History of the National Cancer Institute
Although cancer has plagued the world for the entirety of human history, it was not until the early 1900s that people came together to create prominent cancer advocacy associations worldwide and to develop national cancer legislation in the United States. In March of 1930, the Senate Commerce Committee heard the testimony of leading cancer researchers, advocates, and other cancer specialists. They told stories of cancer incidence in the United States, explained possible cures, and expressed the need for a national clinic. Since then, multiple legislative acts and amendments have broadened the role of NCI in supporting and improving cancer research.
Discover more about our history .

The National Cancer Act of 1937
In 1937, Congress established the National Cancer Act of 1937 to provide additional support for cancer research—it was the first time Congress had appropriated funds toward a noncommunicable disease. The act, signed by President Franklin D. Roosevelt, established the National Cancer Institute (NCI) as the federal government's primary agency to address research and training needs for the cause, diagnosis, and treatment of cancer. NCI’s responsibilities included:
- conducting, coordinating, and promoting research and studies relating to the cause, diagnosis, treatment, and prevention of cancer
- reviewing and approving grant applications to support promising cancer research
- providing training and instruction in the diagnosis and treatment of cancer
- assisting and promoting similar research at other public and private institutions
- receiving advice from cancer experts in the United States and abroad
- cooperating with state health agencies in the prevention, control, and eradication of cancer
- collecting, analyzing, and disseminating the results of cancer research conducted in the United States and in other countries
The act called upon NCI to assist and promote similar research at other public and private institutions and merged the Office of Cancer Investigations at Harvard University with a pharmacology division of NIH to create NCI as an independent research institute within the division of the Public Health Service (independent of NIH).
The act also established the National Advisory Cancer Council (now known as the National Cancer Advisory Board [NCAB] ), which was authorized to review all research projects for approval before recommending funding by the surgeon general, who was directed to “provide for, foster, and aid in coordinating research related to cancer within NCI and among other agencies and organizations.”
The National Cancer Act of 1971

President Roosevelt's 1940 Dedication of the First NCI Building
On October 31, 1940, President Franklin D. Roosevelt delivered a speech dedicating the first six buildings of the new National Institute of Health in Bethesda, Maryland. Building 6, as noted in this video excerpt, was NCI's first official building.
In 1944, Congress approved the Public Health Service Act of 1944 (42 U.S.C. 201) , which substantially consolidated and revised all existing legislation relating to the Public Health Service. This act also had direct effects on NCI because it made the institute an operating division of the National Institutes of Health (NIH). The National Cancer Act of 1971 expands upon these authorities. This act, signed by President Richard Nixon, created the National Cancer Program and:
- Granted the director of NCI broad authority to plan and develop an expanded, intensified and coordinated National Cancer Program that included NCI and related programs, other research institutes and federal and nonfederal programs “in order to more effectively carry out the national effort against cancer."
- Provided the NCI director with direct access to the President of the United States and required the NCI director to submit an annual budget proposal, called the “professional judgement budget,” directly to the President, bypassing the approval of the NIH director or HHS, as required of other NIH institutes.
- Mandated that NCI develop its programs with the advice of a National Cancer Advisory Board (NCAB), a presidentially appointed committee of 18 members, including both distinguished scientists and laypersons from the general public and 12 ex-officio members from other government agencies, and established the President's Cancer Panel (PCP), a three-member panel, which was specifically required to submit an annual report to the President and hold periodic public hearings.
- Provided additional funding for NCI, establishing 15 new cancer research centers, local cancer control programs, and an international cancer research data bank.
- create new cancer centers and physician and researcher training programs
- appoint advisory committees, allowing the director to explore new issues/opportunities
- expand the physical location at NIH and other research facilities across the country
- award contracts for research
- collaborate with other federal, state, or local public agencies and private industry
- conduct cancer control activities
- establish an international cancer research data bank that collects, catalogues, stores, and disseminates results of cancer research
- award research grants
History, Evolution, Milestones in Cancer Research and Treatment
- Living reference work entry
- First Online: 15 July 2023
- Cite this living reference work entry
- Indu Sharma ORCID: orcid.org/0000-0001-9846-9787 4 ,
- Anuradha Sharma ORCID: orcid.org/0000-0001-5975-1456 4 ,
- Reena Tomer ORCID: orcid.org/0000-0003-1133-763X 4 ,
- Neha Negi ORCID: orcid.org/0000-0002-1902-7081 4 &
- Ranbir Chander Sobti 5
52 Accesses
The historical findings of patients with cancer from ancient Egyptian and Greek civilizations support the millennium long medical history of cancer. However, the disease at that time was mostly treated with not so effective radical surgery and cautery, making death the ultimate outcome of cancer patients. Over the centuries, various breakthrough discoveries have not only reformed the cancer detection but also contributed to the development of more effective therapeutic approaches. The most significant of them was the unearthing of cytotoxic antitumor drugs and the inception of chemotherapy. Since then, an exponential progress has been witnessed over the time about new cancer drugs. Another revolution in the field of oncology was targeted therapy with the development of specific drugs for some molecular targets involved in vital neoplastic processes. Collectively, chemotherapy and targeted therapy have definitely enhanced not only the survival rate but also the quality of life of cancer patients. In present times, genetic engineering studies have amplified the further advancements of cancer biology by utilizing monoclonal antibodies and immune checkpoint inhibitors specifically for advanced or metastatic tumors. Hence, cancer research has continuously grown with an intend to develop newer and better therapeutic approaches for cancer. Most recent, artificial intelligence and precision medicine are certainly going to bring a new revolution in the field of medical oncology.
- Chemotherapy
- Radiotherapy
- Targeted Therapy
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Alverson DC, Krupinski EA, Erps KA, Rowe NS, Weinstein RS (2019) The third national telemedicine & telehealth service provider showcase conference. Telemed J E Health 25(4):332–340. https://doi.org/10.1089/tmj.2018.0096
American Cancer Society. www.cancer.org | 1.800.227.2345
Amiri-Kordestani L, Blumenthal GM, Xu QC, Zhang L, Tang SW, Ha L, Weinberg WC, Chi B, Candau-Chacon R, Hughes P, Russell AM, Miksinski SP, Chen XH, McGuinn WD, Palmby T, Schrieber SJ, Liu Q, Wang J, Song P, Mehrotra N et al (2014) FDA approval: ado-trastuzumab emtansine for the treatment of patients with HER2-positive metastatic breast cancer. Clin Cancer Res 20(17):4436–4441. https://doi.org/10.1158/1078-0432.CCR-14-0012
Article CAS PubMed Google Scholar
Andriole GL, Bostwick DG, Brawley OW, Gomella LG, Marberger M, Montorsi F, Pettaway, CA, Tammela TL, Teloken C, Tindall DJ, Somerville MC, Wilson TH, Fowler IL, Rittmaster RS, & REDUCE Study Group (2010) Effect of dutasteride on the risk of prostate cancer. N Engl J Med 362(13):1192–1202. https://doi.org/10.1056/NEJMoa0908127
Azike JE (2009) A review of the history, epidemiology and treatment of squamous cell carcinoma of the scrotum. Rare Tumors 1(1):47–49
Article Google Scholar
Bagnardi V, Blangiardo M, La Vecchia C, Corrao G (2001) A meta-analysis of alcohol drinking and cancer risk. Br J Cancer 85(11), 1700–1705. https://doi.org/10.1054/bjoc.2001.2140
Bakkalci D, Jia Y, Winter JR, Lewis JE, Taylor GS, Stagg HR (2020) Risk factors for Epstein Barr virus-associated cancers: a systematic review, critical appraisal, and mapping of the epidemiological evidence. J Glob Health 10(1):010405. https://doi.org/10.7189/jogh.10.010405
Article PubMed PubMed Central Google Scholar
Basu A, Kuziemsky C, de Araújo Novaes M, Kleber A, Sales F, Al-Shorbaji N, Flórez-Arango JF, Gogia SB, Ho K Hunter, I Iyengar, S John, O John, S Kulatunga G Rajput, VK Ranatunga P, Udayasankaran JG (2021) Telehealth and the COVID-19 Pandemic: International Perspectives and a Health Systems Framework for Telehealth Implementation to Support Critical Response. Yearb Med Inform 30(1):126–133. https://doi.org/10.1055/s-0041-1726484
Bayat Mokhtari R, Homayouni TS, Baluch N, Morgatskaya E, Kumar S, Das B, Yeger H (2017) Combination therapy in combating cancer. Oncotarget 8(23):38022–38043. https://doi.org/10.18632/oncotarget.16723
Article PubMed Google Scholar
Baysal BE, Ferrell RE, Willett-Brozick JE, Lawrence EC, Myssiorek D, Bosch A, van der Mey A, Taschner PE, Rubinstein WS, Myers EN, Richard CW 3rd, Cornelisse CJ, Devilee P, Devlin B (2000) Mutations in SDHD, a mitochondrial complex II gene, in hereditary paraganglioma. Science (New York, N.Y.) 287(5454):848–851. https://doi.org/10.1126/science.287.5454.848
Berger MF, Mardis ER (2018) The emerging clinical relevance of genomics in cancer medicine. Nature reviews. Clin Oncol 15(6):353–365. https://doi.org/10.1038/s41571-018-0002-6
Article CAS Google Scholar
Bergljung L (2005) Sir Geoffrey Keynes 1887–1982. Kirurgisk pionjär, medicinhistoriker, humanist [Sir Geoffrey Keynes 1887–1982. Surgical pioneer, medical historian, humanist]. Svensk medicinhistorisk tidskrift 9(1):147–153
PubMed Google Scholar
Blumberg BS, Larouzé B, London WT, Werner B, Hesser JE, Millman I, Saimot G, Payet M (1975) The relation of infection with the hepatitis B agent to primary hepatic carcinoma. Am J Pathol 81(3):669–682. PMID: 174434 PMCID: PMC2032339
Google Scholar
Burd EM (2003) Human papillomavirus and cervical cancer. Clin Microbiol Rev 16(1):1–17. https://doi.org/10.1128/CMR.16.1.1-17.2003
Article CAS PubMed PubMed Central Google Scholar
Burns MC, O’Donnell A, Puzanov I (2016) Pembrolizumab for the treatment of advanced melanoma. Expert Opin Orphan Drugs 4(8):867–873. https://doi.org/10.1080/21678707.2016.1191348
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults N Engl J Med 348(17):1625–1638. https://doi.org/10.1056
Cancer Genome Atlas Research Network (2008) Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455(7216):1061–1068. https://doi.org/10.1038/nature07385
Chang MH (2011) Hepatitis B virus and cancer prevention. Recent results in cancer research. Fortschritte der Krebsforschung. Progres dans les recherches sur le cancer 188:75–84. https://doi.org/10.1007/978-3-642-10858-7_6
Chen Y, Jia Y, Song W, Zhang L (2018) Therapeutic potential of nitrogen mustard based hybrid molecules. Front Pharmacol 9:1453
Cheng L, Wang Y, Du J (2020) Human papillomavirus vaccines: an updated review. Vaccines 8(3):391. https://doi.org/10.3390/vaccines8030391
Clarke MJ (1998) Ovarian ablation in breast cancer, 1896 to 1998: milestones along hierarchy of evidence from case report to Cochrane review. BMJ 317(7167):1246–1248. https://doi.org/10.1136/bmj.317.7167.1246
Colapietro A, Mancini A, D’Alessandro AM, Festuccia C (2019) Crocetin and crocin from saffron in cancer chemotherapy and chemoprevention. Anti-Cancer Agents Med Chem 19(1):38–47. https://doi.org/10.2174/1871520619666181231112453
Collins FS, Morgan M, Patrinos A (2003) The Human Genome Project: lessons from large-scale biology. Science (New York, NY) 300(5617):286–290. https://doi.org/10.1126/science.1084564
Connell PP, Hellman S (2009) Advances in radiotherapy and implications for the next century: a historical perspective. Cancer Res 69(2):383–392
Cornejo CM, Jambusaria-Pahlajani A, Willenbrink TJ, Schmults CD, Arron ST, Ruiz ES (2020) Field cancerization: treatment. J Am Acad Dermatol 83(3):719–730. https://doi.org/10.1016/j.jaad.2020.03.127
Cragg GM, Newman DJ (2013) Natural products: a continuing source of novel drug leads. Biochimica et biophysica acta 1830(6):3670–3695. https://doi.org/10.1016/j.bbagen.2013.02.008
Crawford ED (2004) Hormonal therapy in prostate cancer: historical approaches. Rev Urol 6(Suppl 7):S3–S11
PubMed PubMed Central Google Scholar
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, Fantin VR, Jang HG, Jin S, Keenan MC, Marks KM, Prins RM, Ward PS, Yen KE, Liau LM, Rabinowitz JD, Cantley LC, Thompson CB, Vander Heiden MG, Su SM (2009) Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 462(7274):739–744. https://doi.org/10.1038/nature08617
DeVita VT Jr, Chu E (2008) A history of cancer chemotherapy. Cancer Res 68(21):8643–8653
Dillard RS, Hampton CM, Strauss JD, Ke Z, Altomara D, Guerrero-Ferreira RC, Kiss G, Wright ER (2018) Biological Applications at the Cutting Edge of Cryo-Electron Microscopy. Microscopy and microanalysis: Microsc Microanal 24(4):406–419. https://doi.org/10.1017/S1431927618012382
Dotan E, Aggarwal C, Smith MR (2010) Impact of rituximab (Rituxan) on the treatment of B-cell non-Hodgkin’s lymphoma. P & T 35(3):148–157
D’Souza G, Kreimer AR, Viscidi R et al (2007) Case-control study of human papillomavirus and oropharyngeal cancer. N Engl J Med 356:1944–1956
Dunn DB (2020) Larotrectinib and entrectinib: TRK inhibitors for the treatment of pediatric and adult patients with NTRK gene fusion. J Adv Pract Oncol 11(4):418–423. https://doi.org/10.6004/jadpro.2020.11.4.9
Elemento O (2021) The road from Rous sarcoma virus to precision medicine. J Exp Med 218(4)
Elion GB, Singer S, Hitchings GH (1954) Antagonists of nucleic acid derivatives. VIII. Synergism in combinations of biochemically related antimetabolites. J Biol Chem 208:477–488
Fisher B, Costantino JP, Wickerham DL, Redmond CK, Kavanah M, Cronin WM, Vogel V, Robidoux A, Dimitrov N, Atkins J, Daly M, Wieand S, Tan-Chiu E, Ford L, Wolmark N (1998) Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 90(18):1371–1388. https://doi.org/10.1093/jnci/90.18.1371
Fröman N (1996) Marie and Pierre Curie and the discovery of polonium and radium. Palestra na royal swedish academy of sciences, em Estocolmo, Suécia
Gilchrest BA (2021) Actinic keratoses: reconciling the biology of field cancerization with treatment paradigms. J Investig Dermatol 141(4):727–731. https://doi.org/10.1016/j.jid.2020.09.002
Gompel A (2019) Hormones et cancers du sein [Hormone and breast cancer]. Presse medicale (Paris, France: 1983) 48(10):1085–1091. https://doi.org/10.1016/j.lpm.2019.09.021
Graziani G, Tentori L, Navarra P (2012) Ipilimumab: a novel immunostimulatory monoclonal antibody for the treatment of cancer. Pharmacol Res 65(1):9–22. https://doi.org/10.1016/j.phrs.2011.09.002
Graziani G, Lisi L, Tentori L, Navarra P (2022) Monoclonal Antibodies to CTLA-4 with Focus on Ipilimumab. Exp Suppl 113:295–350. https://doi.org/10.1007/978-3-030-91311-3_10
Guallar-Garrido S, Julián E (2020) Bacillus Calmette-Guérin (BCG) therapy for bladder cancer: an update. ImmunoTargets Ther 9:1–11. https://doi.org/10.2147/ITT.S202006
Gutierrez C, Schiff R (2011) HER2: biology, detection, and clinical implications. Arch Pathol Lab Med 135(1):55–62. https://doi.org/10.5858/2010-0454-RAR.1
Hammerstrom AE, Cauley DH, Atkinson BJ, Sharma P (2011) Cancer immunotherapy: sipuleucel-T and beyond. Pharmacotherapy 31(8):813–828. https://doi.org/10.1592/phco.31.8.813
Hansford S, Huntsman DG (2014) Boveri at 100: Theodor Boveri and genetic predisposition to cancer. J Pathol 234(2):142–145. https://doi.org/10.1002/path.4414
Hansson N, Moll F, Schultheiss D, Krischel M (2016) Remembering Charles B. Huggins’ Nobel Prize for Hormonal Treatment of Prostatic Cancer at its 50th Anniversary. Eur Uro 69(6):971–972. https://doi.org/10.1016/j.eururo.2016.01.030
Hitchings GH, Elion GB (1954) The chemistry and biochemistry of purine analogs. Ann NY Acad Sci 60:195–199
Hodi FS, Chesney J, Pavlick AC, Robert C, Grossmann KF, McDermott DF, Linette GP, Meyer N, Giguere JK, Agarwala SS, Shaheen M, Ernstoff MS, Minor DR, Salama AK, Taylor MH, Ott PA, Horak C, Gagnier P, Jiang J, Wolchok JD, Postow MA (2016) Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2-year overall survival outcomes in amulticentre, randomised, controlled, phase 2 trial. Lancet Oncol 17(11):1558–1568. https://doi.org/10.1016/S1470-2045(16)30366-7
Howard NP, Troggio M, Durel CE, Muranty H, Denancé C, Bianco L, Tillman J, van de Weg E (2021) Integration of Infinium and Axiom SNP array data in the outcrossing species Malus × domestica and causes for seemingly incompatible calls. BMC genomics 22(1):246. https://doi.org/10.1186/s12864-021-07565-7
Howard KK, Makki H, Novotny NM, Mi M, Nguyen N (2022) Value of robotic surgery simulation for training surgical residents and attendings: a systematic review protocol. BMJ open 12(6):e059439. https://doi.org/10.1136/bmjopen-2021-059439
Hunter B, Hindocha S, Lee RW (2022) The Role of Artificial Intelligence in Early Cancer Diagnosis. Cancers 14(6):1524. https://doi.org/10.3390/cancers14061524
Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S, Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R, Kabbinavar F (2004) Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 350(23):2335–342. https://doi.org/10.1056/NEJMoa032691
ICGC/TCGA Pan-Cancer Analysis of Whole Genomes Consortium (2020) Pan-cancer analysis of whole genomes. Nature 578(7793):82–93. https://doi.org/10.1038/s41586-020-1969-6
Iqbal N, Iqbal N (2014a) Human epidermal growth factor receptor 2 (HER2) in cancers: overexpression and therapeutic implications. Mol Biol Int 2014:852748. https://doi.org/10.1155/2014/852748
Iqbal N, Iqbal N (2014b) Imatinib: a breakthrough of targeted therapy in cancer. Chemother Res Pract 2014:357027. https://doi.org/10.1155/2014/357027
Jensen G (2010) Cryo-EM, Part C: analyses, interpretation, and case studies Academic Press
Yang JE, Larson MR, Sibert BS, Shrum, S, Wright ER (2021) CorRelator: Interactive software for real-time high precision cryo-correlative light and electron microscopy. J Struct Biol 213(2):107709. https://doi.org/10.1016/j.jsb.2021.107709
Jeyakumar A, Younis T (2012) Trastuzumab for HER2-positive metastatic breast cancer: clinical and economic considerations. Clinical medicine insights. Oncology 6:179–187. https://doi.org/10.4137/CMO.S6460
Jones OT, Calanzani N, Saji S, Duffy SW, Emery J, Hamilton W, Singh H, de Wit NJ, Walter FM (2021) Artificial Intelligence Techniques That May Be Applied to Primary Care Data to Facilitate Earlier Diagnosis of Cancer: Systematic Review. J Med Internet Res 23(3):23483. https://doi.org/10.2196/23483
Jordan VC (2014) Tamoxifen as the first targeted long-term adjuvant therapy for breast cancer. Endocr Relat Cancer 21(3):R235–R246. https://doi.org/10.1530/ERC-14-0092
Kaminskas E, Farrell A, Abraham S, Baird A, Hsieh LS, Lee SL, Leighton JK, Patel H, Rahman A, Sridhara R, Wang YC, Pazdur R, FDA (2005) Approval summary: azacitidine for treatment of myelodysplastic syndrome subtypes. Clinical cancer research : Clin Cancer Res 11(10): 3604–3608. https://doi.org/10.1158/1078-0432.CCR-04-2135
Kamps R, Brandão RD, Bosch BJ, Paulussen AD, Xanthoulea S, Blok MJ, Romano A (2017) Next-generation sequencing in oncology: genetic diagnosis, risk prediction and cancer classification. Int J Mol Sci 18(2):308. https://doi.org/10.3390/ijms18020308
Kang TW, Yevsa T, Woller N, Hoenicke L, Wuestefeld T, Dauch D, Hohmeyer A, Gereke M, Rudalska R, Potapova A, Iken M, Vucur M, Weiss S, Heikenwalder M, Khan S, Gil J, Bruder D, Manns M, Schirmacher P, Tacke F, Zender L (2011) Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature 479(7374):547–551. https://doi.org/10.1038/nature10599
Kaufman KD, Dawber RP (1999) Finasteride, a Type 2 5alpha-reductase inhibitor, in the treatment of men with androgenetic alopecia. Expert Opin Investig Drugs 8(4):403–415. https://doi.org/10.1517/13543784.8.4.403
Khatami M (2018) Cancer; an induced disease of twentieth century! Induction of tolerance, increased entropy and ‘Dark Energy’: loss of biorhythms (Anabolism v. Catabolism). Clin Trans Med 7:20. https://doi.org/10.1186/s40169-018-0193-6
Kramer BS, Berg CD, Aberle DR, Prorok PC (2011) Lung cancer screening with low-dose helical CT: results from the National Lung Screening Trial (NLST). J Med Screen 18(3):109–111. https://doi.org/10.1258/jms.2011.011055
Lamm DL, Blumenstein BA, Crawford ED et al (1991) A randomized trial of intravesical doxorubicin and immunotherapy with bacille Calmette-Guerin for transitional-cell carcinoma of the bladder. N Engl J Med 325:1205–1209
Langner E, Rzeski W (2012) Dietary derived compounds in cancer chemoprevention. Contemp Oncol (Poznan, Poland) 16(5):394–400. https://doi.org/10.5114/wo.2012.31767
Lechner M, Liu J, Masterson L, Fenton TR (2022) HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol 19(5):306–327. https://doi.org/10.1038/s41571-022-00603-7
Li MC, Hertz R, Bergenstal DM (1958) Therapy of choriocarcinoma and related trophoblastic tumors with folic acid and purine antagonists. N Engl J Med 259:66–74
Lin R, Tripuraneni P (2011) Radiation therapy in early-stage invasive breast cancer. Indian J Surg Oncol 2(2):101–111. https://doi.org/10.1007/s13193-011-0048-8
Liu C-J, Chen P-J (2020) Elimination of Hepatitis B in highly endemic settings: lessons learned in Taiwan and challenges ahead. Viruses 12(8):815. https://doi.org/10.3390/v12080815
Mansoori B, Mohammadi A, Davudian S, Shirjang S, Baradaran B (2017) The different mechanisms of cancer drug resistance: a brief review. Adv Pharmaceut Bull 7(3):339–348. https://doi.org/10.15171/apb.2017.041
Milani M, Jha G, Potter DA (2009) Anastrozole use in early stage breast cancer of post-menopausal women. Clin Med Ther 1:141–156. https://doi.org/10.4137/cmt.s9
Milani A, Basirnejad M, Shahbazi S, Bolhassani A (2017) Carotenoids: biochemistry, pharmacology and treatment. Br J Pharmacol 174(11):1290–1324. https://doi.org/10.1111/bph.13625
Miller EA, Pinsky PF, Schoen RE, Prorok PC, Church TR (2019) Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: long-term follow-up of the randomised US PLCO cancer screening trial. Lancet Gastroenterol Hepatol 4(2):101–110. https://doi.org/10.1016/S2468-1253(18)30358-3
Monie A, Hung CF, Roden R, Wu TC (2008) Cervarix: a vaccine for the prevention of HPV 16, 18-associated cervical cancer. Biol Targets Ther 2(1):97–105
Monteiro AN, Waizbort R (2007) The accidental cancer geneticist: hilario de gouvea and hereditary retinoblastoma. Cancer Biol Ther 6(5):811–813
Nadel MR, Berkowitz Z, Klabunde CN, Smith RA, Coughlin SS, White MC (2010) Fecal occult blood testing beliefs and practices of U.S. primary care physicians: serious deviations from evidence-based recommendations. J Gen Intern Med 25(8):833–839. https://doi.org/10.1007/s11606-010-1328-7
Newman DJ, Cragg GM (2020) Natural products as sources of new drugs over the nearly four decades from 01/1981 to 09/2019. J Nat Prod 83(3):770–803. https://doi.org/10.1021/acs.jnatprod.9b01285
Nowell PC (2007) Discovery of the Philadelphia chromosome: a personal perspective. J Clin Investig 117(8):2033–2035. https://doi.org/10.1172/JCI31771
Maddocks OD, Berkers CR, Mason SM, Zheng L, Blyth K, Gottlieb E, Vousden KH (2013) Serine starvation induces stress and p53-dependent metabolic remodelling in cancer cells. Nature 493(7433):542–546. https://doi.org/10.1038/nature11743
Marcus L, Lemery SJ, Keegan P, Pazdur R (2019) FDA Approval Summary: Pembrolizumab for the Treatment of Microsatellite Instability-High Solid Tumors. Clinical cancer research : Clin Cancer Res 25(13):3753–3758. https://doi.org/10.1158/1078-0432.CCR-18-4070
Martincorena I, Roshan A, Gerstung M, Ellis P, Van Loo P, McLaren S, Wedge DC, Fullam A, Alexandrov LB, Tubio JM, Stebbings L, Menzies A, Widaa S, Stratton MR, Jones PH, Campbell PJ (2015) Tumor evolution. High burden and pervasive positive selection of somatic mutations in normal human skin. Science (New York, N.Y.) 348(6237):880–886. https://doi.org/10.1126/science.aaa6806
McLaughlin JR, Risch HA, Lubinski J, Moller P, Ghadirian P, Lynch H, Karlan B, Fishman D, Rosen B, Neuhausen SL, Offit K, Kauff N, Domchek S, Tung N, Friedman E, Foulkes W, Sun P, Narod SA, Hereditary Ovarian Cancer Clinical Study Group (2007) Reproductive risk factors for ovarian cancer in carriers of BRCA1 or BRCA2 mutations: a case-control study. Lancet Oncol 8(1):26–34. https://doi.org/10.1016/S1470-2045(06)70983-4
Medical Advisory Secretariat (2010) Robotic-assisted minimally invasive surgery for gynecologic and urologic oncology: an evidence-based analysis. Ont Health Technol Assess Ser 10(27):1–118 PMID: 23074405 PMCID: PMC3382308
Mizuki H, Shimoyama Y, Ishikawa T, Sasaki M (2022) A genomic sequence of the type II-A clustered regularly interspaced short palindromic repeats (CRISPR)/CRISPR-associated system in Mycoplasma salivarium strain ATCC 29803. J Oral Microbiol 14(1):2008153. https://doi.org/10.1080/20002297.2021.2008153
Panahi B, Majidi M, Hejazi MA (2022) Genome mining approach reveals the occurrence and diversity pattern of clustered regularly interspaced short palindromic repeats/CRISPR-associated systems in lactobacillus brevis strains. Front Microbiol 13:911706. https://doi.org/10.3389/fmicb.2022.911706
Paul A, Paul S (2014) The breast cancer susceptibility genes (BRCA) in breast and ovarian cancers. Frontiers in bioscience (Landmark edition) 19(4):605–618. https://doi.org/10.2741/4230
Pérez-Herrero E, Fernández-Medarde A (2015) Advanced targeted therapies in cancer: drug nanocarriers, the future of chemotherapy. Eur J Pharmaceut Biopharmaceut 93:52–79. https://doi.org/10.1016/j.ejpb.2015.03.018
Plesca M, Bordea C, El Houcheimi B, Ichim E, Blidaru A (2016) Evolution of radical mastectomy for breast cancer. J Med Life 9(2):183
CAS PubMed PubMed Central Google Scholar
Raje N, Berdeja J, Lin Y, Siegel D, Jagannath S, Madduri D, Liedtke M, Rosenblatt J, Maus MV, Turka A, Lam LP, Morgan RA, Friedman K, Massaro M, Wang J, Russotti G, Yang Z, Campbell T, Hege K, Petrocca F, Kochenderfer JN (2019) Anti-BCMA CAR T-Cell Therapy bb2121 in Relapsed or Refractory Multiple Myeloma. N Engl J Med 380(18):1726–1737. https://doi.org/10.1056/NEJMoa1817226
Ramalingam SS, Khuri FR (2021) The National Cancer Act of 1971: a seminal milestone in the fight against cancer. Cancer 127(24):4532–4533. https://doi.org/10.1002/cncr.34001
Ramsköld D, Luo S, Wang YC, Li R, Deng Q, Faridani OR, Daniels GA, Khrebtukova I, Loring JF, Laurent LC, Schroth GP, Sandberg R (2012) Full-length mRNA-Seq from single-cell levels of RNA and individual circulating tumorcells. Nat Biotechnol 30(8):777–782. https://doi.org/10.1038/nbt.2282
Redman MW, Tangen CM, Goodman PJ, Lucia MS, Coltman CA Jr, Thompson IM (2008) Finasteride does not increase the risk of high-grade prostate cancer: a bias-adjusted modeling approach. Cancer Prev Res (Philadelphia, PA) 1:174–181
Rivlin N, Brosh R, Oren M, Rotter V (2011) Mutations in the p53 tumor suppressor gene: important milestones at the various steps of tumorigenesis. Genes Cancer 2(4):466–474. https://doi.org/10.1177/1947601911408889
Rock CL, Thomson CA, Sullivan KR, Howe CL, Kushi LH, Caan BJ, Neuhouser ML, Bandera EV, Wang Y, Robien K, Basen-Engquist KM, Brown JC, Courneya KS, Crane TE, Garcia DO, Grant BL, Hamilton KK, Hartman SJ, Kenfield SA, Martinez ME et al (2022) American Cancer Society nutrition and physical activity guideline for cancer survivors. CA 72(3):230–262. https://doi.org/10.3322/caac.21719
Samadi AK, Bilsland A, Georgakilas AG, Amedei A, Amin A, Bishayee A et al (2015) A multi-targeted approach to suppress tumor-promoting inflammation. In: Semin Cancer Biol, vol 35. Academic, pp S151–S184
Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, van Es JH, Abo A, Kujala P, Peters PJ, Clevers H (2009) Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 459(7244):262–265. https://doi.org/10.1038/nature07935
Schrijver LH, Olsson H, Phillips KA, Terry MB, Goldgar DE, Kast K, Engel C, Mooij TM, Adlard J, Barrowdale D, Davidson R, Eeles R, Ellis S, Evans DG, Frost D, Izatt L, Porteous ME, Side LE, Walker L, Berthet P et al (2018) Oral contraceptive use and breast cancer risk: retrospective and prospective analyses from a BRCA1 and BRCA2 mutation carrier Cohort Study. JNCI Cancer Spect 2(2):pky023. https://doi.org/10.1093/jncics/pky023
Slaughter DP, Southwick HW, Smejkal W (1953) Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer 6(5):963–968. https://doi.org/10.1002/10970142(195309)6:5-963::aid-cncr2820060515>3.0.co;2-q
Sottoriva A, Kang H, Ma Z, Graham TA, Salomon MP, Zhao J, Marjoram P, Siegmund K, Press MF, Shibata D, Curtis C (2015) A Big Bang model of humancolorectal tumor growth. Nat Genet 47(3):209–216. https://doi.org/10.1038/ng.3214
Spain PD, Kadan-Lottick N (2012) Observations of unprecedented remissions following novel treatment for acute leukemia in children in 1948. J R Soc Med 105(4):177–181. https://doi.org/10.1258/jrsm.2012.12k013
Sporn MB, Dunlop NM, Newton DL, Smith JM (1976) Prevention of chemical carcinogenesis by vitamin A and its synthetic analogs (retinoids). Fed Proc 35(6):1332–1338. PMID: 770206
Stehelin D, Varmus HE, Bishop JM, Vogt PK (1976) DNA related to the transforming gene(s) of avian sarcoma viruses is present in normal avian DNA. Nature 260(5547):170–173. https://doi.org/10.1038/260170a0
Stein EM, DiNardo CD, Pollyea DA, Fathi AT, Roboz GJ, Altman JK, Stone RM, DeAngelo DJ, Levine RL, Flinn IW, Kantarjian HM, Collins R, Patel MR, Frankel AE, Stein A, Sekeres MA, Swords RT, Medeiros BC, Willekens C, Vyas P, Tallman MS (2017) Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood 130(6):722–731. https://doi.org/10.1182/blood-2017-04-779405
Stellman SD (2006) Ernst Wynder: a remembrance. Prev Med 43(4):239–245. https://doi.org/10.1016/j.ypmed.2006.08.007
Tacklind J, Fink HA, Macdonald R (2010) Finasteride for benign prostatic hyperplasia. Cochrane Database Syst Rev 10:601–615
Tan SY, Tatsumura Y (2015) George Papanicolaou (1883–1962): discoverer of the Pap smear. Singap Med J 56(10):586–587. https://doi.org/10.11622/smedj.2015155
Teh AL, Pan H, Lin X, Lim YI, Patro CP, Cheong CY, Gong M, MacIsaac JL, Kwoh CK, Meaney MJ, Kobor MS, Chong YS, Gluckman PD, Holbrook JD, Karnani N (2016) Comparison of Methyl-capture Sequencing vs. Infinium 450K methylation array for methylome analysis in clinical samples. Epigenetics 11(1):36–48. https://doi.org/10.1080/15592294.2015.1132136
Thompson IM, Klein EA, Lippman SM, Coltman CA, Djavan B (2003) Prevention of prostate cancer with finasteride: US/European perspective. Eur Urol 44(6):650–655. https://doi.org/10.1016/j.eururo.2003.11.001
Tian J, Lai D, Zhou L (2017) Secondary metabolites from Acremonium fungi: diverse structures and bioactivities. Mini Rev Med Chem 17(7):603–632. https://doi.org/10.2174/1389557516666160914194134
Timbang MR, Sim MW, Bewley AF, Farwell DG, Mantravadi A, Moore MG (2019) HPV-related oropharyngeal cancer: a review on burden of the disease and opportunities for prevention and early detection. Hum Vaccin Immunother 15(7–8):1920–1928. https://doi.org/10.1080/21645515.2019.1600985
Timoneda J, Rodríguez-Fernández L, Zaragozá R, Marín MP, Cabezuelo MT, Torres L, Viña JR, Barber T (2018) Vitamin A deficiency and the lung. Nutrients 10(9):1132. https://doi.org/10.3390/nu10091132
Tubiana M (1996) Wilhelm Conrad Röntgen and the discovery of X-rays. Bulletin de l’Académie nationale de médecine 180(1):97–108
CAS PubMed Google Scholar
Ullah MF, Usmani S, Shah A, Abuduhier FM (2022) Dietary molecules and experimental evidence of epigenetic influence in cancer chemoprevention: an insight. Semin Cancer Biol 83:319–334. https://doi.org/10.1016/j.semcancer.2020.10.011
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, Bevers TB, Fehrenbacher L, Pajon ER Jr, Wade JL 3rd, Robidoux A, Margolese RG, James J, Lippman SM, Runowicz CD, Ganz PA, Reis SE, McCaskill-Stevens W, Ford LG, Jordan VC et al (2006) Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA 295(23):2727–2741. https://doi.org/10.1001/jama.295.23.joc60074
Waldman AD, Fritz JM, Lenardo MJ (2020) A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol 20(11):651–668
Wang JJ, Lei KF, Han F (2018) Tumor microenvironment: recent advances in various cancer treatments. Eur Rev Med Pharmacol Sci 22(12):3855–3864. https://doi.org/10.26355/eurrev_201806_15270
Wattenberg LW (1966) Chemoprophylaxis of carcinogenesis: a review. Cancer Res 26:1520–1526
Weinstein IB, Case K (2008) The history of Cancer Research: introducing an AACR Centennial series. Cancer Res 68(17):6861–6862
Yang Y, Arseni D, Zhang W, Huang M, Lövestam S, Schweighauser M, Kotecha A, Murzin AG, Peak-Chew SY, Macdonald J, Lavenir I, Garringer HJ, Gelpi E, Newell KL, Kovacs GG, Vidal R, Ghetti B, Ryskeldi-Falcon B, Scheres SHW, Goedert M (2022) Cryo-EM structures of amyloid-β 42 filaments from human brains. Science (New York, N.Y.) 375(6577):167–172. https://doi.org/10.1126/science.abm7285
Zhang N, Yin Y, Xu SJ, Chen WS (2008) 5-Fluorouracil: mechanisms of resistance and reversal strategies. Molecules (Basel, Switzerland) 13(8):1551–1569. https://doi.org/10.3390/molecules13081551
Zhao L, Cao YJ (2019) Engineered T Cell Therapy for Cancer in theClinic. Front Immunol 10:2250. https://doi.org/10.3389/fimmu.2019.02250
Zhou Y, Zhou W, Zhou J, Yan J, Xu D, Zheng X, Zong S, Jiang P, Tian S, Han J, Qu D (2022) The Clustered Regularly Interspaced Short Palindromic Repeats-Associated System and Its Relationship With Mobile Genetic Elements in Klebsiella. Front Microbiol 12:790673. https://doi.org/10.3389/fmicb.2021.790673
Zhu YS, Tang K, Lv J (2021) Peptide-drug conjugate-based novel molecular drug delivery system in cancer. Trends Pharmacol Sci 42(10):857–869. https://doi.org/10.1016/j.tips.2021.07.001
Download references
Author information
Authors and affiliations.
Department of Zoology, Panjab University, Chandigarh, India
Indu Sharma, Anuradha Sharma, Reena Tomer & Neha Negi
Department of Biotechnology, Panjab University, Chandigarh, India
Ranbir Chander Sobti
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Indu Sharma .
Editor information
Editors and affiliations.
Dept. Biotechnology, Panjab University, Chandigarh, Chandigarh, India
R. C. Sobti
NCR Biotech Science Cluster, Translational Health Sci & Tech Inst, Faridabad, Haryana, India
Nirmal K. Ganguly
National Chair in Cancer Research, Rajiv Gandhi Center for Biotechnology, trivandrum, Kerala, India
Rakesh Kumar
Section Editor information
Swami Rama Himalayan University, Dehradun, Kerala, India
NCR Biotech Science Cluster, Translational Health Science and Technology Institute, Faridabad, India
Rights and permissions
Reprints and permissions
Copyright information
© 2023 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry.
Sharma, I., Sharma, A., Tomer, R., Negi, N., Sobti, R.C. (2023). History, Evolution, Milestones in Cancer Research and Treatment. In: Sobti, R.C., Ganguly, N.K., Kumar, R. (eds) Handbook of Oncobiology: From Basic to Clinical Sciences. Springer, Singapore. https://doi.org/10.1007/978-981-99-2196-6_2-1
Download citation
DOI : https://doi.org/10.1007/978-981-99-2196-6_2-1
Received : 08 April 2023
Accepted : 13 April 2023
Published : 15 July 2023
Publisher Name : Springer, Singapore
Print ISBN : 978-981-99-2196-6
Online ISBN : 978-981-99-2196-6
eBook Packages : Springer Reference Biomedicine and Life Sciences Reference Module Biomedical and Life Sciences
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Advertisement

- Next Article
Acknowledgments
The history of cancer research: introducing an aacr centennial series.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
- Version of Record August 28 2008
I. Bernard Weinstein , Kathleen Case; The History of Cancer Research: Introducing an AACR Centennial Series. Cancer Res 1 September 2008; 68 (17): 6861–6862. https://doi.org/10.1158/0008-5472.CAN-08-2827
Download citation file:
- Ris (Zotero)
- Reference Manager
A century is only a small segment in the timeline measuring the history of science through the ages, but for cancer research, the last 100 years overshadow all of the years that came before. Physicians have moved from being able to do very little to treat patients to achieving survival and cure rates no one believed possible. Just a few decades ago, young investigators and physicians were often told not to go into oncology because the disease is so complex and the clinical outcomes were so discouraging. Today, oncology is one of the most exciting fields in biomedicine because of the many astonishing advances research continues to yield.
The field of cancer research had begun to grow rapidly by the end of the 19th century and the beginning of the 20th. In Europe, spontaneous tumors had been propagated in mice, and Gaylord and Tyzzer, two of the founders of the American Association for Cancer Research (AACR), soon expanded this research in America. Use of radium and X-rays was in its infancy. American institutes for research were being established (Roswell Park, The Rockefeller Institute, and The Institute of Cancer Research at Columbia University), and private endowments to fund research were beginning to proliferate, although direct government research support was not yet available. The first congresses on cancer had just been held in Europe.
The level of optimism was so high during this period that Roswell Park (who was instrumental in starting the institute at Buffalo now named after him) stated that the discovery of the cause of cancer was “just around the corner” ( 1 ). Within this spirit of enthusiasm, a group of 11 American pathologists, surgeons, and chemists proposed forming an organization. The AACR was founded in Washington DC on May 7, 1907, and its purpose was soon defined as “to further the investigation and spread the knowledge of cancer” ( 2 ).
It is interesting to reflect on what was known about cancer at the time AACR was founded ( 3 ). The earliest theory of cancer was based on the humoral theory of disease articulated by Hippocrates (460–370 BCE). It postulated that the disease was due to an excess of black bile. Apparently, this was not a bad hypothesis since it lasted about 1,900 years! However, during this time, the theory was never challenged by actual inquiry until the Renaissance, when anatomic dissection by Andreas Vesalius and others failed to reveal the existence of black bile. In the 1700s, it was postulated that cancer arose from coagulated lymph. The modern era of cancer research really began in the 19th century and led to the current concept developed by several investigators, notably Rudolf Virchow, that cancer is a disease of cells.
The first insights into human cancer causation occurred in the 18th century with the astute clinical observations by John Hill of the association of the use of snuff with nasal polyps, by Percival Pott of the association of soot with scrotal cancer in chimney sweeps, and by Bernadino Ramazzini of the association of reproductive factors with breast cancer. In the last decade of the 19th century, Ludwig Rehn reported an association between occupational exposure to aromatic amines and bladder cancer, thus setting the stage for the identification during the 20th century of other specific chemical carcinogens in the workplace and the environment.
Early evidence for the multistage and multifactor nature of the carcinogenic process was revealed by the experimental studies of Yamagiwa and Ichikawa at the beginning of the 20th century. Within just a few years after the founding of the AACR, the first tumor viruses were identified in chickens by Ellerman and Bong (1909) and Peyton Rous (1911). A few decades later, the Rous virus provided evidence for the first oncogene (src), and thus launched the field of molecular biology of cancer.
Tumor transplantation was reported by Mistislav Novinsky in 1877 and further studied by Carl Jensen in 1903. The technique of cell culture was established by Carrel and Burrows (1911). Gregor Mendel's Principles of Inheritance (1880) were rediscovered in 1900. The field of mouse genetics had just begun, with pioneering studies by Ernest Tyzzer (1908), as mentioned above, a founder of the AACR. Genetic studies in Drosophila had begun, and in 1914, Theodor Boveri made the prophetic postulate that chromosomes were the carriers of hereditary information and that cancer was due to defects in the chromosomes.
The exciting progress in cancer research during the past century has tended to parallel the successive developments in fundamental biology and biomedical research. Thus, in the late 1800s and early 1900s, the emphasis in cancer research was on cytology and genetics, and genetic studies in mice and humans continued to play a major role in cancer research. This was followed by studies in the field of biochemistry and intermediary metabolism (about 1920 to 1950), studies emphasizing DNA and nucleic acids (about 1950 to the present), studies on receptors and pathways of signal transduction (1980 to the present), and within the past decade, studies on gene transcription, epigenetic control of gene expression, genomics, and systems biology.
The very recent discovery, originally in plants, of the regulatory roles of small RNAs is also providing new insights into the biology of cancer. The latter example, which was totally unanticipated, suggests that within the next few years, other discoveries about fundamental aspects of cell biology will be made that will provide further insights into the wayward behavior of cancer cells. These successive themes have also influenced our understanding of cancer causation and provided new strategies for cancer prevention and treatment. Cancer researchers can take pride in the fact that cancer studies have often played an important role in advancing the broader fields of cell biology and biomedical research.
At AACR's first scientific meeting in 1907, in a small room in New York City, nine papers were presented. Two dealt with using transfusions to treat cancer; five covered transplantation of tumors in experimental animals; and two were meant to dispel the myth that some cancers were really infectious diseases ( 4 ). At the AACR's Centennial Celebration Annual Meeting in 2007 in a large convention center in Los Angeles, there were over 17,000 registrants, and over 6,500 abstracts and papers were presented, with topics ranging from antiangiogenesis to biomarkers, to epigenomics, to molecular targets, and to prevention and survivorship, terms not heard in cancer research in 1907.
The AACR is proud of the fact that our members have been responsible for so many scientific advances. Our meetings, conferences, task forces, and journals have provided, and continue to provide, the major forums for reporting, discussing, and disseminating cancer research, and AACR is playing an increasingly important role in research funding.
As part of our dedication to preserving the record of cancer research, and to celebrate our 100th Anniversary, the AACR has commissioned a series of historical review articles to be published serially in our flagship journal, Cancer Research. This history series is intended to cover the major scientific advances of the past 100 years in the fields of cancer causation, pathogenesis, prevention, and treatment. The articles are written by experts in the respective fields who are themselves responsible for some of the advances they will describe. The goal is not to produce a history of the AACR; this has been published elsewhere ( 1, 2, 5, 6 ). Rather, the group of articles will form a unique chronicle of progress, the factors that influenced the developments, their implications, and future directions in the field.
This issue of Cancer Research contains the first article in this series: “Advances in Chemical Carcinogenesis,” by Loeb and Harris. It highlights the evidence that chemical agents play a major role in human cancer causation and the remarkable insights into the underlying mechanisms that have been obtained. The exciting advances in this field also have profound implications in terms of both cancer prevention and treatment.
Subsequent articles related to cancer causation will cover cancer epidemiology, tumor virology, and cancer genetics. Other articles will cover pathogenesis, treatment, and prevention. We thank the authors of these articles for their efforts and insights. We trust that readers of Cancer Research will find the articles not only of interest but also an inspiring record of scientific achievement.
Given how far our understanding of cancer at the clinical, tissue, cellular, and molecular levels has come in the past 100 years, it is not overly optimistic to think that well before the next AACR Centennial, the world will be celebrating a major reduction in cancer incidence and mortality. Exciting progress toward that goal is being made every day in our research laboratories and clinics.
Citing articles via
Email alerts.
- Online First
- Collections
- Online ISSN 1538-7445
- Print ISSN 0008-5472
AACR Journals
- Blood Cancer Discovery
- Cancer Discovery
- Cancer Epidemiology, Biomarkers & Prevention
- Cancer Immunology Research
- Cancer Prevention Research
- Cancer Research
- Cancer Research Communications
- Clinical Cancer Research
- Molecular Cancer Research
- Molecular Cancer Therapeutics
- Info for Advertisers
- Information for Institutions/Librarians
- Privacy Policy
- Copyright © 2023 by the American Association for Cancer Research.
This Feature Is Available To Subscribers Only
Sign In or Create an Account

- The Cancer History Project

Weeks before death from sarcoma, Norm Coleman reflects on career in radiation oncology, addressing health disparities
- By Cancer History Project
- March 22, 2024

Before her legendary career at NIH, Vivian Pinn was the second Black woman to graduate from UVA med school

Roderic Pettigrew, founding director of NIBIB, reflects on a career as a “physicianeer”—merging medicine, engineering

The boy who cried vape: Philip Morris International calls for a smoke-free world
- By The Center for the Study of Tobacco and Society

Excerpt of “Blowing Smoke: The Lost Legacy of the Surgeon General’s Report on Smoking and Health”
Video: The history of SEER registries
Video: 50 years of SEER

- Institutions
MSK’s Sloan Kettering Institute Celebrates 75 Years of Discovery
At DCI 50th Celebration, the Sounds of Hope (April 14, 2022)
Milestones in Gynecologic Oncology at Duke

ASCO Remembers Chemotherapy Pioneer and Karnofsky Award Recipient Dr. Irwin H. Krakoff
ASCO Remembers Former Board of Directors Member and Radiation Oncologist Dr. A. William Blackstock Jr.
The Distinguished Career of Michael B. Kastan

- Research Milestone
Duke BioRepository & Precision Pathology Center Commemorates 10 Years
The Study That Launched 50,000 Papers (and Counting)
2007 Genomics and Cancer Risk Roundtable

Former HHS Secretary Louis Sullivan recalls sinking RJR’s “Uptown,” a menthol brand for Black smokers

60 years after: Don Shopland, Alan Blum discuss the writing of the 1964 Surgeon General’s Report on Smoking and Health

How George Santos and Al Owens’s early Cytoxan studies led to standard-of-care therapy in BMT

Yale Cancer Answers: Richard Edelson on the development of anti-cancer vaccines
50th Anniversary of the Johns Hopkins Kimmel Cancer Center Podcast Series: Cancer Research

The goal of the Cancer History Project is twofold: to collect and preserve the history of cancer research, and to spark rigorous discussion of the achievements of the past half-century.
Created to mark the 50th anniversary of the National Cancer Act of 1971, the Cancer History Project is a free historical resource that places a vast, expertly curated collection of primary sources and authoritative interpretations within easy reach of researchers, medical professionals, students, policy-makers, and patients.
The Cancer History Project is a new way of preserving history: collaboratively curated by the institutions and people who shaped it.
Our Sponsors

- Primary Source
- Photo Archive
- The Cancer Letter Archive
- The Cancer Letter
- Editorial Board
- Contributors
- Terms of Service
- Privacy Policy
Cancer: A Historic Perspective
Since the earliest medical records were kept, cancer as a disease has been described in the history of medicine . The earliest known descriptions of cancer appear in seven papyri, discovered and deciphered late in the 19th century. They provided the first direct knowledge of Egyptian medical practice. Two of them, known as the "Edwin Smith" and "George Ebers" papyri, contain descriptions of cancer written around 1600 B.C., and are believed to date from sources as early as 2500 B.C. The Smith papyrus describes surgery , while the Ebers' papyrus outlines pharmacological, mechanical, and magical treatments.
Based on the information recorded on papyri and hieroglyphic inscriptions, ancient Egyptians were able to distinguish benign tumors from malignant tumors. They were also able to use different treatments, including surgery, and other various modes of medicine.
Following the decline of Egypt, the next chapters of medical and scientific history were written in Greece and Rome. The great doctors Hippocrates and Galen dominated medical thought for 1500 years. They lifted medicine out of the realms of magic, superstition, and religion. Hippocrates and Galen defined disease as a natural process , and based treatment on observation and experience. Cancers were identified, with warnings against treatment of the more severe forms. Hippocrates is credited with naming "cancer" as "karkinoma" ( carcinoma ) because a tumor looked like a "crab" ("karkinoma" is Greek for "crab") in that there is a central body to a tumor and the tumor extension appeared as the legs of the "crab".
After the fall of Rome, Constantinople became the intellectual storehouse of civilization. From there, in Arabic translations, classic Greek and Roman texts made their way back through Europe. The ancient teachings of Galen continued to inspire physicians in Constantinople, Cairo, Alexandria, Athens, and Antioch in a time when magic spells and myths dominated the West. Cancer continued to be explained as the result of an excess of black bile , curable only in its earliest stages.
In the modern world, science and surgery advanced as physicians returned to direct observation of the human body. However, the theory that cancer was caused by an excess of black bile continued to prevail in the 16th century. Cancer was considered incurable, although a wide variety of pastes containing arsenic were formulated to treat its manifestations. In the 17th century, the old theory of disease based on bodily humors was discarded when Gaspare Aselli discovered the vessels of the lymphatic system and suggested abnormalities of lymph as the primary cause of cancer.
Rejecting the 17th-century theory about the cause of cancer was the French physician Claude Gendron. He concluded that cancer arises locally as a hard, growing mass , untreatable with drugs, and must be removed with all its "filaments."
Two 18th-century French scientists, physician Jean Astruc and chemist Bernard Peyrilhe, conducted experiments to confirm or disprove hypotheses related to cancer. Their efforts, however absurd they seem in retrospect, established experimental oncology , the science of seeking better diagnosis , treatments and understanding of the causes of cancer. During this period, environmental cancers were reported, and hospitals specializing in cancer care were opened.
In the late 19th century, the development of better microscopes not only helped document and define disease-causing organisms, but also made possible the examination of cells and cellular activity. Study of cancer tissues and tumors revealed that cancercells were markedly different in appearance than normal cells of surrounding tissue or the cells from which they originated. Researchers began to focus on questions such as the origin of cells and the relationship of disease to the behavior of a cell . It was the invention of the microscope that revealed the cancer cell itself.
The early 20th century saw great strides made in understanding the structures, functions and chemistry of living organisms. Cancer research in cell culture , chemical carcinogens, diagnostic techniques and chemotherapy firmly established oncology as science. Researchers pursued different theories of the origin of cancer, subjecting their hypotheses to systematic experimentation. A viral cause of cancer in chickens was documented in 1911, and both chemical and physical carcinogens were conclusively identified. Chromosomal abnormalities were also investigated as possible causes of cancer.
In 1913, a need to combat rising public fear and ignorance concerning cancer led to two significant events: the publication of the first known article on cancer's warning signs in a popular woman's magazine, and formation of a nationwide organization dedicated to public education on cancer. Cancer, as a disease, was brought into the light of day.
In 1937, the U.S. Congress made the conquest of cancer a national goal with a unanimous vote to pass the National Cancer Institute Act. This Act created the National Cancer Institute, which was expected to break new theoretical ground by conducting its own research, promoting research in other institutions and coordinating cancer-related projects and activities. In 1971, President Richard M. Nixon signed the National Cancer Act, launching a National Cancer Program administered by the National Cancer Institute . Key events in the United States' national cancer policy legislative history, from 1937 to 1999 are available here .
Since its establishment, fundamental biomedical research supported by the National Cancer Institute has advanced the understanding of cancer. Using tools of molecular biology and molecular genetics , scientists are making great leaps in the discovery and mapping of links between chromosomes, the genes within, and cancer. In addition to traditional cancer therapies, potential solutions to the prevention and cure of cancer seem limited only by the imagination.
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
The nih almanac, national cancer institute (nci).
- Important Events
- Legislative Chronology
The National Cancer Institute (NCI) is the federal government's principal agency for cancer research and training. Established under the National Cancer Institute Act of 1937, NCI is part of the National Institutes of Health (NIH), one of 11 agencies that make up the Department of Health and Human Services (HHS).
NCI’s mission is to lead, conduct, and support cancer research across the nation to advance scientific knowledge and help all people live longer, healthier lives.
As the leader of the cancer research enterprise, collectively known as the National Cancer Program, and the largest funder of cancer research in the world, NCI manages a broad range of research, training, and information dissemination activities that reach across the entire country, meeting the needs of all demographics—rich and poor, urban and rural, and all racial/ethnic populations. Specifically, NCI focuses on two broad roles:
Cancer Research
- Leads the nation’s research efforts to improve cancer prevention, detection, diagnosis, and survivorship
- Supports 72 NCI-Designated Cancer Centers and more than 5,000 grantees
- Coordinates and supports all phases of clinical trials across 2,500 clinical trial sites nationwide, seeking the development of new and improved cancer treatments
- Supports intramural research scientists in our own laboratories and clinics
- Partners with industry, private philanthropic organizations, other federal agencies, and other national and foreign institutions to engage in cancer research and training opportunities that otherwise might not be possible because of their complexity and cost
- Collaborates with private-sector life sciences companies to advance promising innovative technologies that fuel improvements in detection, diagnosis, and treatment of cancer
- Supports the Frederick National Laboratory for Cancer Research, the only federally funded research and development center dedicated exclusively to biomedical research
- Maintains long-term storage of publicly available cancer genomic and clinical data
- Supports construction of laboratories, clinics, and related facilities for cancer research
Training and Support for Cancer Researchers
- Strives to attract, train, and retain the best minds to become the next generation of cancer researchers
- Provides support to scientists and their institutions to create outstanding environments for researchers to train, conduct basic and clinical research, and care for cancer patients
- Funds training and career development opportunities across a broad spectrum of cancer research disciplines through training grants, fellowships, research career development awards, and research education grants
- Supports targeted cancer research training for individuals from backgrounds underrepresented in the biomedical and behavioral sciences to achieve and sustain a diverse workforce
- Provides comprehensive training programs that support the needs of qualified individuals at all stages of their career development, ranging from middle-school students to independent researchers
- Offers training opportunities centered in hospitals and research institutions across the nation, in addition to intramural training programs offered at NCI laboratories and offices in Maryland
As a federal agency, NCI receives its funds from Congress. The bulk of our budget supports extramural grants and cooperative agreements to facilitate research conducted at universities, medical schools, hospitals, cancer centers, research laboratories, and private firms in the United States and abroad. These funds also support intramural research at NCI’s laboratories and offices in Bethesda, Rockville, and Frederick, MD.
Our investments have led to declines in the rates of new cancer cases and cancer deaths overall in the last few decades in the United States. In line with this improvement, the number of cancer survivors in the United States has more than doubled from 7 million in 1992 to more than 15 million in 2016—and is expected to rise to more than 26 million by 2040. These trends reflect advances in cancer detection, diagnosis, and patient care that have resulted in people living longer, healthier lives than ever before.
For additional information about NCI and recent cancer research findings, visit the NCI web site .
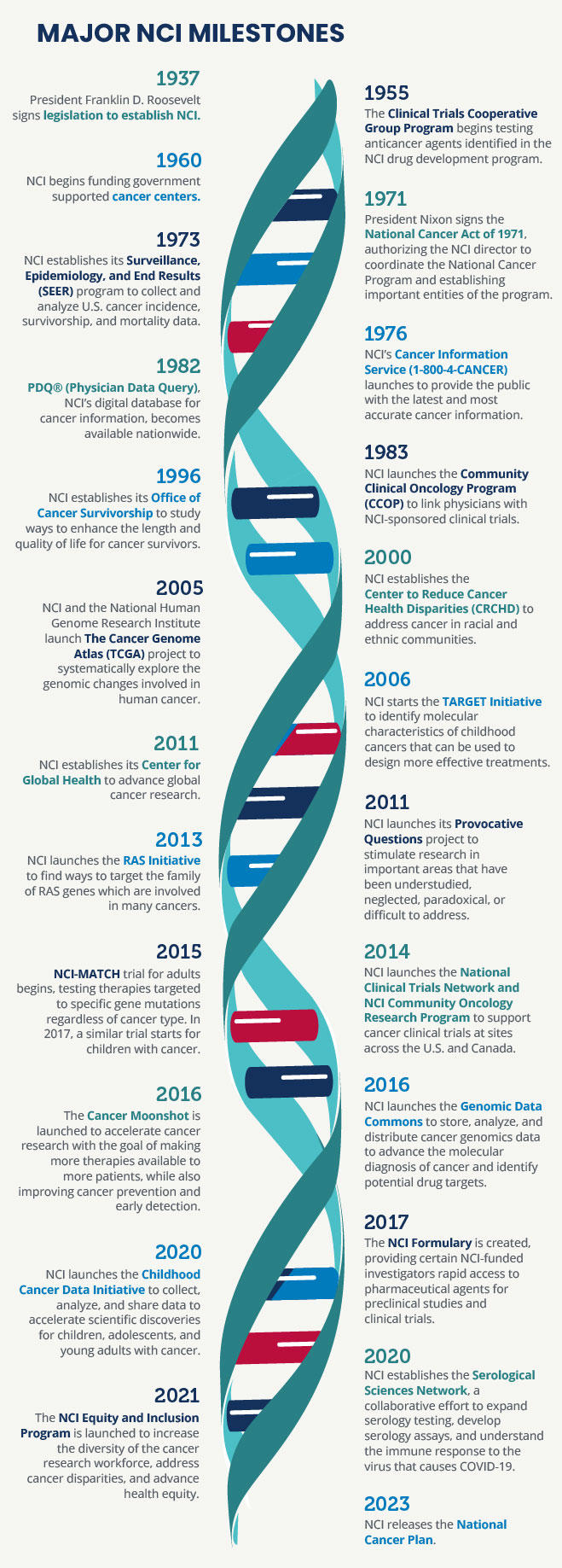
Important Events in NCI History
August 5, 1937 —The National Cancer Institute (NCI) was established through the National Cancer Act of 1937, signed into law by President Franklin D. Roosevelt. Its passage represented the culmination of nearly three decades of efforts to formalize the U.S. government’s place in cancer research. The act represents the first time that Congress provided funding to address a non-communicable disease. The act created NCI as an independent research institute within the Public Health Service. NCI became the federal government’s principal agency for conducting research and training on the cause, diagnosis, and treatment of cancer.
NCI was tasked with assisting and promoting cancer research at other public and private institutions, particularly by providing funding opportunities to support promising cancer research. The act established the National Advisory Cancer Council, now known as the National Cancer Advisory Board, which recommended approval of first award for fellowships in cancer research shortly thereafter.
August 1940 —The first issue of the Journal of the National Cancer Institute was published.
July 1, 1946 —The cancer control program was established, providing grants to the states for support of cancer control activities.
July 2, 1953 —NCI inaugurated a full-scale clinical research program in the new Clinical Center.
1955 —NCI established the Clinical Trials Cooperative Group Program which included several research networks, called cooperative groups, that conduct cancer clinical research primarily under the sponsorship of NCI.
1957 —The first malignancy (choriocarcinoma) was cured with chemotherapy at NCI.
January 12, 1961 —The Laboratory of Viral Oncology was established to investigate the relationship of viruses to human cancer.
April 2, 1962 —An exhibit, "Man Against Cancer," opened in Washington, D.C., to commemorate the Institute's 25th anniversary and inaugurate Cancer Progress Year.
October 25, 1962 —The Human Cancer Virus Task Force held its first meeting. The task force, comprised of scientists from NCI and other institutions, stimulated the development of special programs in viral oncology.
February 13, 1967 —NCI, in collaboration with the U.S. Public Health Service Hospital, established the Baltimore Cancer Research Center to conduct basic and clinical research for cancer treatment and offer training to medical students and scientists.
October 18, 1971 —President Nixon converted the Army's former biological warfare facilities at Fort Detrick, Maryland, to house research activities on the causes, treatment, and prevention of cancer.
December 23, 1971 —President Nixon signed the National Cancer Act of 1971. The act represented the U.S. commitment to what President Nixon described as the “war on cancer,” which, by 1970, had become the nation’s second leading cause of death. The act granted authority to the Director of NCI to plan and develop a National Cancer Program that included NCI, other research institutes, and other federal and non-federal programs. It established the procedure for submitting NCI’s annual budget, called the “bypass budget,” which is transmitted directly from the NCI director to the President and Congress. The act also required the creation of a new National Cancer Advisory Board, a presidentially appointed committee of 18 members, to assist NCI in developing its programs. It also established the President’s Cancer Panel, a three-member panel that submits an annual report to the President and holds periodic public hearings. Finally, the act provided additional funding for NCI to establish 15 new cancer research centers, local cancer control programs, and an international cancer research data bank.
July 27, 1972 —A Bureau-level organization was established for NCI, giving the Institute and its components organizational status commensurate with the responsibilities bestowed on it by the National Cancer Act of 1971.
June 20, 1973 —NCI director Dr. Frank J. Rauscher, Jr., announced that eight institutions were recognized as Comprehensive Cancer Centers to bring results of research as rapidly as possible to a maximum number of people. (In 2017, there are 69 NCI designated cancer centers.)
September 12, 1974 —NCI made its first cancer control awards to state health departments for a three-year program to screen low-income women for cancer of the uterine cervix. At its peak in 1978, the program had grown to a total of 32 states and territories.
December 17, 1974 —NCI and the National Library of Medicine established CANCERLINE, a jointly developed computerized service to provide scientists across the country with information on cancer research projects and published findings.
December 19, 1974 —The Clinical Cancer Education Program was announced to develop more innovative teaching methods in cancer prevention, diagnosis, treatment, and rehabilitation in schools of medicine, dentistry, osteopathy, and public health; affiliated teaching hospitals; and specialized cancer institutions.
1975 —The Frederick National Laboratory for Cancer Research was established as the Frederick Cancer Research and Development Center in 1972 when about 70 acres and 67 buildings of the U.S. Army were transferred to the U.S. Department of Health and Human Services (HHS), which includes the National Institutes of Health (NIH). Since then, Frederick National Lab has become an internationally recognized center of scientific excellence in cancer and AIDS research and development.
Shortly thereafter, The National Science Foundation notified HHS that NCI-Frederick met the criteria for and was designated as a Federally Funded Research and Development Center (FFRDC), a government-owned, contractor-operated facility designed to achieve long-term research and development needs that could not be met as effectively by existing in-house or contractor resources.
1975 —The Cooperative Minority Biomedical Program, as approved by the National Cancer Advisory Board, represented a co-funding effort by NCI to implement and foster cancer research through NIH's Division of Research Resources' Minority Biomedical Research Support Program and the National Institute of General Medical Sciences Minority Access to Research Careers Program.
July 1, 1975 —The Cancer Information Service was established following a mandate of the National Cancer Act of 1971, which gave NCI new responsibilities for educating the public, patients, and health professionals.
August 5, 1977 —NCI celebrated its 40th anniversary with a ceremony on the NIH campus. Senator Warren G. Magnuson of Washington who, as a member of the House of Representatives, introduced a bill to establish NCI in 1937, sent a message stating: "Those one and a half million Americans who are alive today—cured of cancer—are ample justification for all that we've appropriated over the last 40 years."
1979 —The first human RNA virus (HTLV-I) was discovered by NCI's Dr. Robert C. Gallo, leading to his role in the discovery of the human immunodeficiency virus (HIV) as the infectious agent responsible for acquired immune deficiency syndrome (AIDS) and in the development of the HIV blood test. He has been a major contributor to subsequent HIV research.
July 18, 1979 —NCI and the National Naval Medical Center, Bethesda, Md., signed an agreement to cooperate in a cancer treatment research program.
April 27, 1981 —A new Biological Response Modifiers Program was established in the Division of Cancer Treatment to investigate, develop and bring to clinical trial potential therapeutic agents that may alter biological responses that are important in cancer growth and metastasis.
September 1982 —PDQ (or Physician Data Query), a computerized database on cancer treatment information, became available nationwide through the National Library of Medicine's MEDLARS system.
December 16, 1982 —NCI purchased a building adjacent to the NIH campus in Bethesda, Maryland, through generous donations to the NCI Gift Fund. This building housed the Journal of the National Cancer Institute, the Scientific Information Branch (which publishes Cancer Treatment Reports and Cancer Treatment Symposia ), the International Cancer Research Data Bank, and PDQ (Physician Data Query, NCI's comprehensive source of cancer information).
July 16, 1983 —NCI launched the Community Clinical Oncology Program (CCOP) to establish a cancer control effort that combines the expertise of community oncologists with NCI clinical research programs. The CCOP initiative is designed to bring the advantages of clinical research to cancer patients in their own communities.
1984 —A policy statement regarding the relationship of NCI, the pharmaceutical industry, and NCI-supported cooperative groups was developed. The statement conveys the need for collaboration between NCI and the pharmaceutical industry in pursuing the joint development of anticancer drugs of mutual interest.
March 6, 1984 —HHS Secretary Margaret M. Heckler launched a new Cancer Prevention Awareness Program aimed at saving 95,000 lives per year by the year 2000. The program, guided by NCI, will inform the public about cancer risks and steps individuals can take to reduce risk.
April 1984 —NCI scientist Dr. Robert C. Gallo reported the isolation of a new group of viruses found in the helper T-cells of patients with AIDS or pre-AIDS symptoms, as well as from healthy individuals at high risk for developing AIDS. These viruses were ultimately named human immunodeficiency virus or HIV. This discovery made the control of blood-product-transmitted AIDS feasible by enabling the development of a simple test for the detection of AIDS-infected blood by blood banks and diagnostic laboratories.
August 1985 — The Cancer Prevention Fellowship Program (CPFP), one of the first formal postdoctoral research training programs in cancer prevention, began. CPFP provides state-of-the-art training in cancer prevention and control through mentored research at NCI, guiding each fellow to develop an independent research program in cancer prevention.
October 24, 1987 —The Office of Technology Development was established in the Office of the Director to guide implementation of legislation, rules and regulations, and activities relating to collaborative agreements, inventions, patents, royalties, and associated matters.
September 30, 1988 —The first Consortium Cancer Center was established, comprised of three historically black medical schools. Component universities supported by this core grant—Charles R. Drew University of Medicine and Science in Los Angeles, Meharry Medical College in Nashville, and Morehouse School of Medicine in Atlanta—focused their efforts on cancer prevention, control, epidemiology, and clinical trials.
April 1989 —NCI increased efforts to supplement research grants to encourage recruitment of minority scientists and science students into extramural research laboratories. This initiative is expanded to include scientists and science students who are women or individuals with disabilities.
May 22, 1989 —NCI scientist Dr. Steven A. Rosenberg conducted the first human gene transfer trial using human tumor-infiltrating lymphocytes to which a foreign gene had been added.
December 20, 1989— NCI researchers published the Breast Cancer Risk Assessment Model, a tool to estimate a woman's risk of developing invasive breast cancer, based on data from case-control studies and breast cancer incidence rates in the US. Over the years, the tool has been updated and expanded to cover African Americans and other groups; it is widely used by clinicians and researchers. Originally available on a floppy disk, the tool was later renamed and made available online as the Breast Cancer Risk Assessment Tool. The US Food and Drug Administration guidelines for use of tamoxifen and raloxifene for breast cancer risk reduction rely on estimates generated by the tool. It is also used for patient counseling and for assessing possible public health prevention strategies.
September 14, 1990 —Scientists from NCI and National Heart, Lung, and Blood Institute announced the first trial in which a copy of a faulty gene was inserted into white blood cells to reverse the immune deficiency it caused. The trial was initiated to treat adenosine deaminase deficiency. This was the first human gene therapy trial used to treat immunodeficiency.
January 29, 1991 —Patients with melanoma were treated with tumor-infiltrating lymphocytes to which a gene for tumor necrosis factor had been added. This was the first human gene therapy trial used to treat cancer.
October 1991 —NCI began the 5 A Day program, in partnership with the nonprofit group Produce for Better Health, to encourage Americans to eat at least five fruits and vegetables a day.
1992 —NCI established the Specialized Programs of Research Excellence (SPORE). The NCI Translational Research Program (TRP) is the home of SPORE and a cornerstone of NCI’s efforts to promote collaborative, interdisciplinary translational cancer research. SPORE grants involve both basic and clinical/applied science, and support projects that will result in new and diverse approaches to the prevention, early detection, diagnosis, and treatment of human cancers.
December 18, 1992 —Taxol (paclitaxel), an anticancer drug extracted from the bark of the Pacific yew, received approval by the U.S. Food and Drug Administration (FDA) for the treatment of ovarian cancer that was not responsive to other therapy. NCI spearheaded the development of the drug through collaboration with the USDA's Forest Service, the Department of the Interior's Bureau of Land Management, and Bristol-Myers Squibb Company. This collaboration was made possible by the Federal Technology Transfer Act of 1986.
November 1993 —The Prostate, Lung, Colorectal, and Ovarian trial, designed to determine whether certain screening tests will reduce the number of deaths from these cancers, began recruiting 148,000 men and women, ages 55–74.
November 1996 —Cancer mortality rates declined nearly 3% between 1991 and 1995. This was the first sustained decline since national recordkeeping was instituted in the 1930s.
1996 —The NCI Office of Liaison Activities was established to ensure that cancer research advocates have input concerning NCI research and related activities. The office, now called the Office of Advocacy Relations, supports NCI's research and programs by fostering strong communications and partnerships with the cancer advocacy community and professional societies.
August 1, 1997 —NCI, in partnership with government, academic, and industrial laboratories, launched the Cancer Genome Anatomy Project to enhance discovery of the acquired and inherited molecular changes in cancer and to evaluate the clinical potential of these discoveries. The project included a website allowing scientists to rapidly access data generated through the project and apply it to their studies.
April 6, 1998 —Results of the Breast Cancer Prevention Trial, testing the effectiveness of tamoxifen to prevent the disease, were announced 14 months earlier than expected. Women taking tamoxifen had 45% fewer breast cancer diagnoses than women on the placebo, proving that breast cancer can potentially be prevented.
September 25, 1998 —The FDA approved the monoclonal antibody Herceptin (Trastuzumab) for the treatment of metastatic breast cancer in patients with tumors that produce excess amounts of a protein called HER-2. Approximately 30% of breast cancer tumors produce excess amounts of HER-2.
May 25, 1999 —The Study of Tamoxifen and Raloxifene (STAR) one of the largest breast cancer prevention studies ever, began recruiting volunteers at more than 400 centers across the United States, Puerto Rico, and Canada. The trial will include 22,000 postmenopausal women at increased risk of breast cancer to determine whether the osteoporosis prevention drug raloxifene (Evista) is as effective in reducing the chance of developing breast cancer as tamoxifen (Nolvadex) has proven to be.
October 6, 1999 —NCI awarded nearly $8 million in grants toward the creation of the Early Detection Research Network, a network to discover and develop new biological tests for the early detection of cancer and of biomarkers for increased cancer risk.
December 8, 1999 —NCI published the Atlas of Cancer Mortality, 1950–94 , showing the geographic patterns of cancer death rates in over 3,000 counties across the country over more than 4 decades.
April 6, 2000 —A $60 million program was announced to address the unequal burden of cancer within certain populations in the United States over the next 5 years. The Special Populations Networks for Cancer Awareness Research and Training is intended to build relationships between large research institutions and community-based programs. Eighteen grants at 17 institutions are expected to create or implement cancer control, prevention, research, and training programs in minority and underserved populations.
June 7, 2000 —President Clinton issued an executive memorandum directing the Medicare program to reimburse providers for the cost of routine patient care in clinical trials. The memorandum also provides for additional actions to promote the participation of Medicare beneficiaries in clinical studies.
December 3, 2000 —As part of a national commitment to identify and address the underlying causes of disease and disability in racial and ethnic communities, NCI established the Center to Reduce Cancer Health Disparities. Because these communities carry an unequal burden of cancer-related health disparities, NCI is working to enhance its research, education, and training programs that focus on populations in need.
May 10, 2001 —FDA approval of the drug Gleevec, also known as STI571, is announced as an oral treatment for chronic myelogenous leukemia. This marked the approval of the first molecularly targeted drug that directly turns off the signal of a protein known to cause a cancer. Clinical trials expanded as investigators tested Gleevec in a variety of cancers that share common molecular abnormalities.
July 24, 2001 —The largest-ever prostate cancer prevention study was launched by NCI and a network of researchers known as the Southwest Oncology Group. The Selenium and Vitamin E Cancer Prevention Trial is designed to determine if these two dietary supplements can protect against prostate cancer which is the most common form of non-skin cancer in men. The study is expected to include a total of 32,400 men.
September 4, 2001 —NCI and the American College of Radiology Imaging Network launched 3-year multicenter study of digital mammography, called the Digital Mammographic Imaging Screening Trial, the first large, multicenter study to compare digital mammography to standard mammography for the detection of breast cancer.
September 10, 2001 —NCI launched the Consumer Advocates in Research and Related Activities program—a landmark initiative convening a network of 200 dedicated advocates who bring the viewpoint of those affected by cancer to NCI.
February 7, 2002 —Scientists from NCI and FDA reported that patterns of proteins found in patients' blood may reflect the presence of ovarian cancer, even at early stages. Currently, more than 80% of ovarian cancer patients are diagnosed at a late clinical stage and have a 20% or less chance of survival at five years. This new diagnostic concept is potentially applicable to the diagnosis of other diseases.
May 19, 2002 —Researchers from NCI reported that the molecularly targeted drug bevacizumab slowed tumor growth in patients with metastatic renal cell carcinoma, the most common form of kidney cancer in adults.
June 19, 2002 —NCI scientists used microarray technology to determine the patterns of genes that are active in tumor cells from which they could predict whether patients with the most common form of non-Hodgkin lymphoma in adults are likely to be cured by chemotherapy.
July 16, 2002 —The National Heart, Lung, and Blood Institute (NHLBI) of NIH stopped a major clinical trial early of the risks and benefits of combined estrogen and progestin in healthy menopausal women due to an increased risk of invasive breast cancer. The large multi-center trial, a component of the Women's Health Initiative (WHI), also found increases in coronary heart disease, stroke, and pulmonary embolism in study participants on estrogen plus progestin compared to women taking placebo pills. The trial showed that postmenopausal women who used estrogen replacement therapy for 10 or more years were at significantly higher risk of developing ovarian cancer than women who never used hormone replacement therapy.
September 18, 2002 —NCI launched the National Lung Screening Trial to compare spiral computed tomography and single-view chest x-ray for early lung cancer in 50,000 current and former heavy smokers. The trial will examine the relative risks and benefits of both tests at 30 study sites throughout the United States.
September 19, 2002 —NCI researchers demonstrated that a new approach to cancer treatment, that replaces a patient's immune system with cancer-fighting cells produced in the laboratory specifically to destroy their tumors, can lead to tumor shrinkage. The experimental technique, known as adoptive transfer, has shown promising results in patients with metastatic melanoma who have not responded to standard treatment.
October 16, 2002 —NCI and FDA scientists found that patterns of proteins in patients' blood, called prostate-specific antigen (PSA), may help distinguish between prostate cancer and benign prostate conditions. PSA is a protein produced by cells of the prostate gland. The blood level of PSA is often elevated in men with prostate cancer. The technique may be useful in deciding whether to perform a biopsy in men with elevated levels of PSA.
October 31, 2002 —NCI researchers have discovered that a molecule best known for its antimicrobial properties also can activate key cells in the immune response. This newly discovered function suggests the molecule, a peptide called Beta-defensin 2, may be useful in the development of more effective cancer vaccines.
2003 —A novel approach to treatment of solid cancers involves therapeutic agents that inhibit the generation of new blood vessels in growing tumors (angiogenesis).
March 5, 2003 —Taking daily aspirin for as little as three years was shown to reduce the development of colorectal polyps by 19% to 35% in people at high risk for colorectal cancer in two randomized, controlