- Open access
- Published: 26 May 2022

Structural changes in the Russian health care system: do they match European trends?
- Sergey Shishkin ORCID: orcid.org/0000-0002-0807-3277 1 ,
- Igor Sheiman ORCID: orcid.org/0000-0002-5238-4187 2 ,
- Vasily Vlassov ORCID: orcid.org/0000-0001-5203-549X 2 ,
- Elena Potapchik ORCID: orcid.org/0000-0001-7004-3100 1 &
- Svetlana Sazhina ORCID: orcid.org/0000-0002-2023-3384 1
Health Economics Review volume 12 , Article number: 29 ( 2022 ) Cite this article
6932 Accesses
3 Citations
2 Altmetric
Metrics details
In the last two decades, health care systems (HCS) in the European countries have faced global challenges and have undergone structural changes with the focus on early disease prevention, strengthening primary care, changing the role of hospitals, etc. Russia has inherited the Semashko model from the USSR with dominance of inpatient care, and has been looking for the ways to improve the structure of service delivery. This paper compares the complex of structural changes in the Russian and the European HCS.
We address major developments in four main areas of medical care delivery: preventive activities, primary care, inpatient care, long-term care. Our focus is on the changes in the organizational structure and activities of health care providers, and in their interaction to improve service delivery. To describe the ongoing changes, we use both qualitative characteristics and quantitative indicators. We extracted the relevant data from the national and international databases and reports and calculated secondary estimates. We also used data from our survey of physicians and interviews with top managers in medical care system.
The main trends of structural changes in Russia HCS are similar to the changes in most EU countries. The prevention and the early detection of diseases have developed intensively. The reduction in hospital bed capacity and inpatient care utilization has been accompanied by a decrease in the average length of hospital stay. Russia has followed the European trend of service delivery concentration in hospital-physician complexes, while the increase in the average size of hospitals is even more substantial. However, distinctions in health care delivery organization in Russia are still significant. Changes in primary care are much less pronounced, the system remains hospital centered. Russia lags behind the European leaders in terms of horizontal ties between providers. The reasons for inadequate structural changes are rooted in the governance of service delivery.
The structural transformations must be intensified with the focus on strengthening primary care, further integration of care, and development of new organizational structures that mitigate the dependence on inpatient care.
In the last two decades, health care systems in the European Union countries have faced global challenges, including aging populations, a substantial rise in chronic and multiple diseases, the emergence of new medical and information technologies, and a growing citizen awareness of the role of a healthy lifestyle in disease prevention [ 1 ]. The responses of health systems to these challenges included structural changes in their organization with a focus on the promotion of healthy lifestyles and disease prevention, the growing scale of screening for early disease detection, strengthening primary care, changing the role of the hospitals, the development of chronic disease management programs, etc. [ 2 , 3 ]
Studies of these trends address mostly Western countries. Much less attention has been paid to the post-Soviet countries. In this paper, we study structural changes in the health care in Russia. Russian health care has inherited the Semashko model of health care organization. Its main distinction is state-centered financing, regulation, and provision of health care. The model has specific forms of provider organization, for example, outpatient clinics (polyclinics) with a large number of various specialists, the separation of care for adults and children, and large highly-specialized hospitals [ 4 ].
The Soviet and post-Soviet health systems have been underfunded. Public health funding in the 1990s dropped almost by one third in real terms [ 5 ]. The organization of medical care in the 1990s has not changed significantly relative to Soviet times, and the system has adapted through the reduction in the volume of services and increased payments by patients, frequently informal [ 6 ]. The surge in oil prices after 2000 allowed health funding to increase and while encouraged noticeable changes in service delivery.
The changes in the Russian health system have been discussed in the literature mostly focusing on specific sectors and health finance reforms [ 5 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]. But these changes in different sectors were not analyzed together, from a single methodological position, as changes in the structural characteristics of the Russian health care system, i.e. the changes in the ratio of different types of medical care, in the structure of medical service providers, in functionalities and modes of their interaction.
The objective of this paper is to explore the entire complex of structural changes over the past two decades in comparison with European trends. What were the structural changes in European health care systems, what were they like in Russia, and how can their differences be explained?
Study design
We followed a six-step methodological framework. The first stage involved designation of the types of medical care and the types of structural changes for identification and comparison. We considered four main areas of medical care delivery: preventive activities, primary care, inpatient care, long-term care. We focused on three different dimensions of structural changes: i) changes in the organizational structure of medical service providers; ii) changes in the structure of their activities (in its types and in their coverage of the population / patients); iii) changes in the organization of interaction between different service providers.
The second stage consisted of identifying for each type of medical care the changes in these three dimensions in the last twenty years before the COVID-19 pandemic. We described the changes that met two criteria: 1) these changes are assessed in the OECD, WHO, and World Bank reviews, and other review publications on this topic as the most noteworthy characteristics of the development of European health care systems, and 2) they have spread in a large number of European countries.
The changes identified according to the formulated criteria cover not all dimensions of structural changes for each type of medical care. For preventive activities, there are changes in the types of activities and in their coverage of the population. In primary and inpatient care, there are changes in the organizational structure of service providers, in the structure of their activities, and in the organization of interaction with other providers. In long-term care, there are changes in the structure of developed activities and their coverage of the population.
To describe the ongoing changes, we use both qualitative characteristics and, if possible, quantitative indicators that highlight them to the greatest extent.
The third stage involved detection of structural changes in four main areas of medical care delivery in Russia. We used the results of our previous studies and conducted an additional search for data characterizing structural changes in health care, using new statistical data, evidence derived from our survey of physicians and interviews with top managers in medical care system.
On the fourth stage we compared the identified structural changes in European health care systems (HCS) with the changes taking place in Russian health care. We identified the presence or absence of similar types of structural changes and the differences between them. The fifth stage was the consideration of the driving forces of structural changes in the Russian health care system. The sixth stage included discussion of the reasons for the distinctions with European developments.
Data sources
To identify the main structural changes in medical care delivery during last twenty years we searched the literature addressing both European HCS and Russia in the all aspects of changes of health care system indicators, better classified by MeSH term “health care reform”. We searched MEDLINE using the query: (russia OR europ* OR “european union” OR semashko) AND health care reform [mh] AND 2000:2021[dp]). All 788 findings were checked manually and 86 were relevant. We also used sources snowballed from these reports and the grey literature related to Russian health care, including those in limited circulation, unpublished documents, memorandums, and presentations from our personal collections covering more than twenty years.
We also used data from an online survey of 999 primary care physicians (further – survey) conducted by the authors in April–May 2019. The respondents representing 82 out of 85 regions of the Russian Federation were asked about implementation of the national prophylactic medical examination program. We also interviewed four leading specialists of the national Ministry of Health on the criteria for the inclusion of the components into the program.
To identify the driving forces of structural changes in the Russian health care system, we used materials from 10 interviews on the issues of implementing state health care programs that we conducted in 2019 with current and former top-managers in the federal government and in five regional governments. We also used the grey literature as well as published reports.
We used statistical data from the international databases of OECD [ 18 ], WHO [ 19 ], World Bank [ 20 ], as well as the Russian sources — the Federal State Statistics Service [ 21 ] and the Russian Research Instuitute of Health [ 22 ]. The data was analyzed for the period from 2000 to the latest date with available data for both EU member states and Russia. To ensure the comparability of the composition of countries in different years, the analysis of the dynamics of some indicators was limited to EU 19 members, i.e. excluding Cyprus, Greece, Croatia, Bulgaria, Luxemburg, Malta, Netherland, Poland, and Romania. The averages for EU 19 estimates are based on population size-weighted averages. If the studied publications and databases did not contain the necessary indicators, we made our own estimates.
Each section of the paper contains a brief description of the main trends in the European countries, and then provides a comparative analysis of the corresponding changes in Russian health care. The comparison is followed by a discussion of the driving forces and the limitations of structural changes in Russia compared to the main European trends. We limited our analysis to the pre – COVID-19 pandemic years.
The development of preventive activities
European hcs.
Most of them have implemented health check-ups, and population and opportunistic screenings for the early detection of diseases. These activities are viewed as a way to improve outcomes by ensuring that health services can focus on diagnosing and treating disease earlier [ 23 ]. The population covered by screenings is high and growing. In Germany 81% of population between 50 and 74 years in 2014 had been tested for colorectal cancer at least once, in Austria 78%, France 60%, Great Britain 48% [ 24 ].
The impact of these activities on health outcomes depends on the selection of preventive services, as well as on their implementation in specific national contexts. The selection of preventive services is increasingly based on research into their potential impact on mortality and other health indicators, as well as their cost effectiveness, with some services being declined because of their inadequate input into health gains [ 25 ]. It is particularly important that screenings are focused on socially disadvantaged groups with the highest probability of disease identification and the expected benefits of their management. Therefore, screening programs are based on the evaluation of local needs. Physicians have discretion in the choice of patients for screenings, depending on their importance for specific groups of the population, and individual risks and preferences.
It is increasingly common for a screening program to include follow-up management of any detected illnesses, with the implication that policy makers design such programs as a set of interrelated preventive and curative activities [ 26 ].
The original Semashko model and the current legislation prioritize preventive activities, while their implementation has been limited by the chronic underfunding of the health system. In the 2000s, the priority of prevention campaigns was revitalized in the form of a national prophylactic medical examination program (Prophylactic Program, called Dispanserization) that is a set of health check-ups and screenings. The major expectation from this Prophylactic Program is the same as in European HCS [ 27 ].
To supplement the analysis of the Prophylactic Program, we analyzed the evidence base for the components of the program and interviewed leading specialists of the federal Ministry of Health on the criteria for the inclusion of the components into the program. We found that some screenings were not evidence based and effect on the population health and/or health of participants is small [ 28 ]. The screening package of the dispanserization was expanded and reduced couple of times, but still number of ineffective screenings are included in the package (electrocardiography (ECG) screening of healthy subjects, prostate specific antigen (PSA) screening of middle age and adult men, urinalysis and routine blood tests, mammography from age 40 etc.).
Primary care physicians play a major role in conducting screenings and check-ups as well as subsequent interventions. There are also public health units responsible exclusively for these preventive activities in big polyclinics. Polled in 2019, primary care physicians responded that in 11% of polyclinics check-ups are carried out in these departments only, and in 24% of primary care organizations the check-ups are conducted by district physicians as well as by staff of these preventive units.
Under the current Prophylactic Program, people over 40 are supposed to have a set of check-ups annually; those 18–39 every three years. Most children go through physicals only. The official estimates of the coverage of the eligible population in the Prophylactic Program are around 100% [ 29 ], while service providers are less optimistic. According to the survey, more than half of the respondents reported that this share was less than 60%, while 17.4% reported less than 20% [ 27 ].
An important shortcoming of the Prophylactic Program design and implementation is the gap between its major objective and the capacity of primary care. The shortage of primary care physicians does not allow the target groups to be provided with all preventive services. Physicians have to distort the service to their registered population and to underprovide the follow-up care of detected cases. The lack of a systematic approach, less focus on local conditions, and the lack of a professional autonomy of providers are the major distinctions between Russian prevention campaigns and similar activities in Europe.
The Prophylactic Program is built on the presumption that preventive activities should include the follow-up management of any detected conditions. There is some evidence, however, that this is not taking place: according to our survey, a half of primary care physicians are unaware of the results of check-ups and screenings. The reported coverage and quality of the follow-up management of identified cases are low: a half of the respondents indicate that less than 60% of patients with identified diseases become objects of the follow-up disease management. Only 7.7% of respondents indicate that a set of disease management services corresponds to a pattern of dispensary surveillance issued by the federal Ministry of Health. The majority reports that these requirements are met only for some patients or are not met at all.
Disease management of newly identified chronic and multiple cases is focused on process rather than outcome indicators. The information on the latter is very fragmented. According to our survey, a decrease in the number of disability days of chronic patients is reported by only 14% of physicians. More than a half of respondents are unaware of the number of emergency care visits and hospital admissions of their chronic patients.
Strengthening primary care
There is a trend of multi-disciplinary primary care practices or networks development and promotion of teamwork and providers coordination in response to the growing complexity of patients. In Spain, France, and the UK it is increasingly common for large general practices to serve more than 20,000 people and provide a wider spectrum of services than in traditional solo and group practices. These emerging extended practices include pharmacists, mental care professionals, dieticians, and sometimes 2–3 specialists [ 30 , 31 ]. The role of nurses is also expanding. Most advanced nurses independently see patients, provide immunizations, health promotion, routine checks for chronically ill patients in all EU member states [ 32 ]. Related to these extended practices is the growing concentration of primary care providers via mergers and reconfigurations that increase the size of the units. The major benefits are economies of scale and scope through staff sharing and better integrated care.
There is also a general trend to strengthen the links with the local community, social care and hospitals [ 32 ]. Primary care providers are increasingly involved in chronic disease management programs together with other professionals in and out of general practices. Links with hospitals are developing beyond simple referral systems [ 33 ].
The trend of multidisciplinary practices development has greatly affected Russian health care. However, this trend in Russia differs significantly from the European HCS. It began in the 1980s, when large numbers of specialists were employed by polyclinics, which are the major providers of both primary care and outpatient specialty care. Today, large urban polyclinics employ 15–20 categories of specialists, and polyclinics in small towns 3–5 categories. The generalist who serves for the catchment area (district doctors) is limited in the scope of services they provide. Multidisciplinary practices are built through employing new specialists, while in European countries mainly through nurses and other categories of staff. Specialists in Russian polyclinics do not supplement, but essentially replace district doctors: they accounted for 66% of visits in 2019. Footnote 1
The scope of district doctors’ services is limited: at least 30–40% of initial visits end with referrals to a specialist or to a hospital, while in Europe only 5–15% [ 35 , 36 ]. Gatekeeping is promoted, but district doctors are overloaded and not interested in expanding the scope of their services. Specialists in polyclinics have insufficient training and poorly equipped, e.g. urologists do not do ureteroscopy and ophthalmologists do not practice surgery.
Since the 1990s, some regions started replacing district doctors and pediatricians with general practitioners. But this initiative has not been supported by the federal Ministry of Health, therefore the institution of a general practitioner is not accepted throughout the country. Currently, the share of general practitioners in the total number of generalists serving a catchment area is only 15% (Fig. 1 ). The model of general practice is used only in some regions. The main part of the primary care in the country is provided by district doctors and pediatricians, whose task profile remains narrower than that of general practitioners. The division of primary care for children and adults is preserved. The family is not a whole object of medical care. This division is actively defended by Russian pediatricians with references to specific methods of managing child diseases.
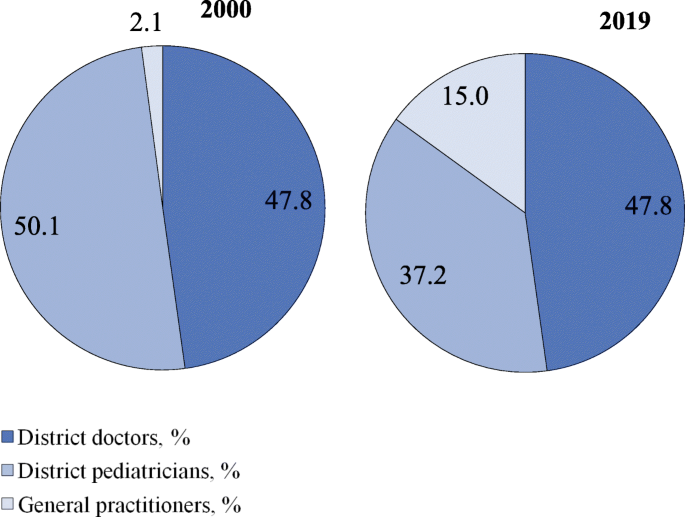
Distribution of generalists in Russia by categories in 2000, 2019. Source: Calculated from RRIH [ 22 , 37 ]
The prevailing trend in all European HCS is to increase the role of nurses. In Russia, the participation of nurses in medical care is limited to fulfilling doctors’ prescriptions and performing ancillary functions.
The transformation of inpatient care
Due to increased costs, technological advances in diagnosis and treatment, there were changes in patterns of diseases and patients treated in hospitals. A substantial amount of inpatient care has been moved to outpatient settings with a respective decrease in bed capacity. This is an almost universal trend in European HCS [ 19 ].
Hospitals continue to be centers of high-tech care, which concentrate most difficult cases and intensify inpatient care with a corresponding decrease in the average length of stay. These changes have been promoted by the move to diagnostic related groups based payment systems and a growing integration with other sectors of service delivery.
In many European countries, most hospitals no longer act as discrete entities and have become units of hospital-physician systems which are multi-level complex adaptive structures [ 3 ]. A new function of hospital specialists is their involvement in chronic disease management in close collaboration with general practitioners, outpatient specialists, and rehabilitative and community care providers [ 38 ].
Over the past two decades the treatment of relatively simple cases and preoperative testing have gradually moved to day care wards and polyclinics. In annual health funding, the federal government sets decreasing targets of inpatient care which are obligatory and which regions use to plan their inpatient care. However, inpatient care discharges per 100 people have been almost stable (21.9 in 2000 and 22.4 in 2018) in contrast to the EU 19 members Footnote 2 (18.4 in 2000 and 16.9 in 2018) [ 18 ]. The pressure of decreasing targets resulted in a drop in the average length of hospital stays (Fig. 2 ) and the total bed-days per person (Fig. 3 ). These indicators, along with bed supply (Fig. 4 ), decreased even faster than in the EU.
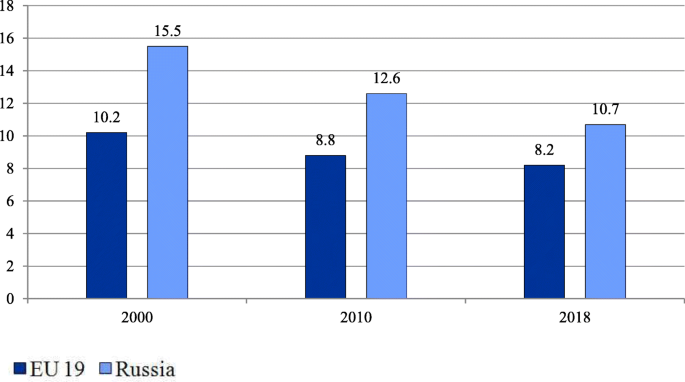
Average length of stay in hospital in EU members and Russia (days). Note: Calculated for EU 19 member states (see Methods). The EU 19 average length of hospital stay estimates are calculated as the sum of the products of inpatient care discharges by the average length of stay for each country, weighted average by the total inpatient care discharges. Source: OECD Health Statistics [ 18 ]
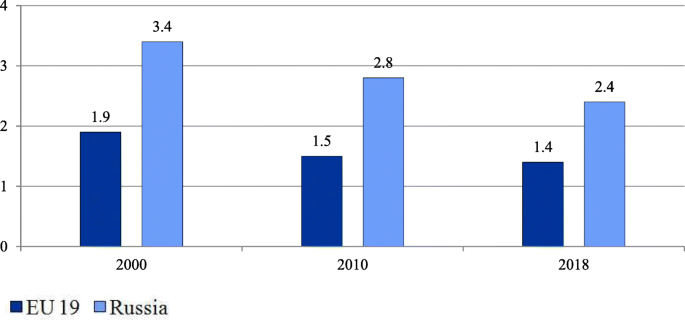
Number of bed-days per person in the EU and Russia. Note: Calculated for EU 19 member states (see Methods). EU 19 estimates are calculated as the sum of the products of inpatient care discharges by the average length of stay for each country weighted by the total population. Source: OECD Health Statistics [ 18 ]

Hospital beds per 1000 people in the EU and Russia. Note: Calculated as the average for all EU 28 members weighted by the total population. Source: World Bank [ 20 ]
At the same time, the intensity of medical care processes in hospitals in Russia remains significantly lower than in European countries. An indicator of this is the gap in the number of hospital employees per 1000 discharged (Table 1 ).
Over the past 20 years, significant efforts have been made to deploy day wards, both in hospitals and polyclinics, to reduce the burden on hospitals. As a result, the proportion of patients treated in day wards in the total number of patients treated in hospitals increased from 7.6% in 2000 to 20.8% in 2016 [ 21 ]. However, there is fragmentary evidence that this figure is still noticeably lower than in Europe. The share of cataract surgery carried out as ambulatory cases varies in most European countries between 80 to 99% [ 24 ] but is negligible in Russia.
Despite these positive trends, the health system remains hospital centered. The number of bed-days per person remains nearly twice as high as the EU average (Fig. 3 ).
An important trend is the increasing concentration of hospitals. The number of hospitals halved between 2000 and 2018, mostly due to mergers, but also due to the closures of inadequately equipped hospitals. This process has led to an increase in the average size of hospitals from 156 beds in 2000 to 223 beds in 2018 [ 21 ]. This figure is higher today than in Western countries with large territories. The average hospital size in France was 130 beds in 2018 and in Germany 215 beds in 2017 [ 18 ]. In Russia, with its very low population density, the reduction in the number of small rural hospitals resulted in some accessibility problems.
At the same time, the incorporation of previously independent polyclinics into hospitals is under way. The proportion of independent polyclinics in the total number of polyclinics has decreased from 35% in 2000 to 19% in 2014 [ 36 ].
The development of long-term care
Over the last 20 years, most European countries have increasingly developed the public provision of long-term care. The number of nursing and elderly home beds per 100,000 people in the EU increased from 581.7 in 2000 to 748.3 in 2014 [ 19 ], although the pace of changes, the coverage of citizens in need of long-term care, and its organization and funding differ substantially across countries [ 39 ]. Many countries control costs by keeping people in their homes longer and shifting the responsibility for non-institutional forms of care to communities [ 40 ]. An expected outcome of investment in long-term care is the reduction of informal care utilization.
Compared to European HCS, long-term care is underdeveloped in Russia. The number of nursing care beds declined from 14.7 per 100,000 people in 2011 to 10.6 in 2019 [ 22 ]. The share of citizens over working age and people with disabilities receiving outpatient and inpatient care within the long-term care system in the total number of citizens over working age and people with disabilities in need of long-term care, was only 2.9% in 2019 [ 41 ].
In contrast to the European HCS, Russia has not built a strong long-term care sector with the capacity to reduce the workload of acute inpatient care settings. Hospitals have to keep some patients longer resulting in a relatively higher length of stay. Palliative care as another sector of the long-term care which started to develop only a few years ago.
Driving forces and tools of structural changes in the Russian health care system
These changes have been driven by the federal and regional governments. They use two main tools to manage structural changes: 1) setting health care targets for the entire country and for regions, and 2) implementing vertical health care programs.
Since 1998, the federal government has annually approved a program of benefit packages for health (the Program). It sets targets for the utilization of medical care for each sector of service delivery, as well as unit cost targets. The Program is designed to balance the volumes of care with the amount of public funding. The annual versions of the Program gradually reduced the targets for inpatient care to encourage a shift to outpatient care. The federal targets are used in regional health planning. In the first decade of using the Program, the changes in the actual volume of medical care were small, but in the second decade, pressure from the federal center on the regions increased, and the gap between the federal targets and the actual utilization of care has noticeably narrowed (Table 2 ).
The development of the legislation on the delimitation of responsibility between levels of government, carried out in the last two decades, has consistently strengthened the regional governments role in restructuring medical care delivery. In 2012, almost all resources of health care governance were transferred from the municipal to the regional level (including the governance of primary health care. During the period 2000–2019 the number of public hospitals has decreased by 2.2 times, the number of hospital beds by 1.5 times, polyclinics 1.3 times, feldsher-obstetric posts 1.3 times. Footnote 3
When oil prices increased, the federal government poured additional resources into vertical programs. They are administered by the federal Ministry of Health and regional governments. The major programs: the ‘Priority national health project’ (2004–2012), the Prophylactic Program (2008 – ongoing), and regional programs for the modernization of health care (2011–2013). All additional and some basic resources are earmarked in an attempt to develop the highest priority activities: preventive care, obstetric care, cardiovascular surgery, oncology, etc.
The role of the centralized administration of these priority programs is controversial. The federal government initiated them, provided regions with additional funding, and made the program’s targets a priority of health policy. According to interviews with federal and regional officials, the implementation of programs is heavily controlled by the federal government: practically all decisions on specific activities, target indicators and resource allocation are approved on the federal level. The Russian regions have low flexibility to respond to local needs such as variation in disease incidence, the capacity of health care, or vulnerable population groups.
Structural changes in the provision of inpatient care were prompted by the introduction of a diagnostic related groups based payment system in the early 2010s. This was initiated by the federal government and implemented with the participation of the World Bank experts. It makes more profitable for hospitals to reduce the duration of hospitalizations and to complicate the structure of inpatient treatment [ 44 ].
We found that despite significant differences in health care organization, some structural changes in Russia have followed the general European trends. A similar rise in the coverage of the population with screenings is underway in Russia. There is a clear tendency to replace some inpatient care with day care. The volume of inpatient care is reducing —mostly due to a significant decrease in the length of stays, while the rate of hospital admission remains relatively stable. As in the most European HCS, the concentration of medical organizations and the formation of large outpatient and inpatient complexes is developing.
However, there are some substantial differences: the development of prevention programs is relatively less focused on the most vulnerable target groups and on local needs; primary care specialization is much stronger than in European HCS; the role of first contact generalists is waning; the worldwide tendency of increasing the role of nurses is almost invisible in Russia; long-term care is starting to develop but is still at a very low level and palliative care is in its infancy; integration in the health system are much less pronounced—both at the level of individual medical organizations and between health sectors.
The reasons for these differences are rooted in the specific features of health governance in Russia.
The Semashko model, by virtue of its genesis, reproduces the state administration patterns of a planned economy. The main driving force of changes is the bureaucracy. Its managerial activities are guided by the mechanism described by J. Kornai: ‘postponement, putting out the fire, postponement’ [ 45 ]. The governance focuses on mobilizing and distributing available resources to solve or mitigate the most pressing problems - ‘fire fighting’. This is what determines the fragmentation of structural changes in Russian health care compared to structural changes in European countries.
Materials of interviews with heads of federal and regional health authorities suggest that in the existing governance system each of its levels must demonstrate the success of its activity exclusively to the higher levels of management. It is easier to achieve success when solving problems of optimizing the volume of medical care and the organizational structure of medical institutions, and much more difficult when solving problems of improving the efficiency of all elements of medical care system, which requires changes in their functionality and ways of interaction. It requires more financial resources and better management at all levels of health governance.
A number of deeply rooted limitations for carrying out structural transformations in Russian health care can be highlighted.
Firstly, the low capacity of primary care providers and to some extent the unwillingness of patients to replace inpatient care with outpatient treatment prevents a shift of patients from hospitals to polyclinics.
Secondly, a feature of the Russian health care system is the weak development of horizontal links between medical organizations related to different levels of medical care, and between medical workers within medical organizations working in different departments [ 36 , 46 , 47 ]. The interaction of different providers is carried out mostly through vertical channels. This is a serious obstacle to the development of horizontal integration [ 36 ].
Thirdly, democratic institutions for the development of health care are historically underdeveloped in Russia and this influences the choice of health policy priorities. According to interviews with heads of regional health authorities, the role of local communities is negligible, and the role of the medical community is marginal. Professional organizations are rarely involved in decision-making on health issues. The input of public councils to government bodies is largely imitative. Information about the activities of the system as a whole and of individual medical organizations is restricted for public use. This enables health authorities to focus on achievements in their reports, while hiding shortcomings. Feedback from patients, and society as a whole, is poorly expressed.
Conclusions
Russian health care, whose genetic basis was the Soviet Semashko model, after a difficult ‘survival’ period in the 1990s, underwent significant structural changes over the next two decades. To a large extent, the directions of these changes have coincided with European trends. The prevention and the early detection of diseases have developed intensively. The reduction in hospital bed capacity and inpatient care was accompanied by an intensification of inpatient treatment and a decrease in the average length of stay. Russia has followed the European trend of service delivery concentration in hospital-physician complexes, while the increase in the average size of hospitals is even more substantial. Structural changes in primary care are much less pronounced. The resources and competences of providers and the governance of primary care are still not enough to abolish the hospital-centered model of service delivery. Russia has intensively implemented vertical health care programs to develop the priority activities, but still significantly lags in the level of development of horizontal ties among services providers.
Specific structural changes in Russia are rooted in the organization and governance of service delivery. The interests of federal and regional bureaucracies, which act as the main drivers of changes, are pushing them to prioritize the changes in volumes of medical care and organizational structure of health care providers and not spend a lot of effort on improving their functionality and modes of interaction between providers of medical care. An important role is also played by the low capacity of primary care units to provide quality care.
To respond effectively to modern global challenges, reduce mortality, and improve the health of the population, structural transformations in Russian health care must be intensified with the focus on strengthening primary care, the further integration of care, and an accelerated development of new structures that mitigate the dependence on inpatient care.
Availability of data and materials
The data used and analysed during the current study are publicly available.
Calculated using data from [ 34 ].
See Methods.
Calculated using data from [ 21 ].
Abbreviations
European Union
Health Care System
Organization for Economic Co-operation and Development
World Health Organization
World Health Organization. Better Health for Europe: more equitable and sustainable. Copenhagen: WHO; 2019. https://apps.who.int/iris/bitstream/handle/10665/327427/9789289054225-eng.pdf . Accessed 9 Mar 2021.
Kringos D, Boerma W, Bourgueil Y, et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract. 2013;63(616):e742–50. https://doi.org/10.3399/bjgp13X674422 .
Article PubMed PubMed Central Google Scholar
McKee M, Merkur S, Edwards N, Nolte E, eds. The changing role of the Hospital in European Health Systems. European Observatory on Health Systems and Policies. Cambrige University Press; 2020. https://www.euro.who.int/__data/assets/pdf_file/0010/448048/Changing-role-of-hospitals-eng.pdf . Accessed 11 Feb 2021.
Davis C. Priority and the shortage model: the medical system in the socialist economy. In: Davis C, Charemza W, editors. Models of disequilibrium and shortage in centrally planned economies. London: Chapman and Hall; 1989. p. 427–59.
Chapter Google Scholar
Shishkin S. Russia’s health care system: difficult path of reform. In: Alexeev M, Weber S, editors. The Oxford handbook of the Russian economy. Oxford: Oxford University Press; 2013. p. 748–74.
Google Scholar
Shishkin SV, Vlassov VV. Russia's healthcare system: in need of modernisation. BMJ. 2009;338:b2132. https://doi.org/10.1136/bmj.b2132 .
Rese A, Balabanova D, Danishevski K, McKee M, Sheaff R. Implementing general practice in Russia: getting beyond the first steps. BMJ. 2005;331(7510):204–7. https://doi.org/10.1136/bmj.331.7510.204 .
Human Rights in Patient Care. Stockholm Region Office in St.Petersburg. Russian Healthcare System Overview. St. Petersburg, 2010. 2010. https://health-rights.org/index.php/cop/item/russian-healthcare-system-overview . Accessed 29 Nov 2020.
Gordeev VS, Pavlova M, Groot W. Two decades of reforms. Appraisal of the financial reforms in the Russian public healthcare sector. Health Policy. 2011;102(2-3):270–7. https://doi.org/10.1016/j.healthpol.2010.08.009 .
Popovich L, Potapchik E, Shishkin S, Richardson E, Vacroux A, Mathivet B. Russian Federation: health system review. Health Syst Transit. 2011;13(7):1-190, xiii-xiv.
PubMed Google Scholar
Bochkareva VK. Health-care reform and ensuring equal access to free medical services. Probl Econ Transit. 2013;55(12);12-31. https://doi.org/10.2753/PET1061-1991551203 .
Sheiman I, Shevski V. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy. 2014. https://doi.org/10.1016/j.healthpol.2013.12.011 .
Kontsevaya A, Sabgaida T, Ivanova A, Leon DA, McKee M. How has the management of acute coronary syndrome changed in the Russian Federation during the last 10 years? Health Policy. 2017;121(12):1274-9. https://doi.org/10.1016/j.healthpol.2017.09.018 .
Tagaeva TO, Kazantseva LK. Public health and health Care in Russia. Probl Econ Transit. 2017;59(11-12):973-90. https://doi.org/10.1080/10611991.2017.1431488 .
Belova N. Health Care in Rural Areas. Sociol Res. 2018;57(2):123-35. https://doi.org/10.1080/10610154.2018.1577621 .
Sheiman I, Shishkin S, Shevsky V. The evolving Semashko model of primary health care: the case of the Russian Federation. Risk Manag Healthc Policy. 2018;11:209-20. https://doi.org/10.2147/RMHP.S168399 .
Somanathan A, Sheiman I, Salakhutdinova S, Buisman L. Universal health coverage in Russia: extending coverage for the poor in the post-soviet era. Universal health coverage study series. Washington, DC: Universal Health Coverage Study Series The World Bank Group; 2018. p. 37. https://openknowledge.worldbank.org/handle/10986/30026 . Accessed 10 Mar 2021.
OECD. Health Statistics. OECD; 2020. https://stats.oecd.org/Index.aspx?ThemeTreeId=9 . Accessed 01 Dec 2020.
World Health Organization (WHO). European Health for All database (HFA-DB). WHO; 2020. https://gateway.euro.who.int/ru/datasets/european-health-for-all-database/ . Accessed 29 Nov 2020.
World Bank. World Bank Open Data. The World Bank Group, 2020. https://data.worldbank.org/ .
Federal State Statistics Service website (Rosstat). Health care in Russia. Moscow: 2020. https://rosstat.gov.ru/folder/210/document/13218 . Accessed 02 Dec 2020.
Russian Research Institute for Health (RRIH). Health statistics. Moscow: 2020. https://mednet.ru/napravleniya/mediczinskaya-statistika . Accessed 29 Nov 2020.
International Agency for Research on Cancer. Cancer Screening in the European Union. Report on the implementation of the Council Recommendation on cancer screening. Lyon: European Commission; 2017. https://ec.europa.eu/health/sites/default/files/major_chronic_diseases/docs/2017_cancerscreening_2ndreportimplementation_en.pdf . Accessed 19 Dec 2020.
OECD. Health at a Glance 2019: OECD Indicators. Paris: OECD Publishing; 2019.
Book Google Scholar
McKee M, Rechel B. Screening. In: Rechel B and McKee M eds. Facets of public health in Europe. WHO Observatory for health systems and health reforms. Berkshire: Open University Press; 2014. https://www.euro.who.int/__data/assets/pdf_file/0003/271074/Facets-of-Public-Health-in-Europe.pdf . Accessed 21 Mar 2021.
Sagan A, McDaid D, Rajan S, Farrington J, McKee M. Screening: When is it appropriate and how can we get it right? European Observatory on health systems and health reforms. European Observatory Policy Brief. 35. Copenhagen, 2020. https://apps.who.int/iris/bitstream/handle/10665/330810/Policy-brief-35-1997-8073-eng.pdf . Accessed 20 Apr 2021.
Sheiman IM, Shishkin SV, Shevsky VI, Sazhina SV, Ponkratova OF. Regular medical check-ups in Russia: expectations and reality. Mir Rossii. 2021;30(4):6-29. https://doi.org/10.17323/1811-038X-2021-30-4-6-29 .
Rebrova OI, Fedyaeva VK, Omel'ianovskiĭ VV, Ilyin MA. Stage 1 screenings of periodical health check: a systematic review of long-term efficiency. Profilakticheskaya Meditsina. 2017;20(3):55-59. https://doi.org/10.17116/profmed201720355-59 .
Federal Fund of Mandatory Health Insurance. Report about the mandatory health insurance system activity in the Russian Federation in 2019. Mandatory Med Insur Russian Federat. 2020;4:22.
Dedeu T, Marti T. Multiprofile primary health care teams in Catalonia, Spain: a population-based effective model of service delivery. WHO; 2018. https://www.euro.who.int/__data/assets/pdf_file/0009/366498/HSS-NCDs-Policy-brief-cat.pdf . Accessed 15 Feb 2020.
Kumpunen S, Curry N, Farnworth M, Rosen R. Collaboration in general practice: surveys of GP practice and clinical commissioning groups. Nuffield trust, Royal College of General Practitioners; 2017. https://www.nuffieldtrust.org.uk/files/2017-10/collaboration-in-general-practice-2017-final.pdf . Accessed 20 Dec. 2020.
OECD. Realizing the full potential of primary care. Policy Brief. OECD; 2019. https://www.oecd.org/health/health-systems/OECD-Policy-Brief-Primary-Health-Care-May-2019.pdf . Accessed 11 Dec 2020.
Damiani G, Pascucci D, Sindoni A, et al. The bigger, the better? A systematic review on the impact of mergers on primary care organizations. Eur J Pub Health. 2021;31(2):244-52. https://doi.org/10.1093/eurpub/ckaa248 .
The Ministry of Health of the Russian Federation. The accounting form No. 30 of the Federal Statistical Surveillance for 2019 (raw data) (not in the public domain).
Kringos DE, WGW B, Hutchinson A, Saltman R. Building primary Care in a Changing Europe. Eur Observ Health Syst Health. Observatory Studies Series. 2015;38;172.
Sheiman I, Shevsky V. Concentration of health care providers: does it contribute to integration of service delivery? Risk Manag Healthc Policy. 2019;12:153-66. https://doi.org/10.2147/RMHP.S205905 .
Rugol LV, Son IM, Starodubov VI, Pogonin AV. Some results of healthcare reforming. Soc Aspects Popul. Health. 2021;67(1):4. https://doi.org/10.21045/2071-5021-2018-64-6-1 .
Article Google Scholar
Urbanski D, Reichert A, Amelung V. Discharge and Transition Management in Integrated Care. In: Amelung V, Stein V, Goodwin N, Balicer R, Nolte E, Suter E, editors. Handbook Integrated Care; 2017. p. 97–111.
Hernández-Quevedo C, Maresso A, Merkur S, Quentin W, Richardson E, Ginneken E. 20 years of health system reforms in Europe: what’s new? Eurohealth. 2018;24(2):23–8.
Spasova S, Baeten R, Vanhercke B. Challenges in long-term care in Europe. Eurohealth. 2018;24(4):7–12.
The presidium of the presidential Council for the Strategic Development and Priority Projects. The Federal Project ‘the senior generation’. Protocol No 16 dated December 24, 2018. The Ministry of Labour and Social Protection; 2018. https://mintrud.gov.ru/ministry/programms/demography/3 . Accessed 15 Nov 2020.
Government of the Russian Federation. Resolutions of the government of the Russian Federation ‘on the program of the state guarantees of free provision of medical care to Citizens’ 1998–2018. The Federal Compulsory Medical Insurance Fund. 2018. https://www.ffoms.gov.ru/system-oms/about-fund/questions-oms/programm-gos-guarantee/ . Accessed 11 Sept 2021.
The Ministry of Health of the Russian Federation. Reports on the implementation of the program of the state guarantees of free provision of medical care to Citizens, 1999–2019. Moscow: The Ministry of Health of the Russian Federation, 2000-2019.
Avxentyeva MV, Omelyanovskiy VV, Petrovskiy AV, et al. New approaches to the development of diagnostic related groups for Cancer pharmacotherapy in Russian Federation. Med Technol Assess Choice. 2018;2(32):8–22.
Kornai J. Economics of shortage. Amsterdam: Elsevier Science. 1980.
Kuhlmann E, Shishkin S, Richardson E, et al. Understanding the role of physicians within the managerial structure of Russian hospitals. Health Policy. 2019;123(8):773-81. https://doi.org/10.1016/j.healthpol.2019.05.020 .
Sazhina SV, Shevsky VI, Sheiman IM, Shishkin SV. Interaction of health care providers: physicians' survey outcomes. Soc Aspects Popul Health. 2021;67(1):4 http://vestnik.mdnet.ru/content/view/1230/30/lang,ru/ .
Download references
Acknowledgements
Authors’ information (optional).
Sergey Shishkin – DSc in Economics, Director, Centre for Health Policy, HSE University.
Igor Sheiman – PhD in Economics, Professor, Health Economics and Management Department, HSE University.
Vasily Vlassov – DSc in Internal Diseases, Professor, Health Economics and Management Department, HSE University.
Elena Potapchik – PhD in Economics, Leading Research Fellow, Centre for Health Policy, HSE University.
Svetlana Sazhina – MPA, Leading Analyst, Centre for Health Policy, HSE University.
The study was funded by the grant provided by the Ministry of Science and Higher Education of the Russian Federation (Grant Agreement No. 075–15–2020-928).
Author information
Authors and affiliations.
Centre for Health Policy, National Research University Higher School of Economics, 4 Slavyanskaya Ploshchad, Building 2, Moscow, Russia, 109074
Sergey Shishkin, Elena Potapchik & Svetlana Sazhina
Department of Health Care Administration and Economics, School of Politics and Governance, Faculty of Social Sciences, National Research University Higher School of Economics, 20 Myasnitskaya Ulitsa, Moscow, Russia, 101000
Igor Sheiman & Vasily Vlassov
You can also search for this author in PubMed Google Scholar
Contributions
Sergey Shishkin conceptualized, designed the study and supervised the work. All authors collected, analyzed and interpreted the data. Elena Potapchik, Svetlana Sazhina made statistical analysis. Sergey Shishkin, Igor Sheiman and Vasily Vlassov wrote a first draft of the manuscript. All authors critically reviewed the draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sergey Shishkin .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shishkin, S., Sheiman, I., Vlassov, V. et al. Structural changes in the Russian health care system: do they match European trends?. Health Econ Rev 12 , 29 (2022). https://doi.org/10.1186/s13561-022-00373-z
Download citation
Received : 19 January 2022
Accepted : 05 May 2022
Published : 26 May 2022
DOI : https://doi.org/10.1186/s13561-022-00373-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care system
- Health service provision
- Primary care
- Inpatient care
- Structural changes
- Semashko model
Health Economics Review
ISSN: 2191-1991
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Russia’s Health Care System, Demographics Present Unique Advantages, Disadvantages in Fighting COVID-19

Russia has responded to the pandemic by drawing on some of its useful experience controlling tuberculosis, but suffers from the weaknesses of an imperfectly reformed health system.
The coronavirus hit Russia late, but is now gathering steam. This week, identified cases have been increasing by around 6,000 daily. As elsewhere, we can assume that unidentified infections are spreading much faster. How has Russia reacted? Among other things Russia has responded by drawing on some of its useful experience controlling tuberculosis since the collapse of the Soviet Union, by suffering from the weaknesses of an imperfectly reformed health system and by seeing control efforts undercut by a legacy of inadequate and unevenly distributed medical facilities.
Russia has been testing aggressively—over 3.49 million tests had been run as of April 30, which represents about 2.4 percent of the population. This is roughly equal to testing rates in Ukraine, lower than those of the Baltics and significantly higher than the rest of the post-Soviet space, Poland and Hungary. (For comparison, consider that the United States testing rate is 1.9 percent; the top tester is Iceland with 13.9 percent, and a hard-hit country like Italy has a testing rate of about 3.2 percent.)
In addition, Russia’s longstanding experience with tuberculosis, both during and after the Soviet Union, may give it an edge in setting up systems to test, treat and contain the spread of the virus. The collapse of the Soviet Union led to a spike in TB cases that remains an issue today, particularly as far as multiple drug resistant TB (MDR-TB) is concerned. To deal with the problem, Russia re-introduced a regime of extensive testing and monitoring of patients. Some regions also introduced highly effective community outreach programs that provided better contact tracing. Unlike COVID-19, TB is concentrated in vulnerable populations like the homeless. However, both COVID-19 and TB are highly infectious diseases that spread through the air, and Russia’s experience in bringing down TB rates by 5-6 percent per year suggests that the country has the capacity to tackle a highly infectious disease.
Russia and other Eurasian (and Asian) countries may also have another TB-related advantage: they continue to vaccinate their populations with the BCG vaccine that is effective against severe cases of childhood tuberculosis. Although the World Health Organization (WHO) reported in April that BCG doesn’t appear to offer protection against coronavirus infection, some scientists hypothesize that the lower than expected number of cases in Asia and Africa might be a side-effect of comprehensive BCG vaccination programs. This theory will have to be tested over time by comparing the incidence of COVID-19 in vaccinated and unvaccinated populations across the pandemic.
Another advantage that Russia enjoys according to some of its Western peers in fighting the disease, which disproportionally kills older people, is the younger age of its population The average age in Russia is 38 compared to 40 in the U.S. and 47 in Italy. Especially in Moscow, Russian COVID-19 cases are skewing younger than we have seen elsewhere. This may be explained by the fact that it is easier to access public or private testing in the capital, but it also reflects Russia’s younger population. It may also be the result of the fact that self-isolation has not been possible for construction workers , employees in isolated work sites in the far north and east, prisoners and doctors (including in the Komi Republic, St. Petersburg and Ekaterinburg ); these groups have been at the heart of a number of COVID-19 clusters, and tend to be of working age. Moreover, given that Russian men have significantly lower life expectancy than women (67 years versus 77 years) and that men appear to succumb more readily to the coronavirus, Russia’s unfavorable demographics may play in its favor when it comes to the pandemic.
At the moment, the epicenter of the Russian coronavirus crisis is in Moscow, which as of April 30 had about 53,700, or roughly half, of Russia’s 106,500 cases. But the disease is rapidly making its way out to the regions where the populations may be, demographically-speaking, more vulnerable if they get infected. As in other countries, COVID-19 started in the largest cities, and then began to seep out to rural areas where the populations are older, as are the medical facilities. In addition, as Judy Twigg has noted, the chronic diseases that disproportionately afflict many Russians (and especially men)—diabetes, heart disease and chronic obstructive pulmonary disease— are those that are associated with coronavirus victims who require more intensive care. Some 40 percent of Russians suffer from multiple chronic diseases.
In addition to disparities in regions’ demographic characteristics and the prevalence of underlying conditions that can make the virus more deadly, Russia faces two more major problems in its fight with the coronavirus. First, seven years of “optimizing” the health care system have significantly reduced not only inefficiencies, but also the capacity of the system to deal with the current crisis. The number of Russian epidemiologists has fallen from 33,300 in 1990 to 13,300 in 2018 , while the number of beds for infectious diseases fell from 140,000 to 59,000 . All that being said, Russia still has an impressive number of doctors and hospital beds—479 doctors and 797 beds per 100,000 people (Germany has 430 and 800, respectively; the United States has 280 and 277 . Tatiana Golikova, the vice premier for health, has said that 94,000 total beds are ready for coronavirus patients.) The neoliberal call to reduce the size of the public sector was not fully implemented in Russia, despite repeated calls from Western advisors.
Second, these resources are not evenly distributed across the country. The number of epidemiologists per 100,000 residents varies from 26 in Altai and the Chukotskiy AO to one in Chechnya . Available ventilators per 1,000 residents varies greatly across regions, but reported statistics should be read as an indication of regional variation, not as reliable data. This is clear from the anecdotal story of a medic in the hospital in Kalach-on-Don. She complained they had only 2.5 ventilators—2 already being used by patients and one with a broken compressor. She was then interrogated by police while the hospital rounded up their hand-pumped ventilators and some other older, nonworking units to bring up their total number of ventilators to 13 .
Moscow has the money to build emergency field hospitals, like it just did in Voronovskoe. However, Russian regional governments, which bear the primary responsibility for funding health care, will not be able to afford personal protective equipment for medical staff, let alone new facilities. Only 41 percent of Russian medical facilities have access to the internet and 10 percent of Russian medical facilities need significant upgrades: half of these have no hot water, and a third lack indoor toilets.
The Political Fallout
Russian President Vladimir Putin has, for the most part, been sitting out the pandemic and working remotely. His public speeches have been increasingly stern, but governors and mayors have been left to deal with the crisis as best they can—ideally without outshining the president. In Moscow, Mayor Sergey Sobyanin has emerged as the man in charge, which may come back to haunt him. Other regional leaders have followed his lead, for example, announcing that they too would introduce a digital pass system for residents who want to travel from their apartments.
The coronavirus may have weakened the Kremlin’s domestic power, but its strength may always have been somewhat illusory. Yes, there is a vertical of power and the federal government has consolidated control over the past twenty years. But the Ministry of Health is like the American Centers for Disease Control—it issues guidance, and then it’s up to the regions to implement. The Italian and American epidemics revealed the extent to which regional leadership can make a difference, for better or worse. Unfortunately, it’s now Russia’s turn to experience this revelation, which was anticipated by Russian author and doctor Mikhail Bulgakov in The White Guard (1926), “For twenty years people have been engaged activities like, for example, reading Roman law, and on the twenty-first, it suddenly turns out that Roman law has nothing to do with anything…”
This piece was originally published on April 30, 2020, by Russia Matters: https://www.russiamatters.org/analysis/russias-health-care-system-demographics-present-unique-advantages-disadvantages-fighting

Alexandra Vacroux
Executive Director, Davis Center
Subscribe to the Davis Center Newsletter
Be the first to know about events, programs, and news.
- Search Menu
- Browse content in Arts and Humanities
- Browse content in History
- Colonialism and Imperialism
- History by Period
- Intellectual History
- Military History
- Political History
- Regional and National History
- Social and Cultural History
- Browse content in Literature
- Literary Theory and Cultural Studies
- Browse content in Media Studies
- Browse content in Philosophy
- Philosophy of Religion
- Browse content in Religion
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Religious Studies
- Browse content in Society and Culture
- Cultural Studies
- Technology and Society
- Browse content in Law
- Comparative Law
- Constitutional and Administrative Law
- Criminal Law
- Employment and Labour Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Public International Law
- Jurisprudence and Philosophy of Law
- Legal System and Practice
- Medical and Healthcare Law
- Browse content in Science and Mathematics
- History of Science and Technology
- Browse content in Psychology
- Developmental Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Medical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Criminology and Criminal Justice
- Browse content in Economics
- Economic History
- Browse content in Education
- Early Childhood and Elementary Education
- Educational Strategies and Policy
- Browse content in Politics
- Asian Politics
- Comparative Politics
- Conflict Politics
- Environmental Politics
- European Union
- International Relations
- Middle Eastern Politics
- Political Theory
- Political Sociology
- Public Policy
- Security Studies
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- Latin American Studies
- Browse content in Social Work
- Child and Adolescent Social Work
- Couple and Family Social Work
- Mental and Behavioural Health
- Social Work and Crime and Justice
- Browse content in Sociology
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Urban and Rural Studies
- Reviews and Awards
- Journals on Oxford Academic
- Books on Oxford Academic
- < Previous chapter
- Next chapter >
Nine Health and Health Care in Russia Today and Tomorrow
- Published: May 2011
- Cite Icon Cite
- Permissions Icon Permissions
This chapter displays the complex linkages between the depressed state of health and demographics in Russia and the integrity and security of the Russian social organism. It presents some population and health statistics for the Russian Federation (RF), examines some factors that influenced the deterioration in the health of the Russian population, discusses problems in the RF health care system that affect the quality and availability of medical and preventive care, and evaluates the challenges that the system will face till 2020 and the expectations of the parties concerned. Finally, the chapter presents some recommendations for the development of a health care strategy to improve the health status of the Russian population according to the guidelines set by the RF government for the year 2020.
Signed in as
Institutional accounts.
- GoogleCrawler [DO NOT DELETE]
- Google Scholar Indexing
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
Institutional access
- Sign in with a library card Sign in with username/password Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Sign in through your institution
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Sign in with a library card
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice

This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Healthcare in the Russian Federation
Introduction, impact on vulnerable population, women’s health and maternal child health, disease management of communicable and non-communicable diseases, the theory and practice of health promotion, behavioral and lifestyle factors that affect health and illness, comparison with the us.
The Russian Federation is the largest country in the world, yet it is still considered a developing nation. Russia managed to separate from the Soviet Union in the 1990s in hopes of a better future for the country and its citizens. In 1993, under the Russian Constitution, the right to free health care was guaranteed to every Russian citizen. Thus far, the healthcare system in Russia is subpar and even described with such words as “grim” and “bleak.” Health care facilities are lacking, resources are limited, and public health is not a priority to Russian Citizens. The mortality rate for young Russian men are astronomical, and alcoholism, tobacco usage, and HIV/AIDS are preventing Russians from living health and disease-free lives.
A current shift towards health promotion and prevention of not transmissible diseases is on the rise in Russia. The problems have been identified by health care officials, and now it is up to the government and health and wellness stakeholders to provide the necessary resources to Russian Citizens. It should be noted that there are chronic health concerns within the Russian Federation and an assessment of public health and its promotion within Russia (“Russian City Offers Health Pursuits for All Ages,” 2013). In addition, one needs to assess fundamental healthcare principles and how self-care is perceived in Russia (Tolpygina et al., 2018). It is also critical to understand how Russia’s healthcare system is impacted by investments and the local economy (Tokun, 2016). Therefore, several key factors lead to major Russian healthcare issues, such as chronic diseases, poor lifestyle habits, and lack of health promotion.
The healthcare system of the Russian Federation is not developed enough to be able to provide fully covered care for its vulnerable population. It is stated that there is an issue of representation of children, which results in higher instances of complications (Bovina et al., 2018). Another study suggests that there is a wide range of problems in health provision for children, where socioeconomic factors play an essential role (Kononova, 2016). The primary causes of childhood disability are mental disorders, diseases of the nervous system, congenital malformations, and somatic diseases. The formation of disability as a result of a severe course of somatic pathology occurs mainly by the age of 10-12, and as a result of mental disorders – by the age of 14-15 (Kononova, 2016). The outcome of chronic disease into disability is most often associated with an insufficient level of preventive work with a healthy child, health-improving, and with children suffering from a chronic pathology– rehabilitation work. Not enough attention is paid to the rehabilitation treatment of children with an established disability, but with high rehabilitation potential.
The aging process of the population in Russia requires the state to pay more attention to its social protection. The formation of social and medical stability of the elderly, and its development, and management has become an objective necessity of the nation. The system of social and medical work with the elderly has already been established in the country. However, despite certain successes, it can be concluded that the previous forms and methods of social and medical work with elderly citizens are not always effective. It is necessary to solve social and medical problems by further improving the social and medical practice with the elderly, and this requires an analysis of the current state of the ego type of activity. The organization of social and medical work at the regional level is of great importance.
Low income is one of the main factors, and the rise in food prices leads to a deterioration in the diet of the elderly. The pensioner is experiencing difficulties in purchasing essential goods, and spending on social and cultural needs is decreasing. All of this hurts the health of older people. Loneliness for many older adults is an important problem, characterized by a low level of social contact, estrangement, and emotional detachment. The main reasons for loneliness in mature and old age are long-term illness, inability to adapt to constantly changing external conditions, death of loved ones, spouse, and relatives.
Women belong to the part of the population that most sensitively reacts to all changes in the social, economic, and social life of the country. They especially respond to changes related to the state of their health, reproductive behavior, and the quality of their children’s health. The state of health of a woman is a marker that shows the state of health of a society at a certain moment and determines it for the distant future. Of women and maternal health, Russian healthcare possesses certain risk factors. It is stated that preterm birth is one of the central issues in this regard, where induced and spontaneous abortions are identified as the main catalyzers (Usynina et al., 2016). However, the current measures of the Russian Federation’s healthcare system involve a three-level system, which includes intensive care during pregnancy, childbirth, and the postpartum period (Shuvalova et al., 2015). The overall morbidity picture becomes especially alarming when analyzing the health of the most reproductively active part of the female population, such as pregnant women. Their health status directly determines the health status of their children.
The history of modern women entering pregnancy is already burdened by various genital diseases. Over the past decade, the proportion of such women among pregnant women has increased significantly. The most common, severe illnesses, and complications of pregnancy are anemia, kidney disease, circulatory system, late gestation (Shuvalova et al., 2015). The issues of prenatal health deserve serious attention because the intrauterine or prenatal period takes up an insignificant period of time in the total life span of a person. However, it is during this period that human health and ill-health are formed, and not only at the organismic level, but also the health of subsequent generations is determined.
The Russian healthcare system is not lagging behind regarding communicable diseases. However, there is a major issue in terms of non-communicable ones, where chronic issues are the most prominent. It is stated that, currently, almost 40% of all Russian citizens live with multi-morbidity due to chronic conditions (Kaneva et al., 2018). Insufficient resource provision of Russian healthcare is exacerbated by ineffective management. It manifests itself in the fact that the industry does not highlight priorities. There is a contradictory regulatory framework, the regulatory requirements themselves are often not provided with the necessary resources. Moreover, statistical data are conflicting or closed, an objective, systematic analysis of activities is not carried out, as a result, the right decisions are not made. Thus, the requirements of mandatory procedures are not coordinated with the methodological documents.
The costs of chronic illness can be reduced or moved later in life through prevention. Quantifying the risk factors that determine the development of chronic diseases is the key to understanding how to build prevention of pathology. The structure of prevention should include three main components, such as primary, secondary, and tertiary prevention. Primary prevention is carried out before the development of the disease, and secondary prevention is aimed at those who have the first symptoms or conditions that are former to the development of the disease. Tertiary prevention is aimed at those who already have the disease, where the goal is to reduce disability, the frequency of exacerbations, and complications. The means of preventing most chronic diseases range from interventions for individuals or families, initiatives for health workers, and organizational change.
The requirements of standards of medical care and procedures for its provision are often not provided with resources, and, accordingly, are not feasible. At the same time, numerous inspections of control and supervisory bodies are carried out for compliance with the requirements of procedures and standards, but the effectiveness of these inspections is questionable. Moreover, the restrictions themselves and the criteria for the checks are multiplying. Therefore, it is critical to follow the priority directions for actions to protect the health of the population of the Russian Federation by slowing the occurrence rate of chronic diseases. In the coming years, these should be the protection of the health of Russian men of working age, Russian children, and adolescents, as well as the elimination of differences in the health status of urban and rural residents.
The Russian healthcare system lacks strong structural integration for health promotion and in both theory and practice. The urgency of solving this problem continues to remain high due to the fact that, despite some positive trends, health indicators, and the state of health care, in general, are at an unsatisfactory level. The hard conditions for the social and economic development of the country displayed themselves, especially, in extremely high rates of morbidity and mortality. There are also low birth rates, the state of health of mothers and children, the quality of nutrition, especially of the unprotected segments of the population, and deepening social differentiation.
The special significance of health promotion programs lies in the fact that socially dependent and professionally determined health defects of the population have been progressing in the last decade. After diseases of the circulatory system, accidents, poisoning, and injuries became the second cause of death in the structure. For many years, the general tendencies in mortality of the population of Russia have been determined by the situation with the high mortality of people of working age. Every year, the overall proportion of neurotic and mental disorders in the structure of morbidity increases. One of the effective ways out of this situation is to increase the health potential of healthy people. Secondly, there is the return of health to patients, patients outside the stage of exacerbation, persons in a state of pre-illness, due to the system of methods of restorative medicine.
The key problem for all areas of health protection is the formation of a culture of health, increasing the prestige of health, self-awareness of the value of health as a factor of resilience, active longevity. The highest priority is to increase the level of psychophysical health, maintain optimal performance, quality of life of the population, and the individual’s achievement of a genetically determined life expectancy. This will ultimately provide the need for a healthier lifestyle and the cultural, social, and economic motive for maintaining and promoting health. It is important to take into account the current situation associated with the deterioration of the basic parameters of the population’s health, the low level of influence on it by the activities of medical institutions. The main and important priorities should be the availability of measures for the rapid assessment of the health status and health improvement of the population, regardless of social status. In addition, it is important to focus on a quantitative evaluation of the body’s reserve capabilities and their correction for the person to realize the health potential.
In terms of behavioral and lifestyle factors, there is tobacco smoking and alcohol drinking affect health. It is stated that the overall drinking of homemade alcoholic beverages in Russia significantly contributes to morbidity and risk (Radaev, 2016). In order for the Russian healthcare system to properly handle the issue, it requires the implementation of two key strategic directions. First of all, it is important to reduce the consumption of alcohol and tobacco among the population. The application of this direction should become the area of responsibility of the heads of regions and municipalities. To do this, it is necessary to urgently start developing and implementing national, regional, and municipal comprehensive interdepartmental programs to reduce the prevalence of alcohol and tobacco consumption, especially among young people.
Secondly, it is critically important to enhance free medical care and its availability. This is the area of responsibility of the Minister of Health of the Russian Federation and the regional health authorities. In this case, priorities are also important, because it may not be possible to develop everything at the same time due to the lack of resources. Employers as well ought to participate in the implementation of this approach.
There are a number of factors that make Russia vastly different from the US, such as politics, culture, wealth, history, and environmental factors. It is stated that corruption is a major issue in Russia, and it has a significant effect on the local healthcare system (Schulze et al., 2016). The lack of political representation of the public and the absence of health-promoting culture alongside the low median income of Russian households results in the fact that providing free state-run healthcare is paramount. Therefore, there is no market force to improve the healthcare system because it is highly regulated.
In conclusion, the healthcare system of the Russian Federation is not as developed as it should be due to low funding and poor infrastructure. One of the most vulnerable members of society suffers from preventable issues, whereas the majority of the population suffers from chronic diseases. Although there are some attempts to promote health, the current system is weak due to the system’s inherent inefficiency. In contrast with the US, Russian healthcare does not benefit from market forces and lacks sufficient funding.
Bovina, I. B., Dvoryanchikov, N. V., Dany, L., Aim, M. A., Milekhin, A. V., Gayamova, S. Y., & Yakushenko, A. V. (2018). Health representations of children and adolescents. Experimental Psychology, 18 (1), 61-74.
Kaneva, M., Gerry, C. J., & Baidin, V. (2018). The effect of chronic conditions and multi-morbidity on self-assessed health in Russia. Scandinavian Journal of Public Health , 46 (8), 886-896.
Kononova, A. E. (2016). Socioeconomic factors of children health in Russia. Sociological Studies, 1 (4), 94-102.
Radaev, V. (2016). Divergent drinking patterns and factors affecting homemade alcohol consumption. International Journal of Drug Policy, 34 (7), 88-95.
Russian city offers health pursuits for all ages. (2013). Bulletin of the World Health Organization , 91 (10), 722–723.
Schulze, G. G., Sjahrir, B. S., & Zakharov, N. (2016). Corruption in Russia. The Journal of Law and Economics, 59 (1), 135-171.
Shuvalova, M. P., Yarotskaya, E. L., Pismenskaya, T. V., Dolgushina, N. V., Baibarina, E. N., & Sukhikh, G. T. (2015). Maternity care in Russia: Issues, achievements, and potential. Journal of Obstetrics and Gynaecology Canada, 37 (10), 865-871.
Tokun, L. (2016). Investments as a factor of stability of the Russian healthcare system. MIR [World] (Modernization Innovation Research) , 7 (2(26)), 132-138.
Tolpygina, S. N., Martsevich, S. Y., Kontsevaya, A. V., & Drapkina, O. M. (2018). Responsible self-care – the fundamental principles and place in the modern Russian healthcare system. Rational Pharmacotherapy in Cardiology , 14 (1), 101-110.
Usynina, A. A., Postoev, V. A., Grjibovski, A. M., Krettek, A., Nieboer, E., Odland, J. O., & Anda, E. E. (2016). Maternal risk factors for preterm birth in Murmansk county, Russia: A registry‐based study. Paediatric and Perinatal Epidemiology, 30 (5), 462-472.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2022, April 17). Healthcare in the Russian Federation. https://studycorgi.com/healthcare-in-the-russian-federation/
"Healthcare in the Russian Federation." StudyCorgi , 17 Apr. 2022, studycorgi.com/healthcare-in-the-russian-federation/.
StudyCorgi . (2022) 'Healthcare in the Russian Federation'. 17 April.
1. StudyCorgi . "Healthcare in the Russian Federation." April 17, 2022. https://studycorgi.com/healthcare-in-the-russian-federation/.
Bibliography
StudyCorgi . "Healthcare in the Russian Federation." April 17, 2022. https://studycorgi.com/healthcare-in-the-russian-federation/.
StudyCorgi . 2022. "Healthcare in the Russian Federation." April 17, 2022. https://studycorgi.com/healthcare-in-the-russian-federation/.
This paper, “Healthcare in the Russian Federation”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: July 30, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.

- Publishing Policies
- For Organizers/Editors
- For Authors
- For Peer Reviewers
Digital Healthcare In The Russian Federation: Systems And Technologies
Successful modernization of the Russian Federations healthcare system depends on the efficiency of organization processes transformation in healthcare and medicine on the basis of digital platforms. It will allow to provide constant control over expenses for achievement of careful rational expenditure of means, and also the new medical, organizational technologies promoting formation of economy (management of patients streams, telemedicine, providing information support of medical diagnostic processes and medical decisions, geoinformation systems application, systems of processing of medical images). The creation and active use of digital platforms will contribute to the introduction of a model of process management in the healthcare sector, which focuses on the performance of functions by departments and, as a consequence, meeting the needs of citizens. Digital healthcare platforms combine such information resources as laboratory results, electronic patient histories, standards of diagnosis and treatment of patients financial and economic information, databases of medicines, material and labor resources, expert systems, etc. Electronic services allow to use all modern possibilities of collection, storage and processing of information that promotes leveling of the errors connected with time delays of paper document circulation, increase of efficiency of use of working time of doctors, creation of comfortable conditions for interaction with patients. Keywords: Digital healthcare telemedicine artificial intelligence
Introduction
The basic task of modern health care is to ensure a high level of treatment and prevention of the population, which can be achieved through digitalization. Healthcare management as an adaptive digital platform involves a systematic consideration of patient-doctor interactions on the basis of modern technologies that provide not only effective treatment, but also prevention of diseases. This study examines the systems and technologies that are modernizing the health care system and making up the trend of digital medicine.
Problem Statement
At present, digital transformation is the leading factor of socio-economic development. Digital transformation is one of the main factors in the development of health care. In public health, digital economy systems and technologies are a major trend and a leading component. For Russian healthcare, digital systems and technologies are the main system-forming factor and are increasingly used. When reforming the Russian health care, the main emphasis is on the use of digital transformations, which will enable the Russian health care to take a leading position in the structure of the country's economic growth. The main burden of Russian health care is that it carries high costs for maintaining the health of people older than 65 years, which are 4-5 times higher than for maintaining the health of people younger than 65 years. The growth of chronic diseases in Russia creates new long-term needs for medical services on the basis of constant interaction with patients, including through the Internet. All this requires the development of new digital platforms and technologies related to the provision of health services, so it is urgent to identify and analyze the main digital technologies and systems that allow for the digital transformation of health care.
Research Questions
The Russian medical cluster should ensure the availability of qualified medical services, and the basis for this is digitalization, which ensures close interaction between the doctor and the patient. Important issues considered in the study are new digital medical technologies: telemedicine technologies, "cloud" technologies used to store large information arrays in the big data format (for example, computed tomography or magnetic resonance imaging).
Innovative is the consideration of the use of Internet of things technology in the development of coherent, secure, flexible real-time healthcare systems incorporating Internet of things technology ( Chen, Lughofer, & Polikar, 2018 ). Intelligent healthcare systems that analyze patient data generated from the Internet of things.
We consider a cognitive healthcare system that uses cloud technologies of the Internet of things and allows on the basis of intelligent sensors to monitor the status of patients in real time and provides accurate, timely and high-quality medical services at low cost ( Syed Umar, Shamim, & Ghulam, 2019 ). The issues of using biomedical signals for intelligent mobile healthcare using big data analysis ( Jeon, Ahmad, Cuomo, & Wu, 2019 ).
The issues of automatic monitoring of voice pathology using models for smart medicine are described ( Musaed & Ghulam, 2019 ). The inclusion of health services for older people in smart homes through the Internet of things, contributing to better care for them ( Choi, Choi, & Shon, 2019 ), is reflected.
An evolving 5G network is described that will support intelligent healthcare applications that meet most requirements such as ultra-low latency, high throughput, ultra-high reliability, high density, and high energy efficiency ( Abdul, Mohammad, & Kok-Lim Alvin, 2019 ).
In relation to Russia, the information medical space is considered, including a Single state information system in the field of health care, mobile devices and gadgets that provide monitoring of vital functions, new mobile applications for Android, Windows Modile, etc., designed to expand the scope of user application of personal wearable gadgets.
Purpose of the Study
Based on the disclosure of the questions, the aim of the study was formulated: to form technological and platform contours of digital healthcare in Russia on the basis of the main digital platforms and technologies.
The main platform of the digital healthcare circuit in Russia is the unified state information system in the field of healthcare, which provides personalized medical care of all kinds. The main subsystems of the platform: electronic registry, integrated electronic medical record, register of normative and reference information. Electronic registry provides monitoring and management of interaction between patients and medical staff. Integrated electronic medical record allows you to collect, organize and process patient data. The register of normative and reference information provides digital formation and updating of all information in the field of health care. Updating and information interaction of classifiers, reference books, normative information in the field of health care.
The main technologies of the digital circuit are telemedicine and medical artificial intelligence systems. Telemedicine allows on the basis of mobile applications and special services to interact doctor and patient. Thus, the patient will be able to receive qualified care online at any time, while being at home. Artificial intelligence technologies allow to systematize a large amount of medical data on the basis of neural networks
The Samara-Togliatti agglomeration may become a priority platform for the implementation of the digital healthcare circuit. Organizational arrangements for the creation of a digital contour health of Samara-Togliatti agglomeration should include: the establishment of regional interagency project of the center for the selection, pilot testing and implementation of innovative products, development of complex of measures on creation and introduction in practice of health and medical education innovative products on the subject of IT-medicine, using technology, virtual and augmented reality, neurotechnology, artificial intelligence formation of "end-to-end " technologies in the field of digital health care within the framework of the Scientific and technological initiative of Russia.
Research Methods
In the study, the calculation of the integral estimates of the level of digitalization of healthcare in the Russian regions was carried out using an iterative method of multivariate belonging to the group of methods of multidimensional comparative analysis. The justification of its use for the construction of rating estimates and multivariate comparative analysis of regional levels of socio-economic development is given in the works of Russian scientists ( Tikhomirova & Chapligin, 2003 ). The problem of obtaining weight coefficients, as well as the application of the iterative method are described in detail in the work of Tikhomirova ( 2009 ).
Multivariate comparative analysis reflects the deterministic state of the region in terms of digitalization of health care and does not take into account the stochastic nature of the processes under consideration. In our opinion, the solution of the two-fold problem of multidimensional comparative analysis taking into account the probabilistic ( Parmeter & Kumbhakar, 2014 ) component of modern mass digitalization processes is possible within the framework of stochastic frontier analysis, the essence of which is the construction of multidimensional nonlinear stochastic models to obtain on their basis aggregated quantitative estimates of the States of the subjects and their subsequent comparison.
Thus, the methods of this class allow to develop nonlinear probabilistic models, to obtain on their basis multidimensional deterministic estimates and to carry out the distribution of subjects to assess their functioning taking into account the deterministic and stochastic component.
Systems and technologies of digital health care are investigated. It is shown that in Russia a single state information system in the field of health care is used as the main platform for digital health care. Based on the analysis of the regional dimension of healthcare digitalization, the following conclusions are made. The region’s healthcare information space is platform-independent, the region’s cloud-based digital healthcare platform is a technology group that will unite all regional services. Information and technological conditions for transforming regional healthcare into digital are based on the results of monitoring health resources and include big data technologies. The transformation of the quality control system for doctors is carried out through the introduction of information systems for decision support based on the use of intelligent processing and analysis of "big" data. Cloud technologies, intelligent technologies based on big data, telemedicine are considered as the main technologies of smart medicine.
Thus, this study identifies global trends in the creation and development of digital healthcare. The issues of using telemedicine technologies, “cloud” technologies for storing large information arrays about patients, developing flexible healthcare systems based on the Internet of things, cognitive healthcare, using smart sensors to track the patient’s condition, and mobile systems for monitoring the patient’s condition are investigated. Proposals for the development of digital health care in the Samara. It is shown that the transformation of regional healthcare into digital is based on intelligent and cloud technologies. Togliatti agglomeration are given. Special attention is paid to the unified state information system in the field of health care in Russia.
- Abdul, A., Mohammad, T., & Kok-Lim Alvin, Y. (2019). 5G-based smart healthcare network: Architecture, taxonomy, challenges and future research directions. IEEE Access, 7, 100747-100762.
- Chen, M. -Y., Lughofer, E. D., & Polikar, R. (2018). Big data and situation-aware technology for smarter healthcare. Journal of Medical and Biological Engineering, 38(6), 845-846. https://doi.org/10.1007/s40846-018-0452-4
- Choi, D., Choi, H., & Shon, D. (2019). Future changes to smart home based on AAL healthcare service. Journal of Asian Architecture and Building Engineering, 18(3), 190-199. https://doi.org/10.1080/13467581.2019.1617718
- Jeon, G., Ahmad, A., Cuomo, S., & Wu, W. (2019). Special issue on bio-medical signal processing for smarter mobile healthcare using big data analytics. Journal of Ambient Intelligence and Humanized Computing, 10(10), 3739-3745. https://doi.org/10.1007/s12652-019-01425-9
- Musaed, A., & Ghulam, M. (2019). Automatic voice pathology monitoring using parallel deep models for smart healthcare. IEEE Access, 7, 46474-46479.
- Parmeter, C. F., & Kumbhakar, S. C. (2014). Efficiency analysis: A primer on recent advances. Foundations and Trends in Econometrics, 7(3-4), 191-385. https://doi.org/10.1561/0800000023
- Syed Umar, A., Shamim, H., & Ghulam, M. (2019). Cognitive smart health care for pathology detection and monitoring. IEEE Access, 7, 10745-10753.
- Tikhomirova, E. I. (2009). Statistical assessment of competitiveness of regions of the Russian Federation: Methodological and information support. Samara: Samara State University of Economics. [in Rus.].
- Tikhomirova, E. I., & Chapligin, S. I. (2003). Multidimensional comparative analysis of the competitiveness of the Samara region in the system of regions of the Volgo-Ural zone. Samara: Samara State University of Economics. [in Rus.].
Copyright information

About this article
Publication date.
09 March 2020
Article Doi
https://doi.org/10.15405/epsbs.2020.03.207
978-1-80296-078-5
European Publisher
Print ISBN (optional)
Edition number.
1st Edition
Business, business ethics, social responsibility, innovation, ethical issues, scientific developments, technological developments
Cite this article as:
Kazarin, S. V., Svechnikova, N. Y., & Pogorelova*, E. V. (2020). Digital Healthcare In The Russian Federation: Systems And Technologies. In S. I. Ashmarina, & V. V. Mantulenko (Eds.), Global Challenges and Prospects of the Modern Economic Development, vol 79. European Proceedings of Social and Behavioural Sciences (pp. 1445-1449). European Publisher. https://doi.org/10.15405/epsbs.2020.03.207
We care about your privacy
We use cookies or similar technologies to access personal data, including page visits and your IP address. We use this information about you, your devices and your online interactions with us to provide, analyse and improve our services. This may include personalising content or advertising for you. You can find out more in our privacy policy and cookie policy and manage the choices available to you at any time by going to ‘Privacy settings’ at the bottom of any page.
Manage My Preferences
You have control over your personal data. For more detailed information about your personal data, please see our Privacy Policy and Cookie Policy .
These cookies are essential in order to enable you to move around the site and use its features, such as accessing secure areas of the site. Without these cookies, services you have asked for cannot be provided.
Third-party advertising and social media cookies are used to (1) deliver advertisements more relevant to you and your interests; (2) limit the number of times you see an advertisement; (3) help measure the effectiveness of the advertising campaign; and (4) understand people’s behavior after they view an advertisement. They remember that you have visited a site and quite often they will be linked to site functionality provided by the other organization. This may impact the content and messages you see on other websites you visit.
- Health, Pharma & Medtech ›
- Health System
Healthcare in Russia - statistics & facts
Russian health system, what are the most common diseases in russia, key insights.
Detailed statistics
Structure of expenditure on healthcare in Russia 2019-2024, by source
Number of hospitals in Russia 2010-2022
Number of medical visits in Russia 2018-2022
Editor’s Picks Current statistics on this topic
Current statistics on this topic.
Health Economics
Healthcare Professionals
Density of doctors in Russia 2010-2021
Related topics
Health and pharmaceuticals in russia.
- Coronavirus (COVID-19) in Russia
- Pharmaceutical industry in Russia
- Pharmaceutical e-commerce in Russia
Healthcare in Central and Eastern Europe
- Healthcare in Poland
- Healthcare in Hungary
- Health care in Romania
- Health care in Czechia
Trends in healthcare
- Global health
- Medical technology
- Biotechnology in Europe
- Health and wellness food trends in Europe
Recommended statistics
- Premium Statistic Expenditure on healthcare in Russia 2014-2029
- Premium Statistic Spending per capita on healthcare expenditure in Russia 2014-2029
- Premium Statistic GDP share of health expenditure in Russia 2014-2029
- Premium Statistic Structure of expenditure on healthcare in Russia 2019-2024, by source
- Premium Statistic Number of medical laboratory services users in Russia 2017-2022
- Basic Statistic Public trust in health system in Russia 2022
- Premium Statistic Medical services revenue in Russia 2022, by city
- Premium Statistic Highest-earning medical companies in Russia 2022
- Premium Statistic MD Medical Group (Mother & Child) revenue in Russia 2009-2023
Expenditure on healthcare in Russia 2014-2029
Expenditure on healthcare in Russia from 2014 to 2029 (in million U.S. dollars)
Spending per capita on healthcare expenditure in Russia 2014-2029
Spending per capita on healthcare expenditure in Russia from 2014 to 2029 (in U.S. dollars)
GDP share of health expenditure in Russia 2014-2029
GDP share of health expenditure in Russia from 2014 to 2029
Government expenditure on healthcare in Russia from 2019 to 2024, by source (in billion Russian rubles)
Number of medical laboratory services users in Russia 2017-2022
Number of users of laboratory diagnostics services in Russia from 2017 to 2022 (in millions)
Public trust in health system in Russia 2022
To what extent do you trust the Russian health system?
Medical services revenue in Russia 2022, by city
Cities with the highest revenue from medical services in Russia in 2022 (in billion Russian rubles)
Highest-earning medical companies in Russia 2022
Leading medical companies in Russia in 2022, by revenue (in billion Russian rubles)
MD Medical Group (Mother & Child) revenue in Russia 2009-2023
Revenue of MD Medical Group (Mother & Child) in Russia from 2009 to 2023 (in billion Russian rubles)
Physicians & hospitals
- Premium Statistic Number of physicians in Russia 1990-2021
- Premium Statistic Density of doctors in Russia 2010-2021
- Premium Statistic Density of doctors in Russia 2021, by field
- Basic Statistic Nursing and midwifery personnel density in Russia 2010-2021
- Premium Statistic Salary of medical professionals in public sector in Russia 2022, by level & region
- Basic Statistic Number of hospitals in Russia 2010-2022
- Basic Statistic Hospital bed density in Russia 2008-2022
- Basic Statistic Number of hospital beds in Russia 2022, by ward
- Premium Statistic Number of medical visits in Russia 2018-2022
Number of physicians in Russia 1990-2021
Number of doctors in Russia from 1990 to 2021 (in 1,000s)
Number of doctors per 10,000 population in Russia from 2010 to 2021
Density of doctors in Russia 2021, by field
Number of doctors per 10,000 population in Russia in 2021, by field
Nursing and midwifery personnel density in Russia 2010-2021
Number of mid-level medical personnel per 10,000 population in Russia from 2010 to 2021
Salary of medical professionals in public sector in Russia 2022, by level & region
Average monthly salary of health care professionals in the public sector in Moscow, Saint Petersburg, and across Russia in 2022, by occupation level (in Russian rubles)
Number of hospital organizations in Russia from 2010 to 2022
Hospital bed density in Russia 2008-2022
Number of hospital beds per 10,000 population in Russia from 2008 to 2022
Number of hospital beds in Russia 2022, by ward
Number of hospital beds in Russia in 2022, by department (in 1,000s)
Number of medical visits in Russia from 2018 to 2022 (in billion visits)
State of health
- Premium Statistic Death rates by main cause in Russia 2022
- Basic Statistic Healthy lifestyle follower share in Russia 2019-2022
- Premium Statistic Cigarettes smoked per day in Russia 2022
- Premium Statistic Morbidity with alcoholism and drug addiction in Russia 2003-2021
- Basic Statistic Abortion count in Russia 2000-2022
- Basic Statistic Number of obesity patients in Russia 2010-2022
- Basic Statistic People with a disability in Russia 2018-2023, by group
Death rates by main cause in Russia 2022
Number of deaths from selected major causes in Russia in 2022 (per 100,000 population)
Healthy lifestyle follower share in Russia 2019-2022
Share of population following a healthy lifestyle in Russia from 2019 to 2022
Cigarettes smoked per day in Russia 2022
Cigarettes smoked per day in Russia in 2022
Morbidity with alcoholism and drug addiction in Russia 2003-2021
Number of people registered for outpatient treatment for alcoholism and alcoholic psychosis and drug addiction per 100,000 population in Russia from 2003 to 2021
Abortion count in Russia 2000-2022
Number of abortions in Russia from 2000 to 2022 (in 1,000s)
Number of obesity patients in Russia 2010-2022
Number of obesity patients in Russia from 2010 to 2022 (in 1,000s)
People with a disability in Russia 2018-2023, by group
Number of people with a disability in Russia from 2018 to 2023, by group (in 1,000s)
- Premium Statistic Morbidity rate in Russia 2021, by disease type
- Premium Statistic Socially significant diseases morbidity rate in Russia 2021, by type
- Basic Statistic Morbidity rate of children aged 0-14 years in Russia 2022, by disease
- Basic Statistic HIV morbidity rate in Russia 2010-2021
- Basic Statistic Tuberculosis morbidity rate in Russia 2010-2021
- Basic Statistic Hepatitis B morbidity rate in Russia 2010-2021
- Basic Statistic Number of new cancer diagnoses in Russia 2021, by type
- Basic Statistic Number of cancer deaths in Russia 2021, by major type
- Basic Statistic Obesity diagnoses growth in Russia 2019-2021
Morbidity rate in Russia 2021, by disease type
Number of patients diagnosed with disease for the first time per 1,000 population in Russia in 2021, by type
Socially significant diseases morbidity rate in Russia 2021, by type
Number of patients diagnosed with socially significant diseases per 100,000 population in Russia in 2021, by type
Morbidity rate of children aged 0-14 years in Russia 2022, by disease
Number of children aged under 14 years diagnosed with diseases for the first time in Russia in 2022, by type (per 100,000 children aged from 0 to 14 years)
HIV morbidity rate in Russia 2010-2021
Number of first-diagnosed HIV patients per 100,000 population in Russia from 2010 to 2021
Tuberculosis morbidity rate in Russia 2010-2021
Number of first-diagnosed tuberculosis cases per 100,000 population in Russia from 2010 to 2021
Hepatitis B morbidity rate in Russia 2010-2021
Number of first-diagnosed Hepatitis B cases per 100,000 population in Russia from 2010 to 2021
Number of new cancer diagnoses in Russia 2021, by type
Number of first-diagnosed cancer cases in Russia in 2021, by major type (in 1,000s)
Number of cancer deaths in Russia 2021, by major type
Number of deaths from malignant neoplasms in Russia in 2021, by major type
Obesity diagnoses growth in Russia 2019-2021
Growth in number of first-diagnosed obesity cases in Russia from 2019 to 2021
- Basic Statistic COVID-19 situation in Russia 2023
- Basic Statistic Cumulative COVID-19 cases, recoveries, and deaths in Russia 2020-2023
- Basic Statistic Number of COVID-19 testing laboratories in Russia 2023, by type
COVID-19 situation in Russia 2023
Key figures on the coronavirus (COVID-19) pandemic in Russia as of July 31, 2023
Cumulative COVID-19 cases, recoveries, and deaths in Russia 2020-2023
Cumulative number of coronavirus (COVID-19) cases, recoveries, and deaths in Russia from January 31, 2020 to October 22, 2023, by date of report
Number of COVID-19 testing laboratories in Russia 2023, by type
Number of laboratories testing for the coronavirus (COVID-19) in Russia as of February 2, 2023, by type
- Premium Statistic Medical devices market revenue in Russia 2014-2022
- Premium Statistic Russia: revenue of medical devices 2018-2028, by segment
- Premium Statistic Highest-earning MedTech companies in Russia 2022-Q3 2023
- Premium Statistic Trust in AI in healthcare in Russia 2023, by age group
Medical devices market revenue in Russia 2014-2022
Revenue of the medical devices market in Russia from 2014 to 2022 (in billion Russian rubles)
Russia: revenue of medical devices 2018-2028, by segment
Revenue of medical devices in Russia from 2018 to 2028, by segment (in million U.S. dollars)
Highest-earning MedTech companies in Russia 2022-Q3 2023
Leading MedTech companies in Russia from 2022 to 3rd quarter 2023, by revenue (in million Russian rubles)
Trust in AI in healthcare in Russia 2023, by age group
Do you think it is possible to trust Artificial Intelligence (AI) algorithms in making diagnoses, prescribing treatment, and research and monitoring of patients' diseases?
Digital health
- Premium Statistic Revenue in the Digital Health market Russia 2018-2028
- Premium Statistic Number of users in the Digital Health market Russia 2017-2027
- Premium Statistic Revenue in the eHealth market Russia 2017-2027
- Premium Statistic Number of users in the eHealth market Russia 2017-2027
- Premium Statistic Telemedicine ARPU in Russia 2017-2021
- Premium Statistic Most visited health & medicine websites in Russia 2023
- Premium Statistic Attitudes toward telemedicine use in Russia 2022
- Premium Statistic Preferred telemedicine formats in Russia 2022
Revenue in the Digital Health market Russia 2018-2028
Revenue in the Digital Health market for different segments Russia from 2018 to 2028 (in million U.S. dollars)
Number of users in the Digital Health market Russia 2017-2027
Number of users in the Digital Health market for different segments Russia from 2017 to 2027 (in million individuals)
Revenue in the eHealth market Russia 2017-2027
Revenue in the eHealth market for different segments Russia from 2017 to 2027 (in million U.S. dollars)
Number of users in the eHealth market Russia 2017-2027
Number of users in the eHealth market for different segments Russia from 2017 to 2027 (in thousand individuals)
Telemedicine ARPU in Russia 2017-2021
Average revenue per user (ARPU) of the telemedicine market in Russia from 2017 to 2021 (in Russian rubles)
Most visited health & medicine websites in Russia 2023
Leading health & medicine websites in Russia in August 2023, by monthly visits (in millions)
Attitudes toward telemedicine use in Russia 2022
Attitudes toward telemedicine services and their use in Russia as of June 2022
Preferred telemedicine formats in Russia 2022
Most popular telemedicine formats in Russia as of June 2022
Further reports Get the best reports to understand your industry
Get the best reports to understand your industry.
Mon - Fri, 9am - 6pm (EST)
Mon - Fri, 9am - 5pm (SGT)
Mon - Fri, 10:00am - 6:00pm (JST)
Mon - Fri, 9:30am - 5pm (GMT)
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Health Care, Medical Practice, and Medical Ethics in Russia Today
From the Department of Medicine, University of North Carolina at Chapel Hill (Dr Cassileth), the Department of Community and Family Medicine, Duke University School of Medicine, Durham, NC (Dr Cassileth), and the Department of Aerospace Medicine, Saratov Medical University, Saratov, Russia (Dr Vlassov). Mr Chapman is a research assistant for Dr Cassileth.
FOR DECADES Russian leaders sacrificed health care to the financial and human resource needs of military and space efforts. Centralized and government controlled in every respect, Soviet health care became disjointed, inequitable, and inadequate. 1 Presumably egalitarian, the health care system was in fact strictly hierarchical. Bribery to obtain better quality care was common. Physicians had access only to Soviet medical literature. The government concealed information about scientific and clinical advances produced outside of the Soviet Union from most physicians and the general public. Limited information was available, but only in restricted areas of selected central libraries in Moscow and Leningrad (now St Petersburg). Concurrent environmental pollution, alcoholism, 2 tobacco addiction, and poor nutrition led to public health crises of major proportions. 3
For editorial comment see p 1622.
Soviet leaders withheld internationally accepted standards of medical ethics, human rights, and patient protection. Thus, Soviet medical ethics did not protect
Cassileth BR , Vlassov VV , Chapman CC. Health Care, Medical Practice, and Medical Ethics in Russia Today. JAMA. 1995;273(20):1569–1573. doi:10.1001/jama.1995.03520440021017
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Integr Care
- v.1; Jan-Mar 2001

Integrated health care in Russia: to be or not to be?
Mikko a. vienonen.
WHO Special Representative of the Director General in Russia, WHO Office, 28 Ostozhenka St., 119034 Moscow, Russian Federation. Phone: +7-095-787 21 66 Fax: +7-095-787 21 19
Ilkka J. Vohlonen
Center for Pharmaceutical Policy and Economics, University of Kuopio, P.O. Box 1627, FIN-70211 Kuopio, Finland. Phone: + 358 17 162 592 Fax: +358 17 162 515
The purpose of this paper is to look at what has happened in Russia during the last ten years in the health care sector from the point of view of integrated care. This country, when it still was the leading subject of the Soviet Union, hosted in 1978 the Alma Ata Conference on Primary Health Care, which in many countries gave a strong boost on the development of multidisciplinary, community based care in a gate-keeper position. In Soviet Russia, PHC became marginalised and identical to poor level of care in remote areas of the country where people had very little choice and did not want to use it. Has the situation changed, and is Russia in practice addressing the problems created by the lack of integration, vertical treatment structures and over specialisation?
In addition to the data sources that are referred to in the text, this paper is based on “gray literature” available in project reports and governmental documents, and on the personal experiences of the authors, who have worked for long periods of time in the Russian Federation as international experts dealing with health sector reforms and health policy formulation.
Introduction
About 146 million Russians live in a federation of 89 states. The federal legal assembly (Duma) is elected by direct vote, as well as the 89 regional assemblies. The federal and the regional assemblies have both legislative and taxation powers.
Russian health care has existed for decades in a society with a federal administration of 89 “Federal Subjects”, i.e. republics and regions (“oblasts”). Their average size is about 2 million inhabitants, which is more than in many European states. Their geographical size can be bigger than the whole of Western Europe (e.g. Krasnoyarsk and Yakutia).
The Soviet era saw the transformation of a rudimentary health care system of Tsarist times and created a substantial inheritance for the present Russian Federation. The advantages of this development were:
- Free access to health care;
- Extensive prevention of infectious diseases;
- Developed curative service infrastructure;
- Abundance of trained health personnel;
- Primary health care via rural and urban health posts or city policlinics;
- Public health services network through Sanitary Epidemiological system;
- Occupational health services;
- Health administration—experienced and authoritative;
- Many statistical information sources and;
- Scientific institutions for medical and health systems research.
Despite the real strengths and opportunities evident above, there are also enormous burdens on the health care system, some of which are directly associated with those features listed as positive. The belief that health care is free at the point of use is shared by the whole nation but is linked to excessive expectations and to unrealistic demands. People feel entitled to unlimited access to health services, and do not understand or respect the gatekeeper function. Recently performed household surveys indicate that approximately 30–50% of the total health care expenditure today comes directly from the patients' pockets. A substantial proportion of this is due to purchasing of pharmaceuticals by the patients.
The health infrastructure has expanded beyond any justified boundaries. There is a large amount of over capacity in terms of polyclinics, hospitals, beds and personnel. The continued existence of parallel health systems sponsored by public and private enterprises and by other ministries (e.g. Defence, Interior, Railways, etc.) exacerbates this issue. The question about over-capacity is a political taboo at all levels. The density of physicians is still rising, although the intake of medical students whose education is paid for by the state has decreased. Medical faculties are now allowed to train also students who pay fully their training expenses. Furthermore, most doctors continue to work way beyond the official retirement age. Quitting of work seems to be mainly dependent on the decision of the individual physician.
The primary health care system, although it exists as a collection of physical settings and staff, is poorly thought through and under utilised. Patients express little confidence in the feldshers and district doctors who are nominally the first point of contact. The concept of community outreach does not exist and disease prevention is seen as screening and periodic health check-ups. Health promotion is perceived as traditional health education (brochures and posters), not as a need for broader policy measures. There has not been a tradition of evidence based practice. Old practices and individual improvisation are encouraged. Although not just typical of Russia, non-evidence-based practices have proven very resilient to change both from professionals' and the patients' side.
After the demise of the Soviet Union, the economy of the Russian Federation collapsed in many areas of society and the country experienced hyperinflation. This resulted in the drastic devaluing of health sector expenditure and a financial crisis within the health system (see Table 1 ). The failure to pay health care institutions, or indeed staff, led to an ever greater reliance on unofficial out-of-pocket payments for pharmaceuticals and supplies and on under-the-table payments for the most basic of services [ 1 ].
Government expenditures on health (1991=100%)
Source [ 2 ]: Calculated from the CSO (State Statistical committee) data using GDP deflator indices.
Although the collapse of the Soviet Union has been an unmitigated disaster for the population in terms of health, the causes of this were to be found behind the retrospective latency time. Similar examples from some decades before can be found from the earlier experiences e.g. in China, Scotland and Finland. The decline in Russian health status has been profound with life expectancy plummeting and almost all other health indicators nose-diving (see Figure 1 ). Some of this trend may be attributable to an ongoing neglect of non-communicable diseases that predated the establishment of the Russian Federation. Some may be due to shifts in data collection and reporting methods. However, it is evident that there has been a real and appreciable worsening of the population's health [ 3 ]. Middle-aged men in particular seem to lack the coping mechanisms to deal with such upheaval. They have developed damaging survival strategies, including inappropriate risk taking (dangerous driving, violence) and worsening health behaviours (smoking, drinking, substance misuse) which have all contributed to escalating mortality rates. There is growing evidence also about the increasing incidence of other non-infectious diseases e.g. the incidence of breast cancer among Russian women.

Years of life expectancy at birth in European Union (EU), Countries of Central and Eastern Europe and the Russian Federation 1970–1998. Source: WHO Regional Office for Europe, HFA database 2000.
The realisation that in the first four years of the existence of the Russian Federation there were a million extra deaths, which would not have occurred had the age and sex specific death rates for 1991 been maintained, was a salutary reminder to planners and politicians that reform was needed.
Legislative and financial changes in Russian health care sector
The reform of the health sector was prompted by numerous collapses in the economy and the pressing need to build cost containment and efficiency into the system, combined with fears about health status and a long overdue recognition of the political aspirations of the regions for more autonomy. The previously highly vertical administrative structure (from federal level to individuals) was to be replaced by horizontal regional and local structures. However, the reform process has not simply been a response to irresistible pressures. Health sector reform was also seen as a real opportunity to address the concerns of planners, providers and population about
- the system's ability to respond to local concerns and to non-infectious diseases;
- the balance between primary and secondary, general and specialist, inpatient and outpatient;
- equity between individuals and between regions;
- the implications of under-the-table payments for equity, quality, and humanity of care.
Presently there are at least 25 laws in the field of health and health care, starting from Article 41 of the Constitution of the Russian Federation. Additionally, there are 16 Decrees and Edicts, 8 “Concepts” (“white papers”) and 8 other administrative documents. However, many of these are not yet co-ordinated and fully compatible with each other. Due to the changing administrative structure, the federal, regional and local policies have not been fitted together and the horizontal integration of health care with the intersectoral activities at various levels of governance is missing. National health policy, as WHO understands it, does not yet exist. However, some of the “Concepts” come relatively close to what can be understood as “health care policy”, although the goals have been set very broadly without clear numerical targets such as numbers of hospital beds per population, training of doctors and nurses, future of parallel health services, out-of-pocket payments, etc. However, some regional (state specific) health policy documents have already been developed e.g. in Chelyabinsk and Vologda regions.
New health insurance legislation became effective from the beginning of 1993. The aim was to supplement health care allocation at all levels (federal, regional and local) by traditional funds provided by the compulsory Mandatory Health Insurance. In theory, all citizens are guaranteed basic medical care. In practice it does not work. The premiums, 3.6% of salaries, are collected from employers, while the local government should cover the cost of care for the non-employed (e.g. the children, pensioners and the disabled) by making contributions to the medical insurance fund. In reality more than half of municipalities do not give their contribution stipulated by law to health insurance but instead prefer to give their subsidies directly to health care institutions. In some of the 89 regions, the regional taxes are also used to finance health care. The Russian health insurance system continues to confront major problems of implementation. The low pay of physicians (average official salaries in the range of $40–50 per month) provides a poor base on which to build a structure of incentives, and the country still lacks the service-infrastructure, which could facilitate change.
Many figures for health care expenditure in the Russian Federation are problematic due to issues in the reporting of finances. The indicators widely used in OECD-countries are absent and make international comparisons complex. Core areas of concern are the budget provided by the parallel health system, which go unrecorded.
The precise amount being spent in the various oblasts now exercising independent control and deviating from expected norms is not usually known. In addition, little is done to record the amounts of money raised by the sale of services within the hospital and polyclinic system and there is no way of recording the extent of under-the-table payments or the financial incentives provided by the pharmaceutical industry to the individual physicians. Further complexity is added to estimates by the experience of rapid inflation and changes in governmental approaches to recording.
Between 1990–1995 Russian Statistical Commissions estimated that only 3.2–4.5% of GDP was devoted to health sector. Other sources have described health spending at a higher percentage share of GDP. One of the latest of these is the World Health Report 2000 [ 4 ], which estimates as an internationally comparable figure for Russia (1997) the total expenditure for health as share of GDP 5.4%. Public expenditure of this is estimated as 76.9% and private (out-of-pocket) expenditure 23.1%. The Russian estimates for actual money spent per capita in 1990–1995 ranged from $245 to $23. However, to estimate this in purchasing power is difficult, as the value of rouble against dollar was changing constantly and rapidly. The World Health Report (2000) estimated that the total per capita expenditure in Russia was $251 (in “international dollars”) in 1997. To compare, in 1997 the same figure in Poland was 1.6 times higher, in the UK 4.6 times higher and in the Netherlands 7.6 times higher than in the Russian Federation. At a similar level with Russia were countries like Latvia, Malaysia, Peru and Turkey. This comparison is further complicated by the fact that many Russian health care expenditures are included e.g. in the industrial production costs.
The fact that health sector personnel are paid relatively low salaries goes some way to protecting the purchasing power of the health budget. However, the privatisation of pharmaceutical, energy and food supplies has created a rapid inflation in the cost of these inputs. Prices for particular goods are comparable with those in countries with far higher GDP per capita and this places further strains on health budgets.
There are clear trends that the proportion of money spent on capital investment has declined dramatically from a high point in the 1970s when building and expansion was taking place. Building programmes have ceased in many areas altogether and there has also been a marked decline in the money spent on equipment. Pharmaceuticals are taking up a greater share of the budget, largely as the result of rising costs and an opening up of the market to imports. However, the percentage spent on inpatient care is largely static, despite statements by planners and policy makers that they would encourage a shift to primary care and preventive measures. The cost-plus budgeting system does not allow for incentives to alter the structure of service supply.
Health care reform in Russia and the quest for integrated care
The Soviet system traditionally focused on inpatient, secondary and tertiary care at the expense of outpatient primary and preventive medicine. This is not very different from the history in the Western developed countries. Funding mechanisms, which linked hospital budgets to bed numbers thus creating perverse incentives for hospital doctors to keep open and fill unnecessary beds, then perpetuated the over-provision of beds. By 1991 the bias towards hospital-based care was deeply entrenched and hospitals were absorbing the excessive share of resources ( Table 2 ).
Indicators of health care supply to the population in Russian Federation 1985–1998 (population in 146 million in 1998)
Source (Shishkin): CSO (State Statistical Committee) 1997 & 1999 and USAID, 1999.
The intention of the reform programme was originally very much to increase quality and patient choice but also to address the imbalance between hospital and primary medical services. Policy-makers assumed that the devolution of funds to insurance companies would create incentives to spend money as efficiently as possible. To the planners of the reforms this implied shifting resources into primary care and preventive medicine. However, insurance companies do not often have the skills or the tools to measure and implement the most cost-efficient approaches, nor do they tend to take the long-term view that would make investment in health promotion worthwhile. Instead, they have tended to fall back on traditional patterns of provision and to perpetuate the imbalance between the secondary and primary sectors. The shift to billing on a fee per case basis and the insurance company taking a percentage of the charges processed as a handling fee have only exacerbated this tendency. These patterns have allowed hospital expenses to continue unchecked. The fee per case approach counteracts other measures of disease prevention, both primary and secondary prevention.
Attempts to shift care to an outpatient mode have also suffered in the face of patient preferences. Traditionally, it was perceived that the least qualified and least able doctors went into primary care and prevention while those that became outpatient specialists in polyclinics were only a rank higher in the professional order. This was one of the drawbacks of the Kemorovo model in West-Siberia, which had polyclinic doctors acting as fundholders. Their lack of authority in the eyes of patients and of other doctors undermined their ability to be effective as budget holders. The best doctors were believed to go into hospital medicine and in consequence patients continue to push for referral to hospitals rather than accepting care in an ambulatory setting. Partly this belief was re-enforced by the insufficient training of general practitioners in most of the 47 medical schools.
The Soviet system also, inadvertently, encouraged patient preferences for hospital admission through its prescription costs policy. Inpatients received pharmaceuticals free of charge while outpatients were expected to pay for pharmaceuticals unless they were exempted due to several privileged categories (e.g. registered invalids, veterans of World War II, pensioners, etc.). This policy continues and it has more impact now when pharmaceuticals are supplied through private sector and are becoming increasingly expensive. Preliminary analysis has shown that e.g. hypertensive patients spend about the equivalent of the cost of a summerhouse on anti-hypertensive pharmaceuticals within their life span. Patients are more likely to benefit financially from hospital admission despite the extra strain this places on the finances of the system as a whole. Rising pharmaceutical cost is a feature of health care expenditure in its own right and it takes up an increasing proportion of total annual health care spending.
Cultural expectations of medical transactions appear to include the belief that each consultation should lead to the prescription of some drug or other. Certainly, consumption of pharmaceuticals before 1991 was relatively high in terms of prescriptions per consultation if not in terms of costs. As the private sector has become involved in the supply of pharmaceuticals and as foreign firms have begun to market directly to consumers, the pressures on doctors to prescribe have increased.
The Ministry of Health, in consultation with external counterparts has taken steps to improve the cost-effective consumption of pharmaceuticals. In July 1994, Ministerial Order number 157 adopted a list of essential drugs, which included 96 drugs in 31 different categories. Hospitals and polyclinics are encouraged to restrict themselves to the administration of drugs listed as essential but compliance is incomplete. There is not a negative list as such. Also, the Constitutional Article 41, which federally allows for a free medical care, does not include the supply of pharmaceuticals.
What has happened in reality, some practical examples?
Russia is a large country. Like a big boat, it changes direction slowly. As the Resolution of the Board meeting of the Ministry of Health of the Russian Federation dated 15 March 2000, in many areas of health care reform, the principle changes in direction have been positive, such as:
- Establishment of health insurance in 1991 and mandatory health insurance in 1993;
- Establishment of legal and methodological framework for general practice in 1998;
- Setting up a system of basic benefits' package in 1998.
However, in spite of good intentions, the current underneath clearly points in another direction. There have been several development projects funded by TACIS of the European Union, the World Bank, and several bilateral agencies in places like St. Petersburg, Kemerovo, Samara, Chelyabinsk, etc. However, after external funding of these pilot projects has finished, the lessons learned have not been actively disseminated to other localities. The official number of GPs working in Russia was 1100 in March 2000. Just to reach a level of one GP per 2000 inhabitants would require about 73,000 practising GPs in Russia. At the present speed, the number of GPs needed will be reached in 100 years. One reason for this is that postgraduate training to a great extent is paid by the trainees themselves or their sponsors.
Polyclinic No 34 in St. Petersburg has 10 GPs who have been trained by Swedish funding in Russia and in Sweden. Strikingly, a reception room does not have any equipment for injections or any other procedures to which a western-trained GP would be used. The explanation is that according to the public health (“San-Epid”) rules of the Federal Ministry of Health, such manoeuvres are only allowed in specifically designed premises. Gynaecological examinations are not allowed either. They can only be performed by a gynaecologist. Children under 15 are not allowed to be treated by a Russian GP, as this is the domaine of a paediatrician.
The mere good intention does not turn a boat, whether big or small. Real action is needed also in the infrastructure. So far no one in Russian health policy has really wanted to challenge the establishment of specialist clinics, which are bound to experience a major decline in their clientele—and revenues—if the first contact level (general practice) really is allowed to function. The changes in the infrastructure are prerequisites which include at least the reorientation of educational and manpower policy, reimbursement policy, budgeting policy, and capital investment policy.
Conclusions
As was indicated earlier in the paper, the views presented in this article are partially based on the personal experience of the authors and on “gray literature”. Therefore, generalisations are difficult in Russia because of its vast geographical size and because all 89 “Federal Subjects” (regions, republics, autonomic areas, etc.) can be very different when it comes to health care implementation. The following conclusions and predictions of the future need to be made with great caution.
A major shift in the health of the Russian population has resulted in a rapid rise of non-infectious diseases e.g. cardiovascular diseases, cancer and accidents. In addition, some infectious diseases have increased due to a deterioration of some previously systematic approaches in public health practices and new social behavioural patterns e.g. the sexually transmitted diseases.
Areas of special concern include the continuing pressures on health status that arise from the chaotic socio-economic conditions and the emerging inequities. Much was expected from the shift to insurance and great reliance was placed on its quasi-market elements to create incentives for efficiency and equity of care.
The insurance system has never functioned as first envisaged. Public policies on business practices were simply not in place, not to mention the necessities of controlling the causes and consequences of market failures in health care. It is necessary to modify the structures as it has become increasingly clear that the private sector insurance companies were not emerging and where they did, they could not be entrusted with lump sum payments that represented the planned health care expenditure for whole populations. Their role in quality control could not come into being, as quality indicators are poorly developed and as most insurance companies could not understand what good quality in health care was about.
There are some positive signs that trained primary health care doctors (general practitioner/family doctor) in Russia as anywhere else can gain trust from their catchment population. However, as long as PHC remains the lowest level in the hierarchical health care system under the administrative and financial control of superseding specialist structures, it is unlikely that the situation would change. If more patients were treated at the first contact level, it would undermine the income of any professional group above them. Furthermore, denial of referral, albeit unnecessary, would undermine the income of the first contact doctor, who receives additional income for making an effective and quick referral. The appropriate economic incentives of PHC are not in place.
For the time being, it is unreasonable to assume a quick change towards integrated care in Russia. There are too many powerful groups who would feel that they would lose out and the medical training structure does not provide adequate professional support or infrastructure for a change. The general public does not perceive well-developed primary health care as a realistic option for them, either. The group of general practitioners is too small, and with the speed they are being trained (by 1999 approximately 5000, about 0.7% of all doctors), they will remain so for a long period.
On the other hand, if the political will would be in place—beyond well meaning concepts and resolutions—it might be possible to have relatively rapid progress, especially now as the Russian economy due to high oil prices is relatively strong. After all, in Russia the responsibility for planning, implementing and financing of medical education is one of the key roles of the Ministry of Health of the Russian Federation. As long as general practitioners and family nurses are rare, a team consisting of a first level internist, paediatrician and obstetrician could become a primary health care team with a fixed catchment population and capitation payment. However, they would need good supervision, to be liberated from the constrictive control of the second level specialists, and they need to be empowered to treat their patients at the first contact level.
For an integrated Russian health care, the resources and the means are there—but the appropriate incentives are not.
Contributor Information
Mikko A. Vienonen, WHO Special Representative of the Director General in Russia, WHO Office, 28 Ostozhenka St., 119034 Moscow, Russian Federation. Phone: +7-095-787 21 66 Fax: +7-095-787 21 19.
Ilkka J. Vohlonen, Center for Pharmaceutical Policy and Economics, University of Kuopio, P.O. Box 1627, FIN-70211 Kuopio, Finland. Phone: + 358 17 162 592 Fax: +358 17 162 515.

COMMENTS
Вackground In the last two decades, health care systems (HCS) in the European countries have faced global challenges and have undergone structural changes with the focus on early disease prevention, strengthening primary care, changing the role of hospitals, etc. Russia has inherited the Semashko model from the USSR with dominance of inpatient care, and has been looking for the ways to ...
By the end of 2021 Russia's values of this indicator were higher than in most advanced countries, while healthcare spending decreased to 6.3% of GDP compared to 7.1% of GDP in 2020. The causes of the high mortality rate from COVID-19 and the increased mortality rate from all causes require special research.
First, seven years of "optimizing" the health care system have significantly reduced not only inefficiencies, but also the capacity of the system to deal with the current crisis. The number of Russian epidemiologists has fallen from 33,300 in 1990 to 13,300 in 2018, while the number of beds for infectious diseases fell from 140,000 to 59,000.
Only since 2005, after an increase in budget allocations, spending on healthcare reached 3.7% of GDP. Despite a certain positive trend (an increase in spending on health care to 4.3% of GDP in 2009), in 2013-2014, health financing fell again to 3.2% of GDP. In 2016, this rate was 3.6% of GDP.
The paper (part 1) analyzes the dynamics of indicators characterizing the state of health of the Russian population. A comparative analysis of the development of healthcare in Russia and other countries is carried out. ... T. Foubister, and E. Mossialos, Financing Health Care in the European Union (WHO Regional Office for Europe, Copenhagen ...
Ambulance car-based GAZelle is the most common type of ambulance in Russia. Healthcare in Russia is provided by the state through the Federal Compulsory Medical Insurance Fund, and regulated through the Ministry of Health. The Constitution of the Russian Federation has provided all citizens the right to free healthcare since 1993. In 2008, 621,000 doctors and 1.3 million nurses were employed ...
The study of the models of the private healthcare system in the USA and the mixed model of Russia also allows tracing the capabilities of each of them in developing the strategy of combatting the new virus and implementing guarantees of the basic human right recognized by the international community. The authors consider some problematic ...
The Lancet. 2017. Vol. 390. No. 10102. P. 1612-1613. Shishkin S. The Russian health care system retains the main characteristics of medical care delivery in the Soviet Union. However the transition from socialism to capitalism in the 90s and the economic growth in the 2000s had a significant impact on accessibility of medical care.
The main problem responsible for the limited access to and the poor quality of health care in Russia is the shortage of public health care resources. Medical care requirements went up by at least 46 percent in the period from 1990 to 2008, while the degree of medical care guaranteed by the government remained at the old "Soviet" level.
Working papers from the Economics Department of the OECD that cover the full range of the Department's work including the economic situation, policy analysis and projections; fiscal policy, public expenditure and taxation; and structural issues including ageing, growth and productivity, migration, environment, human capital, housing, trade and investment, labour markets, regulatory reform ...
Russia's health system is both inefficient and inequitable. Sergey Shishkin and Vasiliy Vlassov describe the challenges it faces and the government's plans for reform The transition to a ...
The main social indicator influenced by the reform of the health system in Russia is public health. Public health is a set of characteristics of the population health of the state as a single functioning organism based on the analysis of medical and demographic indicators. The state of public health has a significant impact on the economic ...
A Bloomberg report ranked Russian healthcare last out of 55 developed countries based on the efficiency of state healthcare systems. Russian citizens seem to be of a similar opinion, with only 2% saying they were proud of the Russian healthcare system in a 2016 survey by Moscow-based polling agency Levada Center.
In 1993, under the Russian Constitution, the right to free health care was guaranteed to every Russian citizen. Thus far, the healthcare system in Russia is subpar and even described with such words as "grim" and "bleak.". Health care facilities are lacking, resources are limited, and public health is not a priority to Russian Citizens.
In Russia, as a result of optimization, the opposite trend was observed: in the total number of people employed in the economy, the number of people employed in health care and social services decreased from 6.8% in 2000 to 6.0% in 2019. Lessons learned from the COVID-19 pandemic.
The main burden of Russian health care is that it carries high costs for maintaining the health of people older than 65 years, which are 4-5 times higher than for maintaining the health of people younger than 65 years. The growth of chronic diseases in Russia creates new long-term needs for medical services on the basis of constant interaction ...
To explain the observed differences, I focus on the institutional background to the current state of healthcare systems in Russia and Latvia. Acknowledgements This essay is an output of a research project implemented as part of the Basic Research Program at the National Research University Higher School of Economics (HSE University).
Government expenditure on healthcare in Russia from 2019 to 2024, by source (in billion Russian rubles) Premium Statistic Number of medical laboratory services users in Russia 2017-2022
There is universal health coverage in the Russian Federation, with all citizens entitled to free care in state and municipal medical facilities through social health insurance funded by a mixture of general taxation and employer contributions. Despite this, in practice the quality and availability of services are highly variable across regions.
FOR DECADES Russian leaders sacrificed health care to the financial and human resource needs of military and space efforts. Centralized and government controlled in every respect, Soviet health care became disjointed, inequitable, and inadequate. 1 Presumably egalitarian, the health care system was in fact strictly hierarchical. Bribery to obtain better quality care was common.
The program major activities. The major objective of the program is to reduce the shortage of physicians and nurses with focus on primary care. While the government recognizes the existence of a critical imbalance in the health workforce, there is an inadequate study and debate on how best to improve the scope and impact of the program's interventions and investments.
Health Care in Russia. Russia also officially known as the Russian Federation is a country in northern Eurasia.It is a federal semi-presidential republic. From northwest to southeast, Russia shares land borders with Norway, Finland, Estonia, Latvia, Lithuania and Poland (both with Kaliningrad Oblast), Belarus, Ukraine, Georgia, Azerbaijan ...
Abstract. The purpose of this paper is to look at what has happened in Russia during the last ten years in the health care sector from the point of view of integrated care. This country, when it still was the leading subject of the Soviet Union, hosted in 1978 the Alma Ata Conference on Primary Health Care, which in many countries gave a strong ...