACH) . Arch Intern Med 2008 ; 168 ( 3 ): 316 – 324 .
Blue L , Lang E , McMurray J et al. . Randomized controlled trial of specialist nurse intervention in heart failure . BMJ 2001 ; 323 ( 7315 ): 715 – 718 .
Stewart S , Horowitz J D . Home-based intervention in congestive heart failure: long-term implications on readmission and survival . Circulation 2002 ; 105 ( 24 ): 2861 – 2866 .
Vilaseca J , Dedeu T , de Graaf P et al. . Chronic heart failure: the role of primary care – position paper of the European Forum for Primary Care . Qual Prim Care 2008 ; 16 ( 5 ): 351 – 362 .
Yu D S , Thompson D R , Lee D T . Disease management programmes for older people with heart failure: crucial characteristics which improve post-discharge outcomes . Eur Heart J 2006 ; 27 ( 5 ): 596 – 612 .
Brotons C , Falces C , Alegre J et al. . Randomized clinical trial of the effectiveness of a home-based intervention in patients with heart failure: the IC-DOM study . Rev Esp Cardiol 2009 ; 62 ( 4 ): 400 – 408 .
Del Sindaco D , Pulignano G , Minardi G et al. . Two-year outcome of a prospective, controlled study of a disease management programme for elderly patients with heart failure . J Cardiovasc Med 2007 ; 8 ( 5 ): 324 – 329 .
Peters-Klimm F , Campbell S , Herman K et al. .; Failure CNH. Case management for patients with chronic systolic heart failure in primary care: the HICMan exploratory randomised controlled trial . Trials 2010 ; 11 : 56 .
Piotrowicz E , Baranowski R , Bilinska M et al. . A new model of home-based telemonitored cardiac rehabilitation in patients with heart failure: effectiveness, quality of life, and adherence . Eur J Heart Fail 2010 ; 12 ( 2 ): 164 – 171 .
Aimonino N , Tibaldi V , Barale S et al. . Depressive symptoms and quality of life in elderly patients with exacerbation of chronic obstructive pulmonary disease or cardiac heart failure: preliminary data of a randomized controlled trial . Arch Gerontol Geriatric 2007 ; 44 ( 1 ): 7 – 12 .
Naylor M D , Brooten D A , Campbell R L et al. . Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial . J Am Geriatr Soc 2004 ; 52 ( 5 ): 675 – 684 .
Stewart S , Marley J E , Horowitz J D . Effects of a multidisciplinary, home-based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled study . Lancet 1999 ; 354 ( 9184 ): 1077 – 1083 .
Wierzchowiecki M , Poprawski K , Nowicka A et al. . A new programme of multidisciplinary care for patients with heart failure in Poznań: one-year follow-up . Kardiol Pol 2006 ; 64 ( 10 ): 1063 – 1070 .
Bowles K H , Holland D E , Horowitz D A . A comparison of in-person home care, home care with telephone contact and home care with telemonitoring for disease management . J Telemed Telecare 2009 ; 15 ( 7 ): 344 – 350 .
Pearson S , Inglis S C , McLennan S N et al. . Prolonged effects of a home-based intervention in patients with chronic illness . Arch Intern Med 2006 ; 166 ( 6 ): 645 – 650 .
Holland R , Brooksby I , Lenaghan E et al. . Effectiveness of visits from community pharmacists for patients with heart failure: HeartMed randomised controlled trial . BMJ 2007 ; 334 ( 7603 ): 1098 .
Triller D M , Hamilton R A . Effect of pharmaceutical care services on outcomes for home care patients with heart failure . Am J Health Syst Pharm 2007 ; 64 ( 21 ): 2244 – 2249 .
Soran O Z , Pina I L , Lamas G A et al. . A randomized clinical trial of the clinical effects of enhanced heart failure monitoring using a computer-based telephonic monitoring system in older minorities and women . J Card Fail 2008 ; 14 ( 9 ): 711 – 717 .
Wongpiriyayothar A , Pothiban L , Liehr P et al. . Effects of home-based care program on symptom alleviation and well-being among persons with chronic heart failure . Thai J Nurs Res 2008 ; 12 ( 1 ): 25 – 39 .
Vavouranakis I , Lambrogiannakis E , Markakis G et al. . Effect of home-based intervention on hospital readmission and quality of life in middle-aged patients with severe congestive heart failure: a 12-month follow up study . Eur J Cardiovasc Nurs 2003 ; 2 ( 2 ): 105 – 111 .
Feldman P H , Peng T R , Murtaugh C M et al. . A randomized intervention to improve heart failure outcomes in community-based home health care . Home Health Care Serv Q 2004 ; 23 ( 1 ): 1 – 23 .
Adams C E , Wilson M . Enhanced quality through outcome-focused standardized care plans . J Nurs Adm 1995 ; 25 ( 9 ): 27 – 34 .
Aguado O , Morcillo C , Delas J et al. . Long-term implications of a single home-based educational intervention in patients with heart failure . Heart Lung 2010 ; 39 ( 6 ): S14 – S22 .
Aiken L S , Butner J , Lockhart C A et al. . Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill . J Palliative Med 2006 ; 9 ( 1 ): 111 – 126 .
Antonicelli R , Testarmata P , Spazzafumo L et al. . Impact of telemonitoring at home on the management of elderly patients with congestive heart failure . J Telemed Telecare 2008 ; 14 ( 6 ): 300 – 305 .
Benatar D , Bondmass M , Ghitelman J et al. . Outcomes of chronic heart failure . Arch Intern Med 2003 ; 163 ( 3 ): 347 – 352 .
Burton L C , Leff B , Harper M et al. . Acceptability to patients of a home hospital . J Am Geriatr Soc 1998 ; 46 ( 5 ): 605 – 609 .
Chaudhry S I , Mattera J A , Curtis J P et al. . Telemonitoring in patients with heart failure . N Engl J Med 2010 ; 363 ( 24 ): 2301 – 2309 .
Cleland J G , Louis A A , Rigby A S et al. .; TEN-HMS Investigators. Noninvasive home telemonitoring for patients with heart failure at high risk of recurrent admission and death: the Trans-European Network-Home-Care Management System (TEN-HMS) study . J Am Coll Cardiol 2005 ; 45 ( 10 ): 1654 – 1664 .
Dar O , Riley J , Chapman C et al. . A randomized trial of home telemonitoring in a typical elderly heart failure population in north west London: results of the Home-HF study . Eur J Heart Fail 2009 ; 11 ( 3 ): 319 – 325 .
Duffy J R , Hoskins L M , Dudley-Brown S . Development and testing of a caring-based intervention for older adults with heart failure . J Cardiovasc Nurs 2005 ; 20 ( 5 ): 325 – 333 .
Feldman P H , Murtaugh C M , Pezzin L E et al. . Just-in-time evidence-based e-mail ‘reminders’ in home health care: impact on patient outcomes . Health Serv Res 2005 ; 40 ( 3 ): 865 – 885 .
Giordano A , Scalvini S , Zanelli E et al. . Multicenter randomised trial on home-based telemanagement to prevent hospital readmission of patients with chronic heart failure . Int J Cardiol 2009 ; 131 ( 2 ): 192 – 199 .
Goldberg L R , Piette J D , Walsh M N et al. . Randomized trial of a daily electronic home monitoring system in patients with advanced heart failure: the Weight Monitoring in Heart Failure (WHARF) trial . Am Heart J 2003 ; 146 ( 4 ): 705 – 712 .
Harrison M B , Browne G B , Roberts J et al. . Quality of life of individuals with heart failure: a randomized trial of the effectiveness of two models of hospital-to-home transition . Med Care 2002 04; 40 ( 4 ): 271 – 282 .
Heidenreich P A , Ruggerio C M , Massie B M . Effect of a home monitoring system on hospitalization and resource use for patients with heart failure . Am Heart J 1999 ; 138 ( 4 ): 633 – 640 .
Ho Y L , Hsu T P , Chen C P et al. . Improved cost-effectiveness for management of chronic heart failure by combined home-based intervention with clinical nursing specialists . J Formos Med Assoc 2007 ; 106 ( 4 ): 313 – 319 .
Jerant A F , Azari R , Nesbitt T S . Reducing the cost of frequent hospital admissions for congestive heart failure: a randomized trial of a home telecare intervention . Med Care 2001 ; 39 ( 11 ): 1234 – 1245 .
Dansky K , Vasey J . Managing heart failure patients after formal homecare . Telemed J E Health 2009 ; 15 ( 10 ): 983 – 991 .
Noel H C , Vogel D C , Erdos J J et al. . Home telehealth reduces healthcare costs . Telemed J E Health 2004 ; 10 ( 2 ): 170 – 183 .
Robinson S , Stroetmann K , Stroetmann V . Tele-homecare for chronically-ill patients: improved outcomes and new developments . J Inform Techn Healthcare 2004 ; 2 ( 4 ): 251 – 262 .
Jaarsma T , Halfens R , Huijer Abu-Saad H et al. . Effects of education and support on self-care and resource utilization in patients with heart failure . Eur Heart J 1999 ; 20 ( 9 ): 673 – 682 .
Weinberger M , Oddone E Z , Henderson W G . Does increased access to primary care reduce hospital readmissions? N Engl J Med 1996 ; 334 ( 22 ): 1441 – 1447 .
Myers S , Grant R W , Lugn N E et al. . Impact of home-based monitoring on the care of patients with congestive heart failure . Home Health Care Manage Pract 2006 10; 18 ( 6 ): 444 – 451 .
Rich M W , Beckham V , Wittenberg C et al. . A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure . N Engl J Med 1995 ; 333 ( 18 ): 1190 – 1195 .
West J A , Miller N H , Parker K M et al. . A comprehensive management system for heart failure improves clinical outcomes and reduces medical resource utilization . Am J Cardiol 1997 ; 79 ( 1 ): 58 – 63 .
Wright S P , Walsh H , Ingley K M et al. . Uptake of self-management strategies in a heart failure management programme . Eur J Heart Fail 2003 ; 5 ( 3 ): 371 – 380 .
Schofield R S , Kline S E , Schmalfuss C M et al. . Early outcomes of a care coordination-enhanced telehome care program for elderly veterans with chronic heart failure . Telemed J E Health 2005 ; 11 ( 1 ): 20 – 27 .
Kwok T , Lee J , Woo J et al. . A randomized controlled trial of a community nurse-supported hospital discharge programme in older patients with chronic heart failure . J Clin Nurs 2008 ; 17 ( 1 ): 109 – 117 .
Weintraub A , Gregory D , Patel A R et al. . A multicenter randomized controlled evaluation of automated home monitoring and telephonic disease management in patients recently hospitalized for congestive heart failure: the SPAN-CHF II trial . J Card Fail 2010 ; 16 ( 4 ): 285 – 292 .
Stewart S , Pearson S , Horowitz J D . Effects of a home-based intervention among patients with congestive heart failure discharged from acute hospital care . Arch Intern Med 1998 ; 158 ( 10 ): 1067 – 1072 .
Thompson D R , Roebuck A , Stewart S . Effects of a nurse-led, clinic and home-based intervention on recurrent hospital use in chronic heart failure . Eur J Heart Fail 2005 ; 7 ( 3 ): 377 – 384 .
Jerant A , Kravitz R , Moore-Hill M et al. . Depressive symptoms moderated the effect of chronic illness self-management training on self-efficacy . Med Care 2008 ; 46 ( 5 ): 523 – 531 .
Johnston B , Wheeler L , Deuser J et al. . Outcomes of the Kaiser Permanente Tele-Home Health Research Project . Arch Fam Med 2000 ; 9 ( 1 ): 40 – 45 .
Finkelstein S M , Speedie S M , Demiris G et al. . Telehomecare: quality, perception, satisfaction . Telemed J E Health 2004 ; 10 ( 2 ): 122 – 128 .
Scott L D , Setter-Kline K , Britton A S . The effects of nursing interventions to enhance mental health and quality of life among individuals with heart failure . Appl Nurs Res 2004 ; 17 ( 4 ): 248 – 256 .
Rondinini L , Coceani M , Borelli G et al. . Survival and hospitalization in a nurse-led domiciliary intervention for elderly heart failure patients . J Cardiovasc Med 2008 ; 9 ( 5 ): 470 – 475 .
Gary R A , Dunbar S B , Higgins M K et al. . Combined exercise and cognitive behavioral therapy improves outcomes in patients with heart failure . J Psychosom Res 2010 ; 69 ( 2 ): 119 – 131 .
Balk A H , Davidse W , Dommelen P et al. . Tele-guidance of chronic heart failure patients enhances knowledge about the disease. A multi-centre, randomised controlled study . Eur J Heart Fail 2008 ; 10 ( 11 ): 1136 – 1142 .
Bowles K H , Riegel B , Weiner M G et al. . The effect of telehomecare on heart failure self care . AMIA Annu Symp Proc 2010 ; 2010 : 71 – 75 .
Dansky K H , Vasey J , Bowles K . Impact of telehealth on clinical outcomes in patients with heart failure . Clin Nurs Res 2008 ; 17 ( 3 ): 182 – 199 .
Konstam V , Gregory D , Chen J et al. . Health-related quality of life in a multicenter randomized controlled comparison of telephonic disease management and automated home monitoring in patients recently hospitalized with heart failure: SPAN-CHF II trial . J Card Fail 2011 ; 17 ( 2 ): 151 – 157 .
Leff B , Burton L , Mader S L et al. . Hospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients . Ann Intern Med 2005 ; 143 ( 11 ): 798 – 808 .
Mader S L , Medcraft M C , Joseph C et al. . Program at home: a veterans affairs healthcare program to deliver hospital care in the home . J Am Geriatr Soc 2008 ; 56 ( 12 ): 2317 – 2322 .
Whitten P , Mickus M . Home telecare for COPD/CHF patients: outcomes and perceptions . J Telemed Telecare 2007 ; 13 ( 2 ): 69 – 73 .
Woodend A K , Sherrard H , Fraser M et al. . Telehome monitoring in patients with cardiac disease who are at high risk of readmission . Heart Lung 2008 ; 37 ( 1 ): 36 – 45 .
Mendoza H , Martin M J , Garcia A et al. . ‘Hospital at home’ care model as an effective alternative in the management of decompensated chronic heart failure . Eur J Heart Fail 2009 ; 11 ( 12 ): 1208 – 1213 .
LaFramboise L M , Woster J , Yager A et al. . A technological life buoy: patient perceptions of the health buddy . J Cardiovasc Nurs 2009 ; 24 ( 3 ): 216 – 224 .
Wakefield B J , Ward M M , Holman J E et al. . Evaluation of home telehealth following hospitalization for heart failure: a randomized trial . Telemed J E Health 2008 ; 14 ( 8 ): 753 – 761 .
Chen Y H , Ho Y L , Huang H C et al. . Assessment of the clinical outcomes and cost-effectiveness of the management of systolic heart failure in Chinese patients using a home-based intervention . J Int Med Res 2010 ; 38 ( 1 ): 242 – 252 .
Kornowski R , Zeeli D , Averbuch M et al. . Intensive home-care surveillance prevents hospitalization and improves morbidity rates among elderly patients with severe congestive heart failure . Am Heart J 1995 ; 129 ( 4 ): 762 – 766 .
Mortara A , Pinna G D , Johnson P et al. . A multi-country randomised trial of the role of a new telemonitoring system in CHF: the HHH study (home or hospital in heart failure). rational, study design and protocol . Eur Heart J Suppl 2004 ; 6 ( 6 ): F99 – F102 .
Hughes S L , Weaver F M , Giobbie-Hurder A et al. . Effectiveness of team-managed home-based primary care: a randomized multicenter trial . JAMA 2000 ; 284 ( 22 ): 2877 – 2885 .
Piette J D , Gregor M A , Share D et al. . Improving heart failure self-management support by actively engaging out-of-home caregivers: results of a feasibility study . Congest Heart Fail 2008 ; 14 ( 1 ): 12 – 18 .
Gonseth J , Guallar-Castillon P , Banegas J R et al. . The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-amalysis of published reports . Eur Heart J 2004 ; 25 ( 18 ): 1570 – 1595 .
Inglis S C , Clark R A , McAllister F A et al. . Structured telephone support or telemonitoring programmes for patients with chronic heart failure . Eur J Heart Fail 2011 ; 13 ( 9 ): 1028 – 1040 .
Phillips C O , Singa R M , Rubin H R et al. . Complexity of program and clinical outcomes of heart failure disease management incorporating specialist nurse-led heart failure clinics: a meta-regression analysis . Eur J Heart Fail 2005 ; 7 ( 3 ): 333 – 341 .
Roccaforte R , Demers C , Baldassarre F et al. . Effectiveness of comprehensive disease management programmes in improving clinical outcomes in heart failure patients. A meta-analysis . Eur J Heart Fail 2005 ; 7 ( 7 ): 1133 – 1144 .
Stewart S , Carrington M J , Marwick T et al. .; Which Heart failure Intervention is most Cost-effective & consumer friendly in reducing Hospital care trial Investigators . The WHICH? trial: rationale and design of a pragmatic randomized, multicentre comparison of home- vs. clinic-based management of chronic heart failure patients . Eur J Heart Fail 2011 ; 13 : 909 – 916 .
Jaarsma T , Luttik M L . Home Care in heart failure: towards an integrated care model . Eur J Heart Fail 2011 ; 13 ( 8 ): 823 – 824 .
Inglis S C , Clark R A , McAlister F A et al. . Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: abridged Cochrane Review . Eur J Heart Fail 2011 : 13 : 1028 – 1040 .
de Vries A E , van der Wal M H , Bedijn W et al. . Follow-up and treatment of an instable patient with heart failure using telemonitoring and a computerised disease management system: a case report . Eur J Cardiovasc Nurs 2011 (epub ahead of print).
Domingo M , Lupón J , González B et al. . Evaluation of a telemedicine system for heart failure patients: feasibility, acceptance rate, satisfaction and changes in patient behavior. Results from the CARME (CAtalan Remote Management Evaluation) study . Eur J Cardiovasc Nurs 2011 (epub ahead of print).
Luttik M L , Jaarsma T , Veeger N et al. . Marital status, quality of life, and clinical outcome in patients with heart failure . Heart Lung 2006 ; 35 ( 1 ): 3 – 8 .
- heart failure
- continuity of patient care
- home care services
- patient care team
- primary health care
- interdisciplinary treatment approach
- titration method
Email alerts
More on this topic, related articles in pubmed, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Components of heart failure management in home care : A literature review
Journal article
https://acuresearchbank.acu.edu.au/item/8v673/components-of-heart-failure-management-in-home-care-a-literature-review
Restricted files
Publisher's version, related outputs.
Development and testing of an instrument to measure contextual factors influencing self-care decisions among adults with chronic illness
Symptom recognition as a mediator in the self-care of chronic illness
Self-care management of bothersome symptoms as recommended by clinicians for patients with a chronic condition : A Delphi study
The effectiveness of self-care interventions in chronic illness : A meta-analysis of randomized controlled trials
Operational definition of self-care interventions for adults with chronic illness [editorial].
Characteristics of self-care interventions for patients with a chronic condition : A scoping review
Self-care research : Where are we now? Where are we going?
Self-care of heart failure patients : practical management recommendations from the heart failure association of the european society of cardiology.
Self-care research : How to grow the evidence base? (reprint)
Cross-cultural assessment of the self-care of chronic illness inventory : a psychometric evaluation.
Status of theory use in self-care research
Self-Care interventions that reduce hospital readmissions in patients with heart failure; Towards the identification of change agents
Development of an instrument for measuring self-care behaviors after left ventricular assist device implantation.
Patients with heart failure with and without a history of stroke in the Netherlands : A secondary analysis of psychosocial, behavioural and clinical outcomes up to three years from the COACH trial
Integrating symptoms into the middle-range theory of self-care of chronic illness
Effectiveness of the European Society of Cardiology/Heart Failure Association website ‘heartfailurematters.org’ and an e-health adjusted care pathway in patients with stable heart failure: Results of the ‘e-Vita HF’ randomized controlled trial
Health care professionals’ perceptions of home telemonitoring in heart failure care: Cross-sectional survey
Development and validation of a questionnaire to measure patient's experiences of health care in pulmonary arterial hypertension outpatient clinics, self-reported health and quality of life outcomes of heart failure patients in the aftermath of a national economic crisis: a cross-sectional study.
Stratified treatment recommendation or one-size-fits-all? A health economic insight based on graphical exploration
The associations between psychological distress and healthcare use in patients with non-cardiac chest pain: does a history of cardiac disease matter, development and psychometric evaluation of the thirst distress scale for patients with heart failure, nursing research in heart failure care: a position statement of the american association of heart failure nurses (aahfn), patient and professional factors that impact the perceived likelihood and confidence of healthcare professionals to discuss implantable cardioverter defibrillator deactivation in advanced heart failure: results from an international factorial survey.
Participants' experiences of a sexual counseling intervention during cardiac rehabilitation: A nested qualitative study within the CHARMS Pilot Randomized Controlled Trial
The CHARMS pilot study: A multi-method assessment of the feasibility of a sexual counselling implementation intervention in cardiac rehabilitation in Ireland
Exercise training in patients with ventricular assist devices: a review of the evidence and practical advice. a position paper from the committee on exercise physiology and training and the committee of advances heart failure of the heart failure association of the european society of cardiology.
Patient experiences of web-based cognitive behavioral therapy for heart failure and depression: Qualitative Study
Using co-design to develop an intervention to improve communication about the heart failure trajectory and end-of-life care
Development and initial testing of the self-care of chronic illness inventory, n-terminal pro-b-type natriuretic peptide and prognosis in caucasian vs. asian patients with heart failure, optimism and quality of life in patients with heart failure, relationships between exercise capacity and anxiety, depression, and cognition in patients with heart failure, quality of life of family caregivers of patients with a left ventricular assist device in japan.
Patient empowerment and general self-efficacy in patients with coronary heart disease: A cross-sectional study
Patterns of self-care and clinical events in a cohort of adults with heart failure: 1 year follow-up.
The dynamics of self-care in the course of heart failure management: Data from the IN TOUCH study
Trajectory of thirst intensity and distress from admission to 4-weeks follow up at home in patients with heart failure
"not getting worse" a qualitative study of patients perceptions of treatment goals in patients with heart failure, translation and psychometric evaluation of the dutch families importance in nursing care: nurses' attitudes scale based on the generalized partial credit model.
A comparison of the prognostic value of BNP versus NT-proBNP after hospitalisation for heart failure
Theory of self-care of chronic illness, variables related to communication about prognosis between nurses and patients at heart failure clinics in sweden and the netherlands, talking about palliative care in heart failure, "i was told that i would not die from heart failure": patient perceptions of prognosis communication.
Continuity and utilization of health and community care in elderly patients with heart failure before and after hospitalization
Association between sexual problems and relationship satisfaction among people with cardiovascular disease, factors related to self-care behaviours in heart failure: a systematic review of european heart failure self-care behaviour scale studies.
Dialogues between nurses, patients with heart failure and their partners during a dyadic psychoeducational intervention: A qualitative study
Sexual function of patients with heart failure: facts and numbers
Development of an international comorbidity education framework, 'heartfailurematters.org', an educational website for patients and carers from the heart failure association of the european society of cardiology: objectives, use and future directions, biomarker profiles in heart failure patients with preserved and reduced ejection fraction.
Serum potassium levels and outcome in acute heart failure (data from the PROTECT and COACH trials)
Reporting on self-care in research studies: guidance to improve knowledge building.
Low circulating microRNA levels in heart failure patients are associated with atherosclerotic disease and cardiovascular-related rehospitalizations
Patterns of self-care in adults with heart failure and their associations with sociodemographic and clinical characteristics, quality of life, and hospitalizations: a cluster analysis, attitudes of nurses towards family involvement in the care for patients with cardiovascular diseases, development, usability, and efficacy of a serious game to help patients learn about pain management after surgery: an evaluation study, heart failure with reduced ejection fraction.
Aspects of family caregiving as addressed in planned discussions between nurses, patients with chronic diseases and family caregivers: a qualitative content analysis
Exergaming through the eyes of patients with heart failure: a qualitative content analysis study.
Representativeness of participants in heart failure e-health trials: a report from the e-vita hf study, the efficacy of a supervised exercise training programme on readmission rates in patients with myocardial ischemia: results from a randomised controlled trial, factors related to self-care in heart failure patients according to the middle-range theory of self-care of chronic illness: a literature update, euroheartcare 2017.
Interpretability of the European heart failure self-care behaviour scale
Psychometric validation of the heart failure caregiver questionnaire (hf-cq), long-term effects of a dyadic psycho-educational intervention on caregiver burden and morbidity in partners of patients with heart failure: a randomized controlled trial, heart failure patients' future expectations and their association with disease severity, quality of life, depressive symptoms and clinical outcomes, high-grade carotid artery stenosis: a forgotten area in cardiovascular risk management, guía esc 2016 sobre el diagnóstico y tratamiento de la insuficiencia cardiaca aguda y crónica, fluid restriction in patients with heart failure: how should we think, vragen naar de onbekende weg (sexual history-taking in medical practice: the elephant in the room}).
The effect of guided web-based cognitive behavioral therapy on patients with depressive symptoms and heart failure: A pilot randomized controlled trial
Telerehabilitation in heart failure patients: the evidence and the pitfalls.
The value of telemonitoring and ICT-guided disease management in heart failure: Results from the IN TOUCH study
Sexual counselling for sexual problems in patients with cardiovascular disease, 2016 esc guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart gailure of the european society of cardiology (esc), self-management interventions: proposal and validation of a new operational definition.
Patients with heart failure with preserved ejection fraction and low levels of natriuretic peptides
Perceptions about traditional and novel methods to learn about postoperative pain management: a qualitative study, constipation in specialized palliative care: factors related to constipation when applying different definitions.
Sexual counselling for patients with cardiovascular disease: Protocol for a pilot study of the CHARMS sexual counselling intervention
Long-term evaluation of the ambulatory geriatric assessment: a frailty intervention trial (age-fit): clinical outcomes and total costs after 36 months, depressive symptoms, cardiac anxiety, and fear of body sensations in patients with non-cardiac chest pain, and their relation to healthcare-seeking behavior: a cross-sectional study, changing needs of heart failure patients and their families during the illness trajectory: a challenge for health care, symptom trajectory and symptom burden in older people with multimorbidity, secondary outcome from the rct age-fit study, the science committee of the council of cardiovascular nursing and allied professions: moving forward.
What are effective program characteristics of self-management interventions in patientswith heart failure? An individual patient data meta-analysis
Guided Internet-delivered cognitive behavioural therapy in patients with non-cardiac chest pain - A pilot randomized controlled study
Changes in thirst intensity during optimization of heart failure medical therapy by nurses at the outpatient clinic, sexual counseling in patients with heart failure: a silent phenomenon: results from a convergent parallel mixed method study, perception of impairments by patients with heart failure, how effective is an in-hospital heart failure self-care program in a japanese setting lessons from a randomized controlled pilot study.
Challenges in personalised management of chronic diseases-heart failure as prominent example to advance the care process
Continuous-time semi-markov models in health economic decision making: an illustrative example in heart failure disease management, sleep disordered breathing, hypoxia and inflammation : associations with sickness behaviour in community dwelling elderly with and without cardiovascular disease, constipation in specialized palliative care : prevalence, definition, and patient-perceived symptom distress, effectiveness of an interactive platform, and the esc/hfa heartfailurematters.org website in patients with heart failure: design of the multicentre randomized e-vita heart failure trial, extrahf survey: the first european survey on implementation of exercise training in heart failure patients, the course of sleep problems in patients with heart failure and associations to rehospitalizations, biomarkers and low risk in heart failure. data from coach and triumph, the challenge of multimorbidity in nurse education: an international perspective.
Physical activity in patients with heart failure: Barriers and motivations with special focus on sex differences
Increasing exercise capacity and quality of life of patients with heart failure through Wii gaming: The rationale, design and methodology of the HF-Wii study; A multicentre randomized controlled trial
Costs and effects of an ambulatory geriatric unit (the age-fit study) : a randomized controlled trial, adherence to self-care in patients with heart failure in the heartcycle study, struggling with issues about cardiopulmonary resuscitation (cpr) for end-stage heart failure patients, patient-nurse communication about prognosis and end-of-life care, caregiving tasks and caregiver burden : effects of an psycho-educational intervention in partners of patients withpost-operative heart failure, exercise programs for lvad supported patients: a snapshot from the esc affiliated countries.
Symptom burden in community-dwelling older people with multimorbidity: A cross-sectional study
The contribution of hypoxia to the association between sleep apnoea, insomnia, and cardiovascular mortality in community-dwelling elderly with and without cardiovascular disease.
Sexual counseling and cardiovascular disease: Practical approaches
Quality of life and influential factors in patients implanted with a left ventricular assist device, internet-based cognitive behavior therapy for patients with heart failure and depressive symptoms: a proof of concept study.
Long term follow-up after a randomized integrated educational and psychosocial intervention in patient-partner dyads affected by heart failure
Heart failure telemonitoring in japan and sweden: a cross-sectional survey, to adjust and endure: a qualitative study of symptom burden in older people with multimorbidity.
Knowledge expectations, self-care, and health complaints of heart failure patients scheduled for cardiac resynchronization therapy implantation
Improving care for patients with acute heart failure: Before, during and after hospitalization
Patient participation in patients with heart failure receiving structured home care:- A prospective longitudinal study
Towards tailoring of self-management for patients with chronic heart failure or chronic obstructive pulmonary disease : A protocol for an individual patient data meta-analysis
Prognostic value of n-terminal pro c-type natriuretic peptide in heart failure patients with preserved and reduced ejection fraction, sexual counseling is important in cardiovascular disease. returning to sexual activity is a common concern.
Sexrådgivning viktig vid kardiovaskulär sjukdom: Återgång till sexuell aktivitet ett vanligt problem [Sexual counseling is important in cardiovascular disease: Returning to sexual activity is a common concern]
Heart failure clinics are still useful (more than ever).
Exergaming to increase the exercise capacity and daily physical activity in heart failure patients: A pilot study
Exergaming in older adults : a scoping review and implementation potential for patients with heart failure, daily physical activity in stable heart failure patients, 20 things you didn't know about european cardiac nurses.
Prognostic value of plasma neutrophil gelatinase-associated lipocalin for mortality in patients with heart failure
Cross-cultural adaptation and reliability testing of polish adaptation of the european heart failure self-care behavior scale (ehfscbs), perceived caring needs in patient-partner dyads affected by heart failure : a qualitative study, sexual dysfunction in heart failure patients, sickness behavior in community-dwelling elderly : associations with impaired cardiac function and inflammation.
Fibrosis marker syndecan-1 and outcome in patients with heart failure with reduced and preserved ejection fraction
Sexual function in patients supported with left ventricular assist device and with heart transplant
Thirst trajectory and factors associated with persistent thirst in patients with heart failure, european cardiac nurses' current practice and knowledge on anticoagulation therapy, effect of spironolactone on 30-day death and heart failure rehospitalization (from the coach study), research in cardiovascular care : a position statement of the council on cardiovascular nursing & allied professionals of the european society of cardiology, 20 things you didn't know about sex and heart disease, characteristics associated with anxiety, depressive symptoms, and quality-of-life in a large cohort of implantable cardioverter defibrillator recipients.
Heart failure: Preventing disease and death worldwide
Zelfmanagement bij chronische ziekten, identification of symptom clusters among patients with heart failure : an international observational study.
Multidrug and optimal heart failure therapy prescribing in older general practice populations : A clinical data linkage study
Long-term follow-up in optimally treated and stable heart failure patients : primary care vs. heart failure clinic. results of the coach-2 study, communicating prognosis and end-of-life care to heart failure patients : a survey of heart failure nurses' perspectives, the european heart failure self-care behaviour scale : new insights into factorial structure, reliability, precision and scoring procedure.
A good manuscript review for the European Journal of Cardiovascular Nursing [Editorial]
Time-course of depressive symptoms in patients with heart failure+, guía de práctica clínica de la esh/esc para el manejo de la hipertensión arterial (2013), communicating about sexual concerns within cardiac health services : do service providers and service users agree, health professionals' expectations versus experiences of internet-based telemonitoring : survey among heart failure clinics.

The WAP four-disulfide core domain protein HE4 : A novel biomarker for heart failure
Wytyczne esh/esc dotyczace postepowania w nadcisnieniu tetniczym w 2013 roku, 2013 esh/esc guidelines for the management of arterial hypertension. the task force for the management of arterial hypertension of the european society of hypertension (esh) and of the european society of cardiology (esc), comparison of self-care behaviors of heart failure patients in 15 countries worldwide.
Perceived barriers of heart failure nurses and cardiologists in using clinical decision support systems in the treatment of heart failure patients
Thirst in heart failure : a systematic literature review, the charms study : cardiac patients' experiences of sexual problems following cardiac rehabilitation.
The CopenHeartSF trial - Comprehensive sexual rehabilitation programme for male patients with implantable cardioverter defibrillator or ischaemic heart disease and impaired sexual function : Protocol of a randomised clinical trial
Sexual counseling for individuals with cardiovascular disease and their partners: A consensus document from the american heart association and the esc council on cardiovascular nursing and allied professions (CCNAP)
Determinants of adherence to heart failure medication : a systematic literature review, preferences of heart failure patients in daily clinical practice : quality of life or longevity, neurohormonal and clinical sex differences in heart failure, validity and reliability of the european heart failure self-care behavior scale among adults from the united states with symptomatic heart failure.
B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction
The ambulatory geriatric assessment - a frailty intervention trial (age-fit) - a randomised controlled trial aimed to prevent hospital readmissions and functional deterioration in high risk older adults : a study protocol.
Randomized clinical trial to evaluate the effect of a supervised exercise training program on readmissions in patients with myocardial ischemia: A study protocol
Societal costs of non-cardiac chest pain compared with ischemic heart disease: A longitudinal study
Motivational factors for exercise in cardiac patients a literature review, quality of life and survival in patients with heart failure, design and methodology of the coach-2 (comparative study on guideline adherence and patient compliance in heart failure patients) study : hf clinics versus primary care is stable patients on optimal therapy, what keeps nurses from the sexual counseling of patients with heart failure, inflammation and anaemia in a broad spectrum of patients with heart failure, wytyczne esc dotycza ce rozpoznania oraz leczenia ostrej i przewlek ej niewydolno ci sierca na 2012 rok, validity and reliability of the german version of the 9-item european heart failure self-care behaviour scale, self-reported versus 'true' adherence in heart failure patients : a study using the medication event monitoring system, the coach risk engine : a multistate model for predicting survival and hospitalization in patients with heart failure, health-related quality of life and anemia in hospitalized patients with heart failure, association between prehospital delay and subsequent clinical course in patients with/hospitalized for heart failure, anaemia and iron deficiency in cardiac patients : what do nurses and allied professionals know, coping with adverse drug events in patients with heart failure : exploring the role of medication beliefs and perceptions, nurses' strategies to address self-care aspects related to medication adherence and symptom recognition in heart failure patients : an in-depth look, depressive symptoms and healthcare utilization in patients with noncardiac chest pain compared to patients with ischemic heart disease, sexual problems in elderly male and female patients with heart failure, perceived sexual difficulties and associated factors in patients with heart failure, the contribution of heart failure to sleep disturbances and depressive symptoms in older adults.
The effect of problem-based learning in patient education after an event of CORONARY heart disease - A randomised study in PRIMARY health care: Design and methodology of the COR-PRIM study
Esc guidelines for the diagnosis and treatment of acute and chronic heart failure 2012, long-term compliance with nonpharmacologic treatment of patients with heart failure, cross-cultural adaptation and validation of the european heart failure self-care behavior scale for brazilian portuguese, the role of advanced glycation end-products and their receptor on outcome in heart failure patients with preserved and reduced ejection fraction, determinants of heart failure self-care : a systematic literature review, quality of life is impaired similarly in heart failure patients with preserved and reduced ejection fraction, perceived adverse drug events in heart failure : patients' perception and related factors, clinical and prognostic effects of atrial fibrillation in heart failure patients with reduced and preserved left ventricular ejection fraction.
The value of INnovative ICT guided disease management combined with Telemonitoring in OUtpatient clinics for Chronic Heart failure patients. Design and methodology of the IN TOUCH study: A multicenter randomised trial
The global burden of cardiovascular disease, social support and self-care in heart failure, predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction, the body of knowledge on compliance in heart failure patients : we are not there yet, educational level and the quality of life of heart failure patients : a longitudinal study, depressive symptoms and inflammation in patients hospitalized for heart failure, psychometric properties of the chinese version of the european heart failure self-care behaviour scale, self-reported adverse drug events and the role of illness perception and medication beliefs in ambulatory heart failure patients : a cross-sectional survey, which interventions are used by health care professionals to enhance medication adherence in cardiovascular patients a survey of current clinical practice, factors associated with patient delay in seeking care after worsening symptoms in heart failure patients, self-care management of heart failure :practical recommendations from the patient care committee of the heart failure association of the european society of cardiology, the advisory brought to practice : routine screening on depression (and anxiety) in coronary heart disease; consequences and implications, vitamin d status and outcomes in heart failure patients, depression and the delay between symptom onset and hospitalization in heart failure patients, sexual counselling of cardiac patients in europe : culture matters, effective communication and ethical consent in decisions related to icds, lack of prognostic value of type d personality for mortality in a large sample of heart failure patients, heart failure patients monitored with telemedicine : patient satisfaction, a review of the literature, a physiotherapist-delivered, combined exercise and pain coping skills training intervention for individuals with knee osteoarthritis: a pilot study, what works in chronic care management: the case of heart failure, what do cardiovascular nurses know about the hematological management of eisenmenger syndrome, heart failure management programmes in europe, pharmacological treatment and perceived health status during 1- year follow-up in patients diagnosed with coronary artery disease, but in ineligible for revascularization. results from the euro heart survey on coronary revascularization, nurse specialists in adult congenital heart disease: the current status in europe, cardiovascular risk estimation by professionally active cardiovascular nurses: results from the basel 2005 nurses cohort.
Components of heart failure management in home care; a literature review
- Nursing Diagnostics
- Linköping University
- University of Groningen
Research output : Contribution to journal › Article › Academic › peer-review
- continuity of patient care
- heart failure
- home care services
- patient care team
- patient education as topic
Access to Document
- 10.1177/1474515112449539
Fingerprint
- Literature Review Nursing and Health Professions 100%
- Home Care Nursing and Health Professions 100%
- Heart Failure Medicine and Dentistry 100%
- Patient Medicine and Dentistry 37%
- Practice Guideline Nursing and Health Professions 25%
- Primary Medical Care Nursing and Health Professions 25%
- Primary Health Care Medicine and Dentistry 25%
- Procedures Nursing and Health Professions 12%
T1 - Components of heart failure management in home care; a literature review
AU - Jaarsma, Tiny
AU - Brons, Maaike
AU - Kraai, Imke H.
AU - Luttik, Marie Louise
AU - Stromberg, Anna
PY - 2013/6
Y1 - 2013/6
N2 - Background: Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and secondary care. Although guidelines on optimal HF care exist, no specific description of components that are applied for optimal HF care at home exist. The objective of this review was to describe which components of HF (home) care are found in research studies addressing homecare interventions in the HF population. Methods: The Pubmed, Embase, Cinahl, and Cochrane databases were searched using HF-, homecare services-, and clinical trial-related search terms. Results: The literature search identified 703 potentially relevant publications, out of which 70 articles were included. All articles described interventions with two or more of the following components: multidisciplinary team, continuity of care and care plans, optimized treatment according to guidelines, educational and counselling of patients and caregivers, and increased accessibility to care. Most studies (n=65, 93%) tested interventions with three components or more and 20 studies (29%) used interventions including all five components. Conclusions: There a several studies on HF care at home, testing interventions with a variety in number of components. Comparing the results to current standards, aspects such as collaboration between primary care and hospital care, titration of medication, and patient education can be improved. © 2012 The European Society of Cardiology.
AB - Background: Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and secondary care. Although guidelines on optimal HF care exist, no specific description of components that are applied for optimal HF care at home exist. The objective of this review was to describe which components of HF (home) care are found in research studies addressing homecare interventions in the HF population. Methods: The Pubmed, Embase, Cinahl, and Cochrane databases were searched using HF-, homecare services-, and clinical trial-related search terms. Results: The literature search identified 703 potentially relevant publications, out of which 70 articles were included. All articles described interventions with two or more of the following components: multidisciplinary team, continuity of care and care plans, optimized treatment according to guidelines, educational and counselling of patients and caregivers, and increased accessibility to care. Most studies (n=65, 93%) tested interventions with three components or more and 20 studies (29%) used interventions including all five components. Conclusions: There a several studies on HF care at home, testing interventions with a variety in number of components. Comparing the results to current standards, aspects such as collaboration between primary care and hospital care, titration of medication, and patient education can be improved. © 2012 The European Society of Cardiology.
KW - continuity of patient care
KW - heart failure
KW - home care services
KW - humans
KW - patient care team
KW - patient education as topic
KW - hartverlamming
KW - thuiszorg
KW - patiëntenzorg
KW - patiëntenvoorlichting
KW - onderzoekshulp
U2 - 10.1177/1474515112449539
DO - 10.1177/1474515112449539
M3 - Article
C2 - 22707520
SN - 1474-5151
JO - European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology
JF - European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology
Digitala Vetenskapliga Arkivet
- CSV all metadata
- CSV all metadata version 2
- modern-language-association-8th-edition
- Other style
- Other locale
Jaarsma, Tiny
Brons, maaike, kraai, imke, luttik, marie louise, strömberg, anna, abstract [en].
BACKGROUND: Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and secondary care. Although guidelines on optimal HF care exist, no specific description of components that are applied for optimal HF care at home exist. The objective of this review was to describe which components of HF (home) care are found in research studies addressing homecare interventions in the HF population.
METHODS: The Pubmed, Embase, Cinahl, and Cochrane databases were searched using HF-, homecare services-, and clinical trial-related search terms.
RESULTS: The literature search identified 703 potentially relevant publications, out of which 70 articles were included. All articles described interventions with two or more of the following components: multidisciplinary team, continuity of care and care plans, optimized treatment according to guidelines, educational and counselling of patients and caregivers, and increased accessibility to care. Most studies (n=65, 93%) tested interventions with three components or more and 20 studies (29%) used interventions including all five components.
CONCLUSIONS: There a several studies on HF care at home, testing interventions with a variety in number of components. Comparing the results to current standards, aspects such as collaboration between primary care and hospital care, titration of medication, and patient education can be improved.
Place, publisher, year, edition, pages
Keywords [en], national category, identifiers, open access in diva, other links, search in diva, by author/editor, by organisation, in the same journal, on the subject, search outside of diva, altmetric score.
Practical guide on home health in heart failure patients
Affiliation.
- 1 Department of Social and Welfare Studies, Linköping University, Linköping, Sweden.
- PMID: 24250283
- PMCID: PMC3821536
- DOI: 10.5334/ijic.992
Introduction: Chronic heart failure is a common condition affecting up to 15 million people in the extended Europe. Heart failure is burdensome and costly for patients in terms of decreased quality of life and poor prognosis, and it is also costly for society. Better integrated care is warranted in this population and specialised heart failure care can save costs and improve the quality of care. However, only a few European countries have implemented specialised home care and offered this to a larger number of patients with heart failure.
Method: We developed a guide on Home Health in Heart Failure patients from a literature review, a survey of heart failure management programs, the opinion of researchers and practitioners, data from clinical trials and a reflection of an international expert meeting.
Results: IN INTEGRATED HOME CARE FOR HEART FAILURE PATIENTS, IT IS ADVISED TO CONSIDER THE FOLLOWING COMPONENTS: integrated multidisciplinary care, patient and partner participation, care plans with clear goals of care, patient education, self-care management, appropriate access to care and optimised treatment.
Discussion: We summarised the state of the art of home-based care for heart failure patients in Europe, described the typical content of such care to provide a guide for health care providers.
Keywords: heart failure; home care; integrated care; multidisciplinary.
- Open access
- Published: 06 May 2023
An evidence map of systematic reviews on models of outpatient care for patients with chronic heart diseases
- Madlen Hoerold ORCID: orcid.org/0000-0001-7673-3022 1 ,
- Heike Heytens 1 ,
- Carla Maria Debbeler 1 ,
- Saskia Ehrentreich 1 ,
- Thomas Rauwolf 2 ,
- Alexander Schmeißer 2 ,
- Marc Gottschalk 2 ,
- Eva Maria Bitzer 3 ,
- Ruediger C. Braun-Dullaeus 2 &
- Christian J. Apfelbacher 1
Systematic Reviews volume 12 , Article number: 80 ( 2023 ) Cite this article
1628 Accesses
10 Altmetric
Metrics details
Chronic heart disease affects millions of people worldwide and the prevalence is increasing. By now, there is an extensive literature on outpatient care of people with chronic heart disease. We aimed to systematically identify and map models of outpatient care for people with chronic heart disease in terms of the interventions included and the outcomes measured and reported to determine areas in need of further research.
We created an evidence map of published systematic reviews. PubMed, Cochrane Library (Wiley), Web of Science, and Scopus were searched to identify all relevant articles from January 2000 to June 2021 published in English or German language. From each included systematic review, we abstracted search dates, number and type of included studies, objectives, populations, interventions, and outcomes. Models of care were categorised into six approaches: cardiac rehabilitation, chronic disease management, home-based care, outpatient clinic, telemedicine, and transitional care. Intervention categories were developed inductively. Outcomes were mapped onto the taxonomy developed by the COMET initiative.
The systematic literature search identified 8043 potentially relevant publications on models of outpatient care for patients with chronic heart diseases. Finally, 47 systematic reviews met the inclusion criteria, covering 1206 primary studies (including double counting). We identified six different models of care and described which interventions were used and what outcomes were included to measure their effectiveness. Education-related and telemedicine interventions were described in more than 50% of the models of outpatient care. The most frequently used outcome domains were death and life impact.
Evidence on outpatient care for people with chronic heart diseases is broad. However, comparability is limited due to differences in interventions and outcome measures. Outpatient care for people with coronary heart disease and atrial fibrillation is a less well-studied area compared to heart failure. Our evidence mapping demonstrates the need for a core outcome set and further studies to examine the effects of models of outpatient care or different interventions with adjusted outcome parameters.
Systematic review registration
PROSPERO (CRD42020166330).
Peer Review reports
Chronic heart diseases (we consider heart failure, coronary heart disease, and atrial fibrillation) are complex clinical conditions associated with various symptoms and comorbidities such as dyspnea, fatigue, peripheral edema, and depression [ 1 , 2 ]. Coronary heart disease (CHD), heart valve disease, arrhythmias, familial cardiomyopathy, toxin‐induced cardiomyopathy, and hypertension are all linked to heart failure (HF) [ 1 ]. Reported estimates of heart failure incidence in European countries and the USA ranges widely from100/100,000 person-years, in French to 4300/100,000 person-years in a US study and strongly depends, on the population studied and the diagnostic criteria used [ 3 ]. Incidence increases with age and with ageing populations this means that prevalence is also on the increase [ 3 ]. At least 26 million people are affected worldwide [ 4 ]. Coronary heart disease is the leading cause of death in both developed and developing countries. Considering current lifestyles, the incidence of CHD will continue to rise [ 5 ]. Atrial fibrillation (AF) is the most prevalent arrhythmia managed in clinical practice and one of the leading causes of HF. The 2019 Global Burden of Disease Study showed that there were about 59.7 million individuals with atrial fibrillation/flutter worldwide [ 6 ]. The majority of patients with heart failure exhibit multi‐morbidity and the number of patients with three or more chronic comorbidities increased [ 7 ]. Comorbidity is associated with increased severity of HF symptoms and corresponds to a poor quality of life and a worse prognosis [ 8 ].
Patients with chronic HF increasingly receive outpatient care. However, they are frequently hospitalised for acute decompensated as well as non‐cardiovascular causes. Assessment of prognosis of heart failure is particularly challenging. The clinical course depends on the underlying pathomechanisms and varies depending on the severity of the disease. Outcomes are difficult to predict in individual patients. Even late in heart failure, patients still have periods of “good days” and apparent stability, which can lead them and their care providers into postponing vital decisions [ 9 ]. Therapeutic interventions in each disease stage aim to modify risk factors, treat risk and structural heart disease to prevent HF, and reduce symptoms, morbidity, and mortality [ 10 ]. Holistic management approaches must foster the implementation of multidisciplinary approaches to address major contributors to the persisting burden of HF including multimorbidity, ageing, and social determinants of health [ 11 ]. Heart failure treatment constitutes challenges related to both self-care and emotional burden. Many patients are struggling emotionally due to a lack of information and education, inadequate care coordination and troublesome medication and self-monitoring of symptoms. Doing so affects their self-care ability and their well-being as well as their quality of life [ 12 ].
There is a large body of literature on the care provided to people with chronic heart diseases. However, previous systematic reviews (SRs) have mainly focused on the effects of specific health services.
Model of care is an overarching design for the provision of a particular type of health care service that is shaped by a theoretical basis, evidence-based practice, and defined standards. It consists of defined core elements and principles and has a framework that provides the structure for the implementation and subsequent evaluation of care. Clearly defined models of care help to ensure that all health professionals are working towards common goals and, most importantly, to evaluate service on agreed outcome measures [ 13 ].
This evidence map [ 14 , 15 ] thus has an important purpose. We aimed to identify models of outpatient care (MoC) associated with chronic heart diseases in published systematic reviews (SRs), and to map which interventions built these models of care as well as the outcomes measured and reported. This will help to identify gaps and future research needs. A broad systematic review of primary studies was not feasible within a reasonable timescale. Hence, we decided to conduct an overview (evidence map) of systematic reviews. This approach [ 16 , 17 , 18 ] is increasingly used in research areas where the literature has already been summarised in several systematic reviews.
To identify any specific models of outpatient care for patients with chronic heart diseases, in systematic reviews, published in the English or German language.
Create a comprehensive overview (evidence map) of identified interventions and outcomes.
Protocol and registration
Our approach was guided by accepted methodological and reporting standards for overviews and mapping reviews [ 19 , 20 , 21 ] including PRISMA flow-chart (Fig. 1 ). We registered the review protocol on PROSPERO (CRD42020166330). We have not made any amendments to the information provided at registration. Our systematic mapping review focused on models of outpatient care.
Inclusion and exclusion criteria
In the protocol, we decided to include only published systematic reviews. We searched for English- and German-language human studies published since 2000. However, for pragmatic reasons we did not choose a larger period. We only included systematic reviews of models of care for people with chronic heart diseases (coronary heart disease, heart failure, and atrial fibrillation) in outpatient care that met the criteria of the Centre for Reviews and Dissemination (Database of Abstracts of Reviews of Effects, DARE) [ 22 ]. Initiation and delivery of interventions (models of care) were required to be linked to outpatient/primary care. Reviews with interventions for specific vulnerable groups (e.g. pregnant woman and palliative care) and infants (0–3 age) were excluded. All other study designs were excluded (Table 1 ).
Data sources and searches
The National Library of Medicine through PubMed, Cochrane Library (Wiley), Web of Science and Scopus were searched for systematic reviews published between January 1, 2000, and June, 30 2021. We used a combination of MeSH and text terms that included terms related to chronic heart diseases, models of care and outpatient care settings. A full search strategy is available in Additional file 1 : Search strategy at Pubmed. We used Citavi 6, a reference management software to manage our records and remove duplicates.
Eligibility screening process
Two groups of reviewers MH, HH and AS, TR—initial search until December 2019; MH, SE and HH, SE—search update, each screening 50% of total) independently screened titles and abstracts for eligibility based on the above selection criteria. All studies reviewed as “yes” or “unsure” by either reviewer team were included in full-text screening. Agreement between both reviewers was required to exclude a study. Where consensus of eligibility was not reached a third reviewer (CA) was consulted. We obtained full texts for all selected systematic reviews, and if study eligibility remained unclear, we discussed again with a third reviewer (CA).
Data extraction
Two groups of reviewers (MH, CD and HH, SE, each 100% of total) extracted data independently and subsequently reconciled. An Excel spreadsheet for data extraction was developed and piloted by the review team. From each systematic review search dates, objectives, populations, number and types of included studies, number of included participants, components of interventions, and outcomes reported were extracted and summarised.
Data analysis
We analysed the extracted data from the included SRs with descriptive statistics for reporting frequencies where appropriate. Temporal data were represented in visual graphs to illustrate trends. All other data were presented in tabular form. We inductively categorised MoC based on the titles and summaries of the included SRs. Intervention categories were formed by inductively coding the characteristics of the interventions in the SRs (content analysis) and jointly consented by the review group. We mapped the outcomes onto the taxonomy developed by the COMET initiative [ 23 ]. The COMET initiative encourage the development and uptake of core outcome sets: an agreed standard set of outcomes that should be measured and reported, as a minimum, in all clinical trials in specific areas of health or healthcare setting [ 24 ]. We categorised by the core areas: death, physiological or clinical, life impact, resource use and adverse events [ 23 ]. If an outcome was composite and addressed several core areas, we classified it within each of the relevant domains. All authors reached final consensus on findings, interpretation and text. We did not perform an assessment of the methodological quality of the included SRs.
To perform a comprehensive analysis of the overlap of the included SRs, we used the GROOVE tool and included all primary studies [ 25 ]. Besides the calculation of overall Corrected Covered Areas (CCA), GROOVE provides a graphical representation of the overlap among each pair of possible SRs (nodes). A CCA value lower than 5 can be considered as a slight overlap, whereas values greater than or equal to 15 can be considered as a very high overlap (0–5; slight, 6–10; moderate, 11–15; high, and > 15; very high overlap) [ 26 ].
Studies and study characteristics
After the removing of duplicates, 86 potentially eligible records were identified and screened according to the protocol. We excluded thirty-eight articles after full-text screening, because they did not meet the inclusion criteria; no model of care—21 articles [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ], no eligible population—ten articles [ 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 ], no eligible setting—4 articles [ 58 , 59 , 60 , 61 ], no SR—2 articles [ 62 , 63 ], no full text available—1 article [ 64 ]. Fourty-seven systematic reviews/48 publications, covering 1154 primary studies (including double counting) were included in this review (Fig. 1 ). Most systematic reviews included models of care for heart failure (42 SRs), in addition to coronary heart disease (4 SRs), and atrial fibrillation (1 SR).
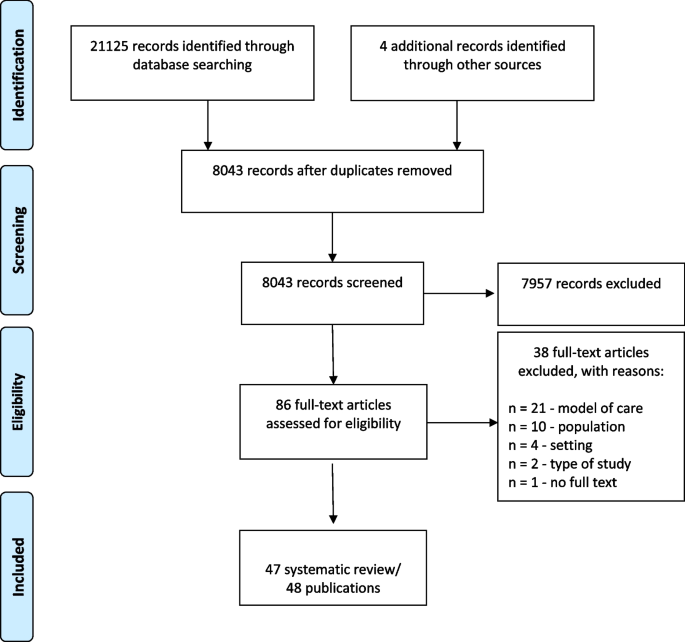
Prisma flow-chart
The number of publications on interventions for patients with chronic heart diseases in outpatient care has increased. While only 21.3% of the systematic reviews included here were published in 2000–2010, 55.3% were published since January 2016 (Fig. 2 ). The studies included in the SRs were conducted between 1967 and 2021.
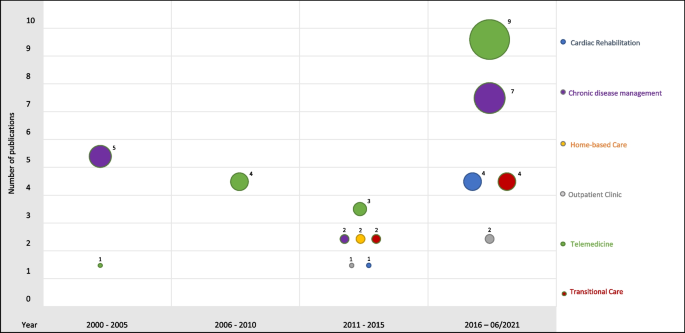
Evidence map — models of care
The authors of the included SRs performed a systematic search of at least two to a maximum of 16 databases to identify randomised controlled trials, non-randomised controlled trials or other relevant research articles to answer the research question. Twenty-one different databases were used for literature search in the included SRs. The number of included participants ranged from 867 to 28,455. The number of included studies ranged from 6 to 70 studies per systematic review (Additional file 2 : Characteristics of the included SRs).
The CCA in our overlap analysis was 3.08% (slight overlap) for all included systematic reviews. However, we measured a very high overlap (≥ 15%) at 111 of 1081 nodes and a high overlap (10–15%) at further 84 nodes. This means that a large number of studies appeared several times across the systematic reviews (Fig. 3 ). Five primary studies were included in 15 or more SRs (Table 2 ).
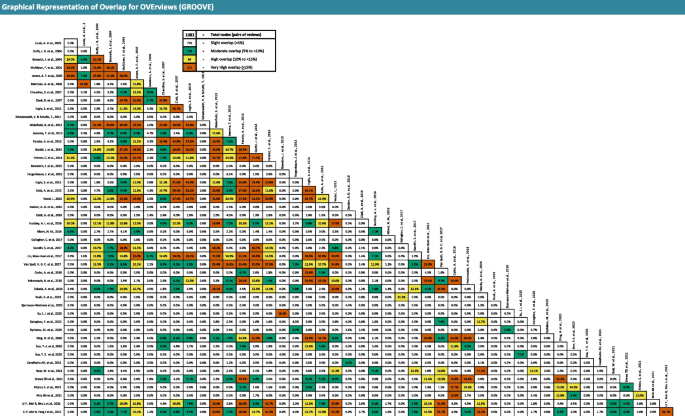
Graphical representation of overlap for overviews (GROOVE)
Evidence map on models of outpatient care
In our evidence mapping, we identified six models of outpatient care: (a) cardiac rehabilitation, (b) chronic disease management, (c) home-based care, (d) outpatient clinics, (e) telemedicine, and (f) transitional care.
We categorised MoCs interventions according to the following characteristics: remote monitoring of daily biometric data, structured telephone support, video conference, information/education program, symptom monitoring (by staff or patients), regular consultation (e.g. outpatient, hospital), home visits, pharmacologic management, nutrition, coordination, behavioural or psychosocial support, planning for discharge, and exercise, which has been visualised in Additional file 3 : Mapping of the single interventions of the included SRs. In addition, we mapped the primary outcomes of the included SRs onto the taxonomy developed by the COMET initiative [ 23 ] (Additional file 4 : Mapping of the primary outcomes of the included SRs). Outcomes from all core areas were used: in 30 SRs outcomes from the core areas death (65.2%) were included. Physical/clinical outcomes were included in 11 SRs (23.9%), life impact in 25 SRs (54.3%), resource use in 30 SRs (65.2%) and adverse events in 6 SRs (13%).
Cardiac rehabilitation
Cardiac rehabilitation (CR) was designed to optimise secondary prevention of chronic heart failure. It has evolved from an exercise-focused program to a comprehensive, multi-component model of care to address risk factors. Indeed, CR societies have published and internationally agreed so-called “core components” of CR, namely, nutritional counselling, risk factor modification, psychosocial management, patient education, and exercise training [ 65 ].
We included five SRs with heart failure and CHD indications for the MoC cardiac rehabilitation [ 66 , 67 , 68 , 69 , 70 ]. All included SRs on MoC reported exercise programs. In addition, four out of five included at least one telemonitoring intervention (remote monitoring of daily biometric data, structured telephone support, or video conference). Information/education programs and behavioural or psychosocial support were provided in 60% of the included SRs. One SR each described nutrition and home visits as interventions. Death and life impact are relevant outcomes for cardiac rehabilitation. All systematic reviews used outcomes of these core areas to evaluate interventions. Thus, four SRs employed psychological/clinical outcomes (80%), three SRs resource use outcomes (60%) and one SR adverse events outcomes (20%).
Chronic disease management
Definitions of chronic disease management (programs) vary substantially. We therefore included a wider range of approaches, which we considered as “chronic disease management”, e.g. case management [ 71 ], chronic care model [ 72 ], coordinated care and integrated care [ 73 ], and disease management programs [ 74 ]. Chronic disease management does not normally involve general coordination of care and preventive services such as flu vaccination [ 75 ].
The MoC chronic disease management included only SRs for people with heart failure [ 39 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 ]. The included SRs demonstrated three core elements: telemonitoring, coordination and information/education program. Telemonitoring interventions (at least one intervention) were part in 12 SRs (85.7%). Coordination and information/education programs were each included in 71% of SRs ( n = 10). In addition behavioural or psychosocial support (7; 50%), regular consultation (6; 43%), symptom monitoring (4; 29%), pharmacological management (4; 29%), and home visits (21%) were reported. Outcomes of the core areas death and resource use were reported in seven of the SRs (50%). Life impact outcomes were included in seven SRs (50%), psychological/clinical outcomes in three (21%) and adverse events outcomes in only two systematic reviews (14%).
Home-based care
Home-based care aims to improve health and prevent the need for long-term care or immediate care. It includes a variety of home services such as health promotion and teaching, clinical care, end-of-life care, rehabilitation, social adaptation and integration, and support for informal caregivers [ 89 ].
The MoC home-based care included only two SRs for people with heart failure [ 89 , 90 ]. One SR was based only on home visits. The second SR included also information/education, behavioural or psychosocial support, pharmacological management, and coordination interventions. All SRs included outcomes from the core area death. Further outcomes from the core areas life impact and resource use were used in one of the two SRs.
Outpatient clinic
Outpatient clinics (often located at hospitals) provide a collaborative, multidisciplinary approach for treatment with cardiologists, nurses, pharmacists, dieticians, psychologists, and social workers. These clinics not only provide optimisation of drug therapy, but also education regarding lifestyle such as diet and exercise, medication compliance and diuretic titration strategies; they serve as a crucial link for patients who develop worsening symptoms and require earlier follow-up or medication adjustment [ 91 ].
We included three SRs for the MoC [ 91 , 92 , 93 ], one SR each for of the indications heart failure, coronary heart disease and atrial fibrillation. For all indications, information/education and symptom monitoring are listed as interventions. In addition, the following interventions are described for heart failure: regular consultation, pharmacological management, nutrition, coordination, and behavioural or psychosocial support. There were fewer interventions for CHD and AF. In two of the three systematic reviews on outpatient clinics, outcomes from four core areas were used. Outcomes on resource use were included in all three SRs.
Telemedicine
Telemedicine (TM) is delivered by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research, and evaluation. In addition, TM is used for continuing education of health care providers, all in the interests of advancing the health of individuals and their communities [ 94 ].
The majority of SRs included in the MoC telemedicine [ 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 ] refer to heart failure. One SR investigated telemedicine MoC for people with CHD. All SRs ( n = 17) offered at least one telemonitoring intervention to their participants: remote monitoring of daily biometric data (16; 94%), structured telephone support (15; 88%) or video conference (2; 12%). In addition, the following interventions were reported in SRs: symptom monitoring (10; 59%), information/education (7; 41%), pharmacological management (5; 29%), behavioural or psychosocial support and home visits (3; 18%), coordination (2; 12%), exercise program and nutrition (1; 6%). Outcomes from four core areas were included in the TM SRs: death (13; 76%), psychological/clinical (2; 6%), life impact (9; 53%), and resource use (12; 71%). The majority of included telemedicine systematic reviews (12; 70.5%) considered outcomes from two core areas (death, ressource use).
Transitional care
Transitional care (TC) encompasses a broad range of services and environments designed to promote the safe and timely passage of patients between levels of health care and across care settings [ 112 ].
The MoC transitional care included six SRs for people with heart failure [ 113 , 114 , 115 , 116 , 117 , 118 ]. Four of the six included SRs reported at least one telemonitoring intervention. In addition, at least 50% of the SRs also described the following interventions: information/education, symptom monitoring, home visits, regular consultation, and coordination. Pharmacological management and behavioural or psychosocial support was only reported in one SR each. Outcomes from the core area death, life impact, and adverse events were included in two of these six SRs each.
We used evidence mapping of systematic reviews to summarise the complex and growing literature on outpatient care for people with chronic heart diseases. We identified six different models of outpatient care (cardiac rehabilitation, chronic disease management, home-based care, outpatient clinics, telemedicine, and transitional care) and described which interventions were used and what outcomes were included to measure their effectiveness. We observed heterogeneity in terms of interventions within as well as commonalities between MoCs. In addition, we identified populations that require further investigation and observed variation in how outcomes were measured. The total overlap between the SRs was calculated as slight. It seems that this effect is due to the diversity of the models of care. Nevertheless, a high and very high overlap was measured at a total of 195 of 1081 nodes, especially within the MoCs on chronic disease management, telemedicine and transitional care.
Due to the large inclusion time frame, we were able to give a broad overview. It is apparent that research and thus the number of publications has increased in the period examined. Fourty-two out of 47 included SRs were on heart failure. This also means that AF and CHD populations are significantly less studied.
Despite the observed heterogeneity in populations, our evidence map shows noteworthy trends. Systematic reviews on chronic disease management [ 39 , 76 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 ] and telemedicine [ 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 107 , 108 , 109 , 110 , 111 , 119 ] have been increasingly published. Telemedicine provides an opportunity to improve outpatient healthcare delivery. Inequalities in access to healthcare and in the provision of healthcare services, caused by difficulties in transportation and, in some cases, lack of healthcare workers, are particularly challenging in rural areas [ 120 ]. The evidence map show core elements of models of care combined with additional interventions. Especially, education-related and telemedicine interventions were described more than 50% of the MoCs. The details on how the interventions were implemented are described in varying detail. In addition, the interventions in the primary studies varied in terms of design, for example frequency of sessions, duration, and their providers. This has not been analysed in our study and needs further investigation.
It was remarkable that outcomes were used very heterogeneously in the SRs. Only few SRs measured psychological/clinical and adverse events outcomes. Rather, outcomes of the core areas death, life impacts, and resources are used. Up to the best of our knowledge, there is a lack of a core outcome set for studies on outpatient care of chronic heart disease. Defined and agreed upon outcomes and measurement tools would help to increase comparability of the effectiveness of interventions in primary studies and systematic reviews.
As visual representation, this evidence map summarise the evolving research on outpatient care for people with chronic heart diseases: We only used published systematic reviews for our overview and evidence mapping [ 18 ]. As not necessarily required for our objectives, we have not provide an assessment of the methodological quality of the reviews by available instruments such as AMSTAR-2 [ 121 ] or ROBIS [ 122 ], neither calculate effect sizes in a meta-analysis. We included only systematic reviews that met at least four of five DARE criteria for SR [ 22 ]—we relied on the skills of the authors of the included systematic reviews in conducting the literature search, conducting and assessing study quality, selecting and presenting results.
In an ever-evolving research environment on outpatient care for people with chronic heart diseases, summarising research evidence on models of outpatient care and interventions is becoming increasingly complex, especially for healthcare stakeholders. Our evidence map can help bridge the gap between the available scientific evidence on outpatient care for people with chronic heart diseases and the adoption of this evidence by health systems with an overview of systematic reviews from January 1, 2000, to June 30, 2021, on models of outpatient care.
In addition, evidence maps are also a useful tool to identify gaps in the literature, and to guide future research. Our results show that the comparability of published SRs on MoC is limited due to differences in interventions and outcome measures. For example, physical/clinical outcomes are less considered in SRs. Outpatient care of CHD and AF is poorly studied compared to HF. Thus our evidence map determines the need for primary or secondary research. First of all, it would be helpful to develop a core outcome set to have a consistent set of clinical endpoints for chronic heart disease outpatient care studies. Further, future studies should examine the effects of models of outpatient care or different interventions with adjusted outcome parameters to determine which interventions in the MoCs described here have the most positive effects for the person concerned. This could provide an impetus for practice and policy to develop renewed or new model of outpatient care for patients with chronic heart diseases.
Availability of data and materials
The data underlying this article are available in the article and in its online supplementary material.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Article PubMed Google Scholar
Falk H, Ekman I, Anderson R, Fu M, Granger B. Older patients’ experiences of heart failure—an integrative literature review. J Nurs Scholarsh. 2013;45(3):247–55.
Emmons-Bell S, Johnson C, Roth G. Prevalence, incidence and survival of heart failure: a systematic review. Heart. 2022;108(17):1351–60.
Savarese G, Lund LH. Global Public Health Burden of Heart Failure. Card Fail Rev. 2017;3(1):7–11. Available from: https://pubmed.ncbi.nlm.nih.gov/28785469 .
Liang F, Wang Y. Coronary heart disease and atrial fibrillation: a vicious cycle. Am J Physiol Heart Circ Physiol. 2021;320(1):H1–12.
Li H, Song X, Liang Y, Bai X, Liu-Huo W-S, Tang C, et al. Global, regional, and national burden of disease study of atrial fibrillation/flutter, 1990–2019: results from a global burden of disease study, 2019. BMC Public Health. 2022;22(1):2015.
Article PubMed PubMed Central Google Scholar
Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, et al. Temporal trends and patterns in heart failure incidence: a population-based study of 4 million individuals. The Lancet. 2018;391(10120):572–80.
Article Google Scholar
Baldi I, Azzolina D, Berchialla P, Gregori D, Scotti L, Corrao G. Comorbidity-adjusted relative survival in newly hospitalized heart failure patients: a population-based study. Int J Cardiol. 2017;243:385–8.
Allen LA, Stevenson LW, Grady KL, Goldstein NE, Matlock DD, Arnold RM, et al. Decision making in advanced heart failure: a scientific statement from the American Heart Association. Circulation. 2012;125(15):1928–52.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–1032.
PubMed Google Scholar
Roger VL. Epidemiology of heart failure: a contemporary perspective. Circ Res. 2021;128(10):1421–34.
Article CAS PubMed Google Scholar
Nordfonn OK, Morken IM, Bru LE, Husebø AML. Patients’ experience with heart failure treatment and self-care-A qualitative study exploring the burden of treatment. J Clin Nurs. 2019;28(9–10):1782–93.
Davidson PM, Elliott D. Managing approaches to nursing care delivery. In: J. Daly (Ed.), Preparing for Professional Nursing Practice. Sydney: Maclennan and Petty; 2001.
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231.
Snilstveit B, Vojtkova M, Bhavsar A, Stevenson J, Gaarder M. Evidence & Gap Maps: A tool for promoting evidence informed policy and strategic research agendas. J Clin Epidemiol. 2016;79:120–9.
Pollock A, Campbell P, Brunton G, Hunt H, Estcourt L. Selecting and implementing overview methods: implications from five exemplar overviews. Syst Rev. 2017;6(1):145.
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39.
Bragge P, Clavisi O, Turner T, Tavender E, Collie A, Gruen RL. The Global Evidence Mapping Initiative: scoping research in broad topic areas. BMC Med Res Methodol. 2011;11:92.
Cooper ID. What is a “mapping study?” J Med Libr Assoc. 2016;104(1):76–8.
Andrew Booth. EVIDENT Guidance for Reviewing the Evidence: a compendium of methodological literature and websites; 2016.
Miake-Lye IM, Hempel S, Shanman R, Shekelle PG. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016;5(1):28.
Centre for Reviews and Dissemination. Welcome to CRD Database: About DARE. https://www.crd.york.ac.uk/CRDWeb/AboutPage.asp ; 2015 2015 Jun 3 [cited 2019 Sep 3].
Dodd S, Clarke M, Becker L, Mavergames C, Fish R, Williamson PR. A taxonomy has been developed for outcomes in medical research to help improve knowledge discovery. J Clin Epidemiol. 2018;96:84–92.
Kirkham JJ, Davis K, Altman DG, Blazeby JM, Clarke M, Tunis S, et al. Core Outcome Set-STAndards for Development: The COS-STAD recommendations. PLoS Med. 2017;14(11):e1002447.
Pérez-Bracchiglione J, Meza N, Bangdiwala SI, Guzmán EN de, Urrútia G, Bonfill X et al. GROOVE - Graphical Representation of Overlap for OVErviews: Open Science Framework; 2022 2022.
Pieper D, Antoine S-L, Mathes T, Neugebauer EAM, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Allida S, Du H, Xu X, Prichard R, Chang S, Hickman LD et al. mHealth education interventions in heart failure. Cochrane Database Syst Rev. 2020;7(7):CD011845. Available from: https://pubmed.ncbi.nlm.nih.gov/32613635/ .
Palm P, Qvist I, Rasmussen TB, Christensen SW, Håkonsen SJ, Risom SS. Educational interventions to improve outcomes in patients with atrial fibrillation-a systematic review. Int J Clin Pract. 2020;74(11):e13629.
Jovicic A, Holroyd-Leduc JM, Straus SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord 2006 [cited 2022 Jun 3]; 6:43. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1660572/pdf/1471-2261-6-43.pdf .
Koshman SL, Charrois TL, Simpson SH, McAlister FA, Tsuyuki RT. Pharmacist care of patients with heart failure: a systematic review of randomized trials. Arch Intern Med. 2008;168(7):687–94.
van der Meer S, Zwerink M, van Brussel M, van der Valk P, Wajon E, van der Palen J. Effect of outpatient exercise training programmes in patients with chronic heart failure: a systematic review. Eur J Prev Cardiol. 2012;19(4):795–803. Available from: https://pubmed.ncbi.nlm.nih.gov/22988592/ .
Labrunée M, Pathak A, Loscos M, Coudeyre E, Casillas J-M, Gremeaux V. Therapeutic education in cardiovascular diseases: state of the art and perspectives. Ann Phys Rehabil Med. 2012;55(5):322–41.
Clarkesmith DE, Pattison HM, Khaing PH, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database Syst Rev. 2017;2017(4):CD008600.
Rice H, Say R, Betihavas V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review Patient Educ Couns. 2018;101(3):363–74.
Sterling MR, Shaw AL, Leung PB, Safford MM, Jones CD, Tsui EK, et al. Home care workers in heart failure: a systematic review. J Multidiscip Healthc. 2018;11:481–92.
Tse G, Chan C, Gong M, Meng L, Zhang J, Su X-L, et al. Telemonitoring and hemodynamic monitoring to reduce hospitalization rates in heart failure: a systematic review and meta-analysis of randomized controlled trials and real-world studies. J Geriatr Cardiol. 2018;15(4):298–309.
PubMed PubMed Central Google Scholar
Tse G, Gong M, Meng L, Ng EMC, Tsang NS, Ali-Hasan-Al-Saegh S, et al. Effects of Telemonitoring and Hemodynamic Monitoring on Mortality in Heart Failure: a Systematic Review and Meta-analysis. Curr Emerg Hosp Med Rep. 2019;7(2):36–47.
Cui X, Dong W, Zheng H, Li H. Collaborative care intervention for patients with chronic heart failure: A systematic review and meta-analysis. Medicine (Baltimore). 2019;98(13):e14867.
Duffy JR, Hoskins LM, Chen M-C. Nonpharmacological strategies for improving heart failure outcomes in the community: a systematic review. J Nurs Care Qual. 2004;19(4):349–60.
Schumacher PM, Becker N, Tsuyuki RT, Griese-Mammen N, Koshman SL, McDonald MA, et al. The evidence for pharmacist care in outpatients with heart failure: a systematic review and meta-analysis. ESC Heart Fail. 2021;8(5):3566–76.
Schichtel M, Wee B, Perera R, Onakpoya I, Albury C. Effect of behavior change techniques targeting clinicians to improve advance care planning in heart failure: a systematic review and meta-analysis. Ann Behav Med. 2021;55(5):383–98.
Romiti GF, Pastori D, Rivera-Caravaca JM, Ding WY, Gue YX, Menichelli D, et al. Adherence to the “atrial fibrillation better care” pathway in patients with atrial fibrillation: impact on clinical outcomes-a systematic review and meta-analysis of 285,000 patients. Thromb Haemost. 2022;122(3):406–14.
Ogungbe O, Byiringiro S, Adedokun-Afolayan A, Seal SM, Dennison Himmelfarb CR, Davidson PM, et al. Medication adherence interventions for cardiovascular disease in low- and middle-income countries: a systematic review. Patient Prefer Adherence. 2021;15:885–97.
Gebreyohannes EA, Mill D, Salter S, Chalmers L, Bereznicki L, Lee K. Strategies for improving guideline adherence of anticoagulants for patients with atrial fibrillation in primary healthcare: a systematic review. Thromb Res. 2021;205:128–36.
Biersteker TE, Schalij MJ, Treskes RW. Impact of mobile health devices for the detection of atrial fibrillation: systematic review. JMIR MHEALTH UHEALTH. 2021;9(4):e26161.
Austin RC, Schoonhoven L, Clancy M, Richardson A, Kalra PR, May CR. Do chronic heart failure symptoms interact with burden of treatment? Qualitative literature systematic review. BMJ Open. 2021;11(7):e047060.
Al-Arkee S, Mason J, Lane DA, Fabritz L, Chua W, Haque MS, et al. Mobile apps to improve medication adherence in cardiovascular disease: systematic review and meta-analysis. J Med Internet Res. 2021;23(5):e24190.
Wongvibulsin S, Habeos EE, Huynh PP, Xun H, Shan R, Porosnicu Rodriguez KA, et al. Digital health interventions for cardiac rehabilitation: systematic literature review. J Med Internet Res. 2021;23(2):e18773.
Candelaria D, Randall S, Ladak L, Gallagher R. Health-related quality of life and exercise-based cardiac rehabilitation in contemporary acute coronary syndrome patients: a systematic review and meta-analysis. Qual Life Res. 2020;29(3):579–92.
Choi JY, Choi H, Seomun G, Kim EJ. Mobile-application-based interventions for patients with hypertension and ischemic heart disease: a systematic review. J Nurs Res. 2020;28(5):e117.
Huang K, Liu W, He D, Huang B, Xiao D, Peng Y et al. Telehealth interventions versus center-based cardiac rehabilitation of coronary artery disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2015;22(8):959–71.
Han E, Quek RYC, Tan SM, Singh SR, Shiraz F, Gea-Sánchez M, et al. The role of community-based nursing interventions in improving outcomes for individuals with cardiovascular disease: a systematic review. Int J Nurs Stud. 2019;100: 103415.
Kotb A, Hsieh S, Wells GA. The effect of telephone support interventions on coronary artery disease (CAD) patient outcomes during cardiac rehabilitation: a systematic review and meta-analysis. PLoS ONE. 2014;9(5):e96581.
Salzwedel A, Jensen K, Rauch B, Doherty P, Metzendorf M-I, Hackbusch M, et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: Update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur J Prev Cardiol. 2020;27(16):1756–74.
Sadeghi M, Rahiminam H, Amerizadeh A, Masoumi G, Heidari R, Shahabi J, et al. Prevalence of return to work in cardiovascular patients after cardiac rehabilitation: a systematic review and meta-analysis. Curr Probl Cardiol. 2022;47(7): 100876.
Smigorowsky MJ, Sebastianski M, Sean McMurtry M, Tsuyuki RT, Norris CM. Outcomes of nurse practitioner-led care in patients with cardiovascular disease: a systematic review and meta-analysis. J Adv Nurs. 2020;76(1):81–95. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85074615563&doi=10.1111%2fjan.14229&partnerID=40&md5=ee619a95dbfad56b4bf3e1123c5bfb47 .
Meiring RM, Tanimukai K, Bradnam L. The effect of exercise-based cardiac rehabilitation on objectively measured physical activity and sedentary behavior: a systematic review and meta-analysis. J Prim Care Community Health. 2020;11:2150132720935290.
Nishikawa Y, Hiroyama N, Fukahori H, Ota E, Mizuno A, Miyashita M et al. Advance care planning for adults with heart failure. Cochrane Database Syst Rev. 2020; 2(2):CD013022.
Driscoll A, Meagher S, Kennedy R, Hay M, Banerji J, Campbell D, et al. What is the impact of systems of care for heart failure on patients diagnosed with heart failure: a systematic review. BMC Cardiovasc Disord. 2016;16(1):195.
Risom SS, Zwisler A-D, Johansen PP, Sibilitz KL, Lindschou J, Gluud C et al. Exercise-based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev 2017;2:CD011197.
Heckman GA, Shamji AK, Ladha R, Stapleton J, Boscart V, Boxer RS, et al. Heart Failure Management in Nursing Homes: A Scoping Literature Review. Can J Cardiol. 2018;34(7):871–80.
Kruse CS, Soma M, Pulluri D, Nemali NT, Brooks M. The effectiveness of telemedicine in the management of chronic heart disease - a systematic review. JRSM Open. 2017; 8(3):2054270416681747. [cited 2022 Jun 7] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5347273/pdf/10.1177_2054270416681747.pdf .
Case R, Haynes D, Holaday B, Parker VG. Evidence-based nursing: the role of the advanced practice registered nurse in the management of heart failure patients in the outpatient setting. Dimens Crit Care Nurs. 2010;29(2):57–62.
Schadewaldt V, Schultz T. A systematic review on the effectiveness of nurse-led cardiac clinics for adult patients with coronary heart disease. JBI Library Syst Rev. 2010; 8(2):53–89. Available from: https://pubmed.ncbi.nlm.nih.gov/27820168/ .
Kabboul NN, Tomlinson G, Francis TA, Grace SL, Chaves G, Rac V et al. Comparative Effectiveness of the Core Components of Cardiac Rehabilitation on Mortality and Morbidity: A Systematic Review and Network Meta-Analysis. J Clin Med. 2018;7(12):514.
Bjarnason-Wehrens B, Nebel R, Jensen K, Hackbusch M, Grilli M, Gielen S et al. Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): a systematic review and meta-analysis. Eur J Prev Cardiol. 2020;27(9):929–52. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85067856703&doi=10.1177%2f2047487319854140&partnerID=40&md5=52a90d3e7586541bc6c2eadc91375d82 .
Cavalheiro AH, Silva Cardoso J, Rocha A, Moreira E, Azevedo LF. Effectiveness of tele-rehabilitation programs in heart failure: a systematic review and meta-analysis. HealthServInsights. 2021;14:11786329211021668.
Google Scholar
Rawstorn JC, Gant N, Direito A, Beckmann C, Maddison R. Telehealth exercise-based cardiac rehabilitation: a systematic review and meta-analysis. Heart. 2016;1:1183–92.
Su JJ, Yu D, Paguio JT. Effect of eHealth cardiac rehabilitation on health outcomes of coronary heart disease patients: A systematic review and meta-analysis. J Adv Nurs. 2020;76(3):754–72. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85079320766&doi=10.1111%2fjan.14272&partnerID=40&md5=238b94f8ea50a8dacf6d8ae67a66d4c2 .
Zwisler A-D, Norton RJ, Dean SG, Dalal H, Tang LH, Wingham J, et al. Home-based cardiac rehabilitation for people with heart failure: A systematic review and meta-analysis. Int J Cardiol. 2016;221:963–9.
Treadwell J, Perez R, Stubbs D, McAllister JW, Stern S, Buzi R. Case management and care coordination: supporting children and families to optimal outcomes. Cham, s.l.: Springer International Publishing; 2015. (SpringerBriefs in Public Health).
Wagner EH, Davis C, Schaefer J, von Korff M, Austin B. A survey of leading chronic disease management programs: are they consistent with the literature? Manag Care Q. 1999;7(3):56–66.
CAS PubMed Google Scholar
Nies H, Berman, Philip C, editors. Integrating services for older people: a resource book for managers. Dublin: European Health Management Association (EHMA); 2004. (vol 5) [cited 2021 Jul 16]. Available from: https://ehma.org/wp-content/uploads/2016/08/CARMEN_Integrating-Services-for-Older-People-A-Resource-Book-for-Managers.pdf .
Krumholz HM, Currie PM, Riegel B, Phillips CO, Peterson ED, Smith R, et al. A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation. 2006;114(13):1432–45.
Nolte E, Knai C, Saltman, Richard B. Assessing chronic disease management in European health systems: Concepts and Approaches; 2014 [cited 2021 Jul 16]. Available from: https://www.euro.who.int/__data/assets/pdf_file/0009/270729/Assessing-chronic-disease-management-in-European-health-systems.pdf .
Clark AM, Wiens KS, Banner D, Kryworuchko J, Thirsk L, McLean L, et al. A systematic review of the main mechanisms of heart failure disease management interventions. Heart. 2016;102(9):707–11.
Gallagher C, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME, Mahajan R et al. Integrated care in atrial fibrillation: A systematic review and meta-analysis. Heart. 2017; 103(24):1947–53. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85031688687&doi=10.1136%2fheartjnl-2016-310952&partnerID=40&md5=339bcf8a1c4170dfe2a89b0f7881afe0 .
Gonseth J, Guallar-Castillon P, Banegas JR, Rodriguez-Artalejo F. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reports. Eur Heart J. 2004;25(18):1570–95.
Gorthi J, Hunter CB, Mooss AN, Alla VM, Hilleman DE. Reducing Heart Failure Hospital Readmissions: A Systematic Review of Disease Management Programs. Cardiol Res. 2014;5(5):126–38.
Huntley AL, Johnson R, King A, Morris RW, Purdy S. Does case management for patients with heart failure based in the community reduce unplanned hospital admissions? A systematic review and meta-analysis. BMJ Open. 2016;6(5):e010933.
Jerant AF, Nesbitt TS. Heart failure disease management incorporating telemedicine: a critical review. J Clin Outcomes Manag. 2005;12(4):207–17. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-18744394627&partnerID=40&md5=4a8a9126ac791779d234d9828d045900 .
Kalogirou F, Forsyth F, Kyriakou M, Mantle R, Deaton C. Heart failure disease management: a systematic review of effectiveness in heart failure with preserved ejection fraction. ESC Heart Fail. 2020;7(1):195–213. Available from: https://search.proquest.com/docview/2379680851?accountid=12235 .
Kyriakou M, Middleton N, Ktisti S, Philippou K, Lambrinou E. Supportive care interventions to promote health-related quality of life in patients living with heart failure: a systematic review and meta-analysis. Heart Lung Circ. 2020;29(11):1633–47.
McAlister FA, Lawson FM, Teo KK, Armstrong PW. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001;110(5):378–84.
McAlister FA, Stewart S, Ferrua S, McMurray, John J J V. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44(4):810–9.
Raat W, Smeets M, Janssens S, Vaes B. Impact of primary care involvement and setting on multidisciplinary heart failure management: a systematic review and meta-analysis. ESC Heart Fail. 2021;8(2):802–18.
Takeda A, Martin N, Taylor RS, Taylor SJ. Disease management interventions for heart failure. Cochrane Database Syst Rev 2019;1:CD002752.
Wakefield BJ, Boren SA, Groves PS, Conn VS. Heart failure care management programs: a review of study interventions and meta-analysis of outcomes. J Cardiovasc Nurs. 2013;28(1):8–19.
Fergenbaum J, Bermingham S, Krahn M, Alter D, Demers C. Care in the home for the management of chronic heart failure: systematic review and cost-effectiveness analysis. J Cardiovasc Nurs. 2015;30(4 Suppl 1):S44-51.
Jaarsma T, Brons M, Kraai I, Luttik ML, Stromberg A. Components of heart failure management in home care; A literature review. Eur J Cardiovasc Nurs. 2013;12(3):230–41. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84878238443&doi=10.1177%2f1474515112449539&partnerID=40&md5=708850e642584420f23b41037204f0f3 .
Gandhi S, Mosleh W, Sharma UC, Demers C, Farkouh ME, Schwalm J-D. Multidisciplinary heart failure clinics are associated with lower heart failure hospitalization and mortality: systematic review and meta-analysis. Can J Cardiol. 2017;33(10):1237–44. [cited 2020 May 4] Available from: https://www.onlinecjc.ca/action/showPdf?pii=S0828-282X%2817%2930248-9 .
Rush KL, Burton L, Schaab K, Lukey A. The impact of nurse-led atrial fibrillation clinics on patient and healthcare outcomes: a systematic mixed studies review. Eur J Cardiovasc Nurs. 2019;18(7):526–33.
Schadewaldt V, Schultz T. Nurse-led clinics as an effective service for cardiac patients: results from a systematic review. Int J Evid Based Healthc. 2011;9(3):199–214.
World Health Organization. Telemedicine: Opportunities and Developments in Member States. Report on the Second Global Survey on eHealth 2009. Geneva: World Health Organization; 2010. (Global Observatory for Ehealth). Available from: http://gbv.eblib.com/patron/FullRecord.aspx?p=753845 .
Carbo A, Gupta M, Tamariz L, Palacio A, Levis S, Nemeth Z, et al. Mobile technologies for managing heart failure: a systematic review and meta-analysis. Telemed J E Health. 2018;24(12):958–68.
Chaudhry SI, Phillips CO, Stewart SS, Riegel B, Mattera JA, Jerant AF, et al. Telemonitoring for patients with chronic heart failure: A systematic review. J Card Fail. 2007;13(1):56–62.
Clark RA, Inglis SC, McAlister FA, Cleland JGF, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ (Online). 2007;5:334(7600):942.
Ding H, Chen SH, Edwards I, Jayasena R, Doecke J, Layland J et al. Effects of different telemonitoring strategies on chronic heart failure care: systematic review and subgroup meta-analysis. J Med Internet Research 2020; 22(11). Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85096202824&doi=10.2196%2f20032&partnerID=40&md5=240dd208c066cbf51fdd8c8f3a9cf248 .
Drews TEI, Laukkanen J, Nieminen T. Non-invasive home telemonitoring in patients with decompensated heart failure: a systematic review and meta-analysis. ESC Heart Fail. 2021;8(5):3696–708.
Inglis SC, Clark RA, McAlister FA, Ball J, Lewinter C, Cullington D et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev. 2010;8:CD007228.
Inglis SC, Clark RA, Dierckx R, Prieto-Merino D, Cleland JGF. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst Rev. 2015;10:CD007228.
Kitsiou S, Vatani H, Paré G, Gerber BS, Buchholz SW, Kansal MM, et al. Effectiveness of mobile health technology interventions for patients with heart failure: systematic review and meta-analysis. Can J Cardiol. 2021;37(8):1248–59.
Kotb A, Cameron C, Hsieh S, Wells G. Comparative effectiveness of different forms of telemedicine for individuals with heart failure (HF): a systematic review and network meta-analysis. PLoS ONE. 2015;10(2):e0118681.
Lin M-H, Yuan W-L, Huang T-C, Zhang H-F, Mai J-T, Wang J-F. Clinical effectiveness of telemedicine for chronic heart failure: a systematic review and meta-analysis. J Investig Med. 2017;65(5):899–911.
Louis AA, Turner T, Gretton M, Baksh A, Cleland JGF. A systematic review of telemonitoring for the management of heart failure. Eur J Heart Fail. 2003;5(5):583–90.
Martinez A, Everss E, Rojo-Alvarez JL, Figal DP, Garcia-Alberola A. A systematic review of the literature on home monitoring for patients with heart failure. J Telemed Telecare. 2006;12(5):234–41.
Nick JM, Roberts LR, Petersen AB. Effectiveness of telemonitoring on self-care behaviors among community-dwelling adults with heart failure: a quantitative systematic review. JBI Evidence Synthesis. 2021;19(10):2659–94.
Pandor A, Thokala P, Gomersall T, Baalbaki H, Stevens JW, Wang J, et al. Home telemonitoring or structured telephone support programmes after recent discharge in patients with heart failure: systematic review and economic evaluation. Health Technol Assess. 2013;17(32):1–207.
Article CAS PubMed PubMed Central Google Scholar
Pekmezaris R, Tortez L, Williams M, Patel V, Makaryus A, Zeltser R et al. Home telemonitoring in heart failure: a systematic review and meta-analysis. Health Aff (Millwood) 2018.
Son Y-J, Lee Y, Lee H-J. Effectiveness of mobile phone-based interventions for improving health outcomes in patients with chronic heart failure: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(5):1749.
Sua YS, Jiang Y, Thompson DR, Wang W. Effectiveness of mobile phone-based self-management interventions for medication adherence and change in blood pressure in patients with coronary heart disease: A systematic review and meta-analysis. European Journal of Cardiovascular Nursing 2020; 19(3):192–200. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85077147001&doi=10.1177%2f1474515119895678&partnerID=40&md5=c9ad2320e9337b672d2627c09fb12ed0 .
Naylor M, Keating SA. Transitional care. Am J Nurs. 2008;108(9 Suppl):58–63; quiz 63.
Albert NM. A systematic review of transitional-care strategies to reduce rehospitalization in patients with heart failure. Heart Lung. 2016;45(2):100–13.
Feltner C, Jones CD, Cene CW, Zheng Z-J, Sueta CA, Coker-Schwimmer EJL, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160(11):774–84.
Li Y, Fu MR, Fang J, Zheng H, Luo B. The effectiveness of transitional care interventions for adult people with heart failure on patient-centered health outcomes: a systematic review and meta-analysis including dose-response relationship. Int J Nurs Stud. 2021;117: 103902.
Li Y, Fu MR, Luo B, Li M, Zheng H, Fang J. The effectiveness of transitional care interventions on health care utilization in patients discharged from the hospital with heart failure: a systematic review and meta-analysis. J Am Med Dir Assoc. 2021;22(3):621–9.
Van Spall, Harriette G C, Rahman T, Mytton O, Ramasundarahettige C, Ibrahim Q, Kabali C et al. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis. Eur J Heart Fail. 2017;19(11):1427–43.
Vedel I, Khanassov V. Transitional care for patients with congestive heart failure: a systematic review and meta-analysis. United States; 2015.
Inglis SC, Clark RA, McAlister FA, Stewart S, Cleland JGF. Which components of heart failure programmes are effective? A systematic review and meta-analysis of the outcomes of structured telephone support or telemonitoring as the primary component of chronic heart failure management in 8323 patients: Abridged Cochrane Review. Eur J Heart Fail. 2011;13(9):1028–40.
Batsis JA, DiMilia PR, Seo LM, Fortuna KL, Kennedy MA, Blunt HB, et al. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc. 2019;67(8):1737–49.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017:j4008. [cited 2019 Sep 6].
Whiting P, Savović J, Higgins JPT, Caldwell DM, Reeves BC, Shea B et al. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016; 69:225–34. [cited 2022 Mar 1] Available from: https://www.bristol.ac.uk/media-library/sites/social-community-medicine/robis/robisjclinepi.pdf .
Download references
Acknowledgements
The authors would like to thank Adeline Reinemann for providing helpful comments on the draft manuscript.
Open Access funding enabled and organized by Projekt DEAL. The project (ZS/ 2018/ 12/ 96167) belongs to the Research Association “Autonomy in old Age” (AiA) funded by the European Union (ERDF-European Regional Development Fund) and the State of Saxony-Anhalt, Germany.
Author information
Authors and affiliations.
Institute of Social Medicine and Health Systems Research, Medical Faculty, Otto von Guericke University Magdeburg, Leipziger Str. 44, Magdeburg, Sachsen-Anhalt, 39120, Germany
Madlen Hoerold, Heike Heytens, Carla Maria Debbeler, Saskia Ehrentreich & Christian J. Apfelbacher
Department of Angiology and Cardiology, Otto-von-Guericke University of Magdeburg, Leipziger Str. 44, Magdeburg, Sachsen-Anhalt, 39120, Germany
Thomas Rauwolf, Alexander Schmeißer, Marc Gottschalk & Ruediger C. Braun-Dullaeus
Department of Public Health and Health Education, University of Education Freiburg, Kunzenweg 21, Freiburg, Baden-Würtemberg, 79117, Germany
Eva Maria Bitzer
You can also search for this author in PubMed Google Scholar
Contributions
CA, MH, HH, EMB, RBD, AS, TR contributed to the design of the study, development of the selection criteria, and previously registered the protocol with PROSPERO. MH and HH developed the search strategy using previously published research. For the evidence map MH, HH, SE, AS, and TR completed the data search and screening. MH, HH, CD, and SE were involved in data extraction and synthesis. CD and MH conducted data visualisation. MH, CD, and HH drafted the original manuscript. All authors read, provided feedback on and approved the final manuscript. RBD acquired funding. CA provided substantial methodological advice and supervised the study.
Corresponding author
Correspondence to Madlen Hoerold .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
All authors have read the final version of the manuscript and approved its submission for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Search strategy at PubMed.
Additional file 2:
Characteristics of the included SRs.
Additional file 3:
Mapping of the single interventions of the included SRs.
Additional file 4:
Mapping of the primary outcomes of the included SRs.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hoerold, M., Heytens, H., Debbeler, C.M. et al. An evidence map of systematic reviews on models of outpatient care for patients with chronic heart diseases. Syst Rev 12 , 80 (2023). https://doi.org/10.1186/s13643-023-02227-z
Download citation
Received : 08 June 2022
Accepted : 30 March 2023
Published : 06 May 2023
DOI : https://doi.org/10.1186/s13643-023-02227-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Heart failure
- Coronary heart disease
- Atrial fibrillation
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (43,934,836 articles, preprints and more)
- Free full text
- Citations & impact
- Similar Articles
A systematic review on clinical guidelines of home health care in heart failure patients.
Author information, affiliations.
- Hashemlu L 1
- Esmaeili R 2
- Bahramnezhad F 3
BMC Nursing , 18 Apr 2023 , 22(1): 127 https://doi.org/10.1186/s12912-023-01294-w PMID: 37072792 PMCID: PMC10111843
Abstract
- Conclusions
Free full text

A systematic review on clinical guidelines of home health care in heart failure patients
Leila hashemlu.
1 PhD of Nursing, Student Research Committee, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Roghayeh Esmaeili
2 Department of Medical-Surgical Nursing, School of Nursing & Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Fatemeh Bahramnezhad
3 Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
4 Spiritual Health Group, Research Center of Quran, Hadith and Medicine, Tehran University of Medical Sciences, Tehran, Iran
Camelia Rohani
5 Palliative Care Reseaech Center, Ersta Sköndal Bräcke University College, Campus Ersta, Stigbergsgatan 30, Box 11189, Stockholm, SE-100 61 Sweden
6 Community Health Nursing Department, School of Nursing & Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- Associated Data
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request. All requests will be answered within a maximum of 1 month by email.
“Guidelines for the care of heart failure patients at home support safe and effective evidence-based practice. The aims of the present study were: [ 1 ] to identify guidelines addressing the care at home for adults with heart failure and [ 2 ] evaluate the quality of the guidelines and the extent to which they address eight components of home-based HF disease management.”
A systematic review was conducted of articles published between 1st of January 2000 to 17th of May 2021 using the databases of PubMed, Web of Science, Scopus, Embase, Cochrane, and nine specific websites for guideline development organisations. Clinical guidelines for HF patients with recommendations relevant to care provision at home were included. The results were reported according to the Preferred Reporting Items for Systematic Reviews (PRISMA-2020) criteria. The quality of included guidelines was evaluated using the Appraisal of Guidelines for Research and Evaluation-II (AGREE-II) by two authors independently. Guidelines were evaluated for their coverage of eight components of HF care at home, consisting of integration, multi-disciplinary care, continuity of care, optimized treatment, patient education, patient and partner participation, care plans with clear goals of care, self-care management and palliative care.
Ten HF guidelines, including two nursing-focused guidelines and eight general guidelines were extracted from 280 studies. After evaluation of quality by AGREE-II, two guidelines obtained the highest score: “NICE” and the “Adapting HF guideline for nursing care in home health care settings. Five guidelines addressed all eight components of care at home while the others had six or seven.
This systematic review identified ten guidelines addressing care at home for patients with HF. The highest quality guidelines most relevant to the care at home of patients with HF are the “NICE” and “Adapting HF guideline for nursing care in home health care settings” and would be most appropriate for use by home healthcare nurses.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12912-023-01294-w.
- Introduction
With growing numbers and complexity of persons living with HF, the management heart failure (HF) challenges the whole health system globally [ 1 ]. HF affects nearly 64.3 million people worldwide, a roughly two-fold increase from 33.5 million since 1990 [ 2 ]. The prevalence of HF has progressively increased for many years, both due to effective therapies keeping patients alive longer and the ageing of many populations worldwide [ 3 ], with the latter explaining more of the increase. Due to the chronic nature of HF, the recurrent disease exacerbations and patient’s re-admission to the hospital is one of the significant health problems in today’s society [ 4 ].
Multidisciplinary management of patients has been recommended in HF guidelines and it can improve caring outcomes [ 5 ]. A multidisciplinary team often consists of nurses, physicians, specialists in cardiology, in addition to physiotherapists, dieticians and social workers can provide standardized home care for HF patients [ 6 , 7 ] by supporting person-centered care and self-management services. The person-centered approach to develop guidelines necessitates considering the patient’s conditions and needs, patient preferences, participation in goal-setting plans, and individual beliefs and values [ 8 ] and nurses are well positioned to support these functions.
Numerous studies show that ongoing person-centered care has positive results in nursing management of the HF patients and reduces their re-admission rate [ 9 , 10 ]. One of the models for continuing care of the HF patients after discharging from hospital, is home healthcare services [ 11 ]. The term “home healthcare” can be perceived very different across countries according to their healthcare systems and delivering services for different target groups. Home healthcare services can deliver to the patients in their home or nursing home care centers. They can range from professional care for those requiring long-term care to those who only require assistance with relatively simple tasks on an as-needed basis (primarily support services or basic nursing care – e.g., bathing and dressing) [ 12 ]. Home healthcare services in patients’ home help families participate in their patient care and self-care. These services are a crucial component of community-based care services [ 10 ]. Maintaining and restoring patient’s independence is one of the primary missions of home healthcare services [ 13 , 14 ].
Home healthcare nurses can provide services that previously were available only in hospitals. By transferring the knowledge and practice from hospitals to the patients’ home, the role of the home healthcare nurses is expanded [ 15 ]. HF patients receive different services at home by home healthcare nurses. Nurses manage patients in various aspects of physical, mental, spiritual and give them emotional support [ 16 ]. They provide general to specific care such as prevent medication and other medical errors, evaluate responses to therapy, identify early signs of problems such as impending volume overloading collaboration with patients’ physicians, implement strategies to prevent the onset of symptoms or minimize their effects, teach patients and caregivers about early symptom recognition, but also coach them about effective treatment, such as the use of as-needed diuretics at home for HF patients [ 7 , 16 , 17 ].
Nurses are one of the largest groups of the home-based healthcare providers, but provision of guideline-based caring has remains less than optimal [ 18 ]. Nursing management of HF patients at home is very critical. It has been recommended that the following eight components are considered: “integrated, multi-disciplinary care (integrate the care between community care, secondary and primary care, use a team approach, prioritize continuity of care and staff members), patient and partner participation, care plans with clear goals of care (focus care to improve quality of life, functional status and sense of security for patients include communication protocols palliative treatment), patient education (also family education), self-care management, appropriate access to care (use of tele-rehabilitation, telemonitoring, and telephone follow up, palliative care approach), optimize treatment (use guidelines and Individualize treatment” [ 19 ].
Clinical practice guidelines (CPGs) have helped to continuously improve patient safety and care across the globe. CPGs need to be both well developed and effectively introduced in clinical practice so that we can achieve quality patient care [ 20 ]. Although high-quality clinical guidelines can be a gold standard for practice [ 21 ], little is known about the content and consistency of HF guidelines relevant to homecare. To address these gaps, we conducted a systematic review with these aims: [ 1 ] to identify clinical home care guidelines in adult HF patients and their recommendations [ 2 ] to evaluate quality of the guidelines as well as to assess eight components of disease management at home in the guidelines.
The present systematic review is reported using the Preferred Reporting Items for Systematic Reviews (PRISMA 2020) [ 22 ]. The protocol of this systematic review was registered on PROSPERO (CRD42021241979).
Data sources and search strategy
A systematic search was performed to identify appropriate guidelines published between the1st of January 2000 to 17th of May 2021. We did an extensive search in databases of PubMed, Web of Science, Scopus, Embase, Cochrane and nine specific websites for organizations of guideline development, including “Agency for Healthcare Research and Quality & National Guideline Clearinghouse, Guideline International Network (G-I-N), New Zealand Guidelines Group, National Health and Medical Research Council (NHMRC), National Institute for Clinical Excellence (NICE; UK), Australian National Health and Medical Research Council, Scottish Intercollegiate Guidelines Network (SIGN), Canadian Medical Association InfoBase of Clinical Practice Guidelines, Professional CR society websites (ICCPR; http://globalcardiacrehab.com/cr-guidelines/ ). In addition, authors carried out manual searches as a supplemental approach to identify additional primary studies for systematic reviews [ 23 ]. Appropriate keywords were identified using Medical Subject Headings (Mesh). The selected keywords were: guideline/guidelines or recommendation, or guideline adherence or practice guideline, and home care and heart failure. These keywords were combined together by Boolean operators, and an extensive search was done (Appendix1).
Study selection
Two authors independently screened all potentially relevant studies by reading the titles, abstracts and full-text of the studies according to inclusion criteria of the study. Disagreements were solved by discussion and using the viewpoint of a third reviewer.
Inclusion and exclusion criteria
The term “home care” can be perceived differently across countries, depending on their healthcare systems and how they deliver services to different target groups. The definition of home care used in this review includes short-term and long-term professional care provided by home healthcare nurses within own patients’ home [ 12 ]. The scope of home healthcare services for HF patients can be preventive, acute, rehabilitative or palliative.
The inclusion criteria for this study were: the guideline was developed specifically for patients with HF, and the publication language was English. It was published between 1st of January 2000 to 17th of May 2021, and was labelled guideline/guidelines, or recommendation, or guideline adherence or practice guideline. When there were multiple versions of the guideline, the most recently updated one was chosen.
The exclusion criteria were: the guidelines did not reference home health care services, it was not supported by a health professional association or society, public or private organization, healthcare organization or government agency. Also, it did not target HF patients, and its recommendations was not based on a systematic literature search.
Data collection
Data collection was divided into the three steps in our study: [ 1 ] to run a systematic search and selection of current evidence-based guidelines for HF patients that can be applied to home-based care (Fig. 1 ), [ 2 ] to evaluate of the methodological quality of the selected guidelines with the Appraisal of Guidelines for Research and Evaluation (AGREE-II) and [ 3 ] to compare recommendations of the guidelines with the eight components of disease management at home [ 19 ].

Diagram of the Study selection according to the PRISMA 2020 [ 25 ]
Two independent evaluators conducted data extraction. They used specific forms that were designed in the research team to extract the required data. When there was no consensus, a third evaluator assessed the situation. The data were extracted from all included guidelines: title, publication year, organization, country or region, target users, standardized level of evidence, search strategy for evidence. During the whole the process, a third evaluator checked the data for errors and resolved discrepancies or disagreements through discussions or consultations.
To evaluate the methodological quality of the guidelines, AGREE-II was used. The AGREE-II includes 23 items divided into the following six categories: scope and purpose (3 items), stakeholder involvement (3 items), the rigor of development (8 items), clarity of presentation (3 items), applicability (4 items) and editorial independence (2 items). A seven-point Likert scale is used to evaluate each one of the 23 items between 1 (strongly disagree) to 7 (strongly agree). Each of the six-domain scores is calculated separately by adding up all the scores of the specific items in a domain, as well as by calculating the aggregate as a percentage of the highest score for that domain. The following method was used to calculate the Domain scores (obtained score - minimum possible score) / (maximum possible score - minimum possible score). The minimum possible score was calculated as 1× (number of items) × (number of appraisers). The maximum possible score was calculated as 7× (number of items) × (number of appraisers) [ 24 ]. The value of 50% has been defined as a cut-off for AGREE-II, and values over that threshold were deemed satisfactory [ 25 ]. The quality assessment of all included clinical guidelines was performed by two evaluators, independently.
Comparison of the clinical guidelines based on the eight components of HF management at home
In integrating hospital care to home, it has been advised to consider the following components in home care of HF patients: ”Integrated, multi-disciplinary care, continuity of care and care plans, optimized treatment according to guidelines, patients and caregiver’s education, patient and partner participation, care plans with clear goals of care, self-care management, and palliative care” [ 19 , 26 ]. We used these components to identify comprehensive guidelines for home care of HF patients.
The results of study selection were shown based on the PRISMA 2020 [ 26 ] in Fig. 1 . In the initial search, 280 records were obtained. From 206 non-duplicate records, the title and abstract of each study were screened, of which 174 were excluded and, 32 full guidelines text remained; among, them, 22 guidelines were excluded due to incorrect patient population, protocols, not refer to homecare, quality too low, not based on a systematic literature search were excluded and, the final selection yielded a total of 10 clinical practice guidelines for HF patients, including two nursing-focused guidelines [ 19 , 27 ] and eight general guidelines [ 28 – 35 ].
Characteristics of the clinical guidelines
Table 1 . presents the characteristics of the guidelines included. The majority (60%) of the guidelines were published or updated within the latest three years. Among the 10 guidelines, seven (70%) were developed or published by national institutions of HF, and the remaining three by the independent expert panel and Institute for Clinical Systems Improvement (ICSI). Overall, all of guidelines were developed based on evidence (100%). The guidelines were developed in different places: the USA (four guidelines), the UK (one guideline), Europe (two guidelines), Canada (one guideline), Scotland (one guideline), and Australia (one guideline).
Characteristics of 10 selected clinical home care guidelines for HF patients in the study
Quality assessment of guidelines
Quality assessment of guidelines was done based on the AGREE-II guidelines. The AGREE-II includes 23 items divided into the following six domains: scope and purpose (3 items), stakeholder involvement (3 items), the rigor of development (8 items), clarity of presentation (3 items), applicability (4 items) and editorial independence (2 items).The results of the domain scores of the 10 guidelines are shown in Table 2 . Among the 10 guidelines, guidelines of “the National Institute for Health and Care Excellence -NICE” and “Adapting HF Guideline for Nursing Care in Home Healthcare settings scored higher than 50% across all six domains. The field of Recommendations for all 10 selected guidelines are shown in Table 3 .
The results of quality evaluation of the clinical home care guidelines by using the AGREE-II
Reported recommendations field in 10 selected clinical home care guidelines in HF patients
Evaluation of eight components of disease management at home in the guidelines
Eight principal components of HF patient’s management at home were evaluated in all guidelines. They were extracted from a practical home care guide for HF patients in the guidelines following a systematic review and an international expert panel meeting [ 19 , 26 ]. Our results showed that the level of details varied in the guidelines. Five guidelines addressed all eight components and the rest of them addressed six or seven components. These results are shown in Table 4 .
Comparison of the clinical guidelines based on the recommended components of home care
This is the first systematic review to identify the quality of clinical practice guidelines on home-based care for HF Patients. In this review, two nursing-focused guidelines and eight general guidelines were extracted. All general HF guidelines can be applied to HF care at home, depending on the clinical characteristics and the need for interprofessional HF training as well as more attention to home care planning and advanced care. Our results showed that there are two specific HF CPGs for home care nursing.
The first specific HF guideline was “Practical guide on Home Health in HF patients” (2012) [ 19 ]. The purpose of this guide was to describe the characteristics of home-based heart failure care and develop guidance for establishing and delivering home-based care for HF patients by health care providers. One of the preferences of this guide was including eight components of HF care at home; Integrated, multi-disciplinary care, continuity of care and care plans, optimized treatment according to guidelines, patients and caregiver’s education, patient and partner participation, care plans with clear goals of care, self-care management, and palliative care. In our study, we used these components to categorize all selected guidelines. The second CPGs was “adapting HF guideline for nursing care in home health settings” that adapt general HF CPGs for home health nursing expectations and scope of practice [ 27 ].
CPGs’ quality, detail of recommendations, and applicability vary, making selecting high-quality CPGs to implement complex. Based on the results of the study, nurses should be aware of the differences in the quality between these guidelines and try to use the highest quality guidelines based on the context and health system. The first step in improving the quality and outcomes for HF patients receiving home care is to identify clinical home care guidelines for adult HF patients and their recommendations, evaluate the quality of the guidelines, and assess eight components of disease management at home in the guidelines. CPGs should create various materials to support implementation activity and offer advice on implementing the recommendations [ 36 ]. Therefore, we recommend that nurses rely on CPGs that perform better in the ‘applicability’ domain.
By using the AGREE-II, the quality of all included guidelines were evaluated. AGREE-II assesses how well a CPG development process is reported, but the content of the CPG recommendations has not been reported. We have attempted to consider capturing this information detail within our extraction of guideline recommendations and Comparison of the clinical guidelines based on the recommended eight components of home care [ 19 ]. This study was similar to previous systematic evaluations of clinical practice guidelines in other clinical disciplines: the highest average AGREE-II values were computed in domains of “editorial independence” and “clarity of presentation” In contrast, the lowest average score was acquired in the domain of “Applicability” [ 37 ]. A large majority of guidelines were developed without considering if they had recognized facilitators and obstacles to execution, presented criteria for monitoring or auditing, conducted economic analysis, and provided practice instruments.
HF CPGs were rated based on the AGREE-II in our study. “Chronic heart failure in adults: diagnosis and management NICE-2018” and “adapting HF guideline for nursing care in home health settings guidelines” achieved score of more than 50% in all six domains. NICE guidelines used evidence-based strategies that weighed possible opportunities and risks, as well as clinical and cost-effectiveness. Besides, during the guideline development process, NICE involved multi-disciplinary guideline workgroups, including stakeholders in a collaborative, explicit, and transparent manner. It produced a range of materials to support implementation activity [ 28 ].
All guidelines can be a valuable guide for health care professionals who are involved in the home care of HF patients, thereby reducing unnecessary readmission of the patients in the hospital. Moreover, they can improve the quality of home health care services and clinical outcomes. Specific HF CPGs for home care seem more practical but can also be used in conjunction with general HF guidelines. However, what is certain is that the guidelines should be clear, concise, and practical, or even short versions can be produced from extended versions for ease of use.
As nurses are one of the largest groups of the home-based healthcare providers, it is recommended that authors of the guidelines pay more attention to the role of nurses in outpatient settings, such as patients’ home. Also, more effective education of HF patients and their families and their participation in self-care should be considered.
- Strengths and limitations
This systematic review included a comprehensive search for guidelines, the systemic and explicit application of eligibility criteria, and the careful consideration of guideline quality by using the AGREE-II, and did a rigorous analytical approach. However, several limitations could have biased our results. There is the possibility of missing clinical guidelines in other languages, as we restricted our search to only English language guidelines. AGREE-II emphasizes the technical validity of guideline recommendations, not the clinical acceptability or effectiveness. The information of this review was included particular sources at a specific range time; new guidelines have been released after May 2021, are not included.
This is the first study to identify and evaluate clinical home care guidelines for HF patients. This review showed that there are 10 general and specific guidelines for home care of HF patients, but there are only two specific nursing guidelines. Two guidelines with high quality were: “NICE” and “Adapting HF guideline for nursing care in home health care settings”. It is recommended that they use by home healthcare nurses during caring of HF patients at their home.
- Future work is required to ensure:
The incoming guidelines make suggestions on the development of viable strategies for homecare stakeholders. It is very important a person-centered approach to guideline development to ensure that all bio-psycho-social needs are addressed.
Continuous care needs to be strengthened and effective interventions that ensure quality HF care to home care.
A comprehensive understanding of complex needs would facilitate and evaluate the appropriateness of current health policy proposals for home care.
It is suggested that guideline authors developed useful and holistic CPG for Home Health Care in HF Patients.
According to the special needs and resources, cultural and economic differences in each health care system, clinical guidelines should be adapted.
The future study has to look for impediments to guideline implementation and adherence and strategies to overcome these barriers.
- Electronic supplementary material
Below is the link to the electronic supplementary material.
- Acknowledgements
The present study is part of the first author’s PhD nursing dissertation. We would like to express our sincere thanks and persons who cooperated in the implementation of the project.
- List of abbreviations
- Author contributions
The study was designed by L.H,CR, R.E and F.B. All authors have read and approved the manuscript. L.H participated as the main interviewer data collection, data analysis. L.H,C.R, RE and F.B have made substantial contributions in the conceptualization, design of the study and interpretation of the study findings. All authors have contributed to the drafting and critically revising the manuscript. All the authors are responsible for the content and have approved this final version of the manuscript.
This research received no funding.
- Data availability
- Declarations
Not applicable.
The authors declare that they have no competing interests.
1 National Institute for Health and Care Excellence.
2 Ia evidence from systematic reviews or meta-analysis of randomised controlled trials.
Ib evidence from at least one randomised controlled trial.
IIa evidence from at least one controlled study without randomisation.
IIb evidence from at least one other type of quasi-experimental study such as a cohort study.
III evidence from non-experimental descriptive studies, such as comparative studies, correlation studies, case-control studies and case series.
IV evidence from expert committee reports or opinions or clinical experience of respected authorities.
3 Canadian Cardiovascular Society.
4 Scottish Intercollegiate Guidelines Network.
1 - Meta-analyses, systematic reviews, or RCTs with a high risk of bias.
2 - Case-control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal.
3 Non-analytic studies, e.g. case reports, case series.
4 Expert opinion.
6 European Society of Cardiology.
7 American Heart Association and American College of Cardiology Foundation.
8 United States of America.
9 Level of Evidence.
10 Level A Randomized, Controlled, Clinical Trials May be assigned based on results of a single methodologically rigorous trial.
Level B Cohort and Case-Control Studies Post hoc, subgroup analysis, and meta-analysis Prospective observational studies or registries.
Level C Expert Opinion Observational studies-epidemiologic findings Safety reporting from large-scale use in practice.
11 Heart Failure Society of America.
12 Institute for Clinical Systems Improvement.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Contributor Information
Leila Hashemlu, Email: [email protected] .
Roghayeh Esmaeili, Email: [email protected] .
Fatemeh Bahramnezhad, Email: ri.ca.smut.anis@dahzenmarhab .
Camelia Rohani, Email: [email protected] , Email: [email protected] .
Full text links
Read article at publisher's site: https://doi.org/10.1186/s12912-023-01294-w
Citations & impact
Impact metrics, alternative metrics.

Article citations
The negative impact of insulin resistance/hyperinsulinemia on chronic heart failure and the potential benefits of its screening and treatment..
Fazio S , Mercurio V , Affuso F , Bellavite P
Biomedicines , 11(11):2928, 30 Oct 2023
Cited by: 0 articles | PMID: 38001929 | PMCID: PMC10669553
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Beyond the black stump: rapid reviews of health research issues affecting regional, rural and remote Australia.
Osborne SR , Alston LV , Bolton KA , Whelan J , Reeve E , Wong Shee A , Browne J , Walker T , Versace VL , Allender S , Nichols M , Backholer K , Goodwin N , Lewis S , Dalton H , Prael G , Curtin M , Brooks R , Verdon S , [...] Holliday S
Med J Aust , 213 Suppl 11:S3-S32.e1, 01 Dec 2020
Cited by: 9 articles | PMID: 33314144
Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas.
Crider K , Williams J , Qi YP , Gutman J , Yeung L , Mai C , Finkelstain J , Mehta S , Pons-Duran C , Menéndez C , Moraleda C , Rogers L , Daniels K , Green P
Cochrane Database Syst Rev , 2(2022), 01 Feb 2022
Cited by: 4 articles | PMID: 36321557 | PMCID: PMC8805585
Review Free full text in Europe PMC
The future of Cochrane Neonatal.
Soll RF , Ovelman C , McGuire W
Early Hum Dev , 150:105191, 12 Sep 2020
Cited by: 5 articles | PMID: 33036834
Effects of home telemonitoring interventions on patients with chronic heart failure: an overview of systematic reviews.
Kitsiou S , Paré G , Jaana M
J Med Internet Res , 17(3):e63, 12 Mar 2015
Cited by: 121 articles | PMID: 25768664 | PMCID: PMC4376138
Components of heart failure management in home care; a literature review.
Jaarsma T , Brons M , Kraai I , Luttik ML , Stromberg A
Eur J Cardiovasc Nurs , 12(3):230-241, 15 Jun 2012
Cited by: 19 articles | PMID: 22707520
Europe PMC is part of the ELIXIR infrastructure

IMAGES
VIDEO
COMMENTS
Although guidelines on optimal HF care exist, no specific description of components that are applied for optimal HF care at home exist. The objective of this review was to describe which components of HF (home) care are found in research studies addressing homecare interventions in the HF population. Methods: The Pubmed, Embase, Cinahl, and ...
Background. Patients with heart failure (HF) constitute a large group within health care worldwide. The prevalence of symptomatic HF is estimated to 2% of the population, approximately 15 million in Europe. 1 The mean age of HF patients is around 75 years and HF is a leading cause of hospitalization for elderly patients at high healthcare costs. 1 Patients with HF often need complex care due ...
The literature search identified 703 potentially relevant publications, out of which 70 articles were included. All articles described interventions with two or more of the following components: multidisciplinary team, continuity of care and care plans, optimized treatment according to guidelines, educational and counselling of patients and caregivers, and increased accessibility to care.
The objective of this review was to describe which components of HF (home) care are found in research studies addressing homecare interventions in the HF population.
Which components of HF (home) care are found in research studies addressing homecare interventions in the HF population, and aspects such as collaboration between primary care and hospital care, titration of medication, and patient education can be improved. Background: Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and ...
Background:Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and secondary care. Although guidelines on optimal HF care exist, no spe...
Search worldwide, life-sciences literature Search. Advanced Search Coronavirus articles and preprints Search examples: "breast cancer" Smith J
Background: Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and secondary care. Although guidelines on optimal HF care exist, no specific description of components that are applied for optimal HF care at home exist. The objective of this review was to describe which components of HF (home) care are found in research studies ...
Most studies (n=65, 93%) tested interventions with three components or more and 20 studies (29%) used interventions including all five components. Conclusions: There a several studies on HF care at home, testing interventions with a variety in number of components. Comparing the results to current standards, aspects such as collaboration ...
BACKGROUND: Patients with heart failure (HF) need long-term and complex care delivered by healthcare professionals in primary and secondary care. Although guidelines on optimal HF care exist, no sp ...
Background "Guidelines for the care of heart failure patients at home support safe and effective evidence-based practice. The aims of the present study were: [1] to identify guidelines addressing the care at home for adults with heart failure and [2] evaluate the quality of the guidelines and the extent to which they address eight components of home-based HF disease management." Methods A ...
Europe Home care nurses, clinicians Multidisciplinary not mentioned literature review, Survey of European heart failure management programmes, Opinion of re-searchers and practitioners Chronic heart failure in adults: diag-nosis and management NICE1(2018) Update 2018 [28] The National Collaborating Centre for Chronic Conditions/Na-tional ...
This website requires cookies, and the limited processing of your personal data in order to function. By using the site you are agreeing to this as outlined in our privacy notice and cookie policy.
Background. Home care workers (HCWs), which include home health aides and personal care aides, are increasingly used by heart failure (HF) patients for post-acute care and long-term assistance. Despite their growing presence, they have largely been left out of HF research and interventions. This systematic review was aimed to 1) describe ...
Practical guide on home health in heart failure patients. 2013 Nov 4;13:e043. doi: 10.5334/ijic.992. 24250283. PMC3821536. 10.5334/ijic.992. Introduction: Chronic heart failure is a common condition affecting up to 15 million people in the extended Europe. Heart failure is burdensome and costly for patients in terms of decreased quality of life ...
The purpose of this literature review is to evaluate the evidence supporting the effectiveness of home care monitoring for heart failure patients as a means of reducing hospital readmissions. The use of effective home care monitoring of heart failure patients will decrease the incidence of readmissions, increase patients the quality of life and ...
DOI: 10.1177/1474515112449539 Corpus ID: 36221697; Components of heart failure management in home care; a literature review @article{Jaarsma2013ComponentsOH, title={Components of heart failure management in home care; a literature review}, author={Tiny Jaarsma and Maaike Brons and Imke Kraai and Marie Louise A Luttik and Anna Stromberg}, journal={European Journal of Cardiovascular Nursing ...
The highest quality guidelines most relevant to the care at home of patients with HF are the "NICE" and "Adapting HF guideline for nursing care in home health care settings" and would be most appropriate for use by home healthcare nurses. Background "Guidelines for the care of heart failure patients at home support safe and effective evidence-based practice. The aims of the present ...
Chronic heart disease affects millions of people worldwide and the prevalence is increasing. By now, there is an extensive literature on outpatient care of people with chronic heart disease. We aimed to systematically identify and map models of outpatient care for people with chronic heart disease in terms of the interventions included and the outcomes measured and reported to determine areas ...
Background "Guidelines for the care of heart failure patients at home support safe and effective evidence-based practice. The aims of the present study were: [1] to identify guidelines addressing the care at home for adults with heart failure and [2] evaluate the quality of the guidelines and the extent to which they address eight components of home-based HF disease management."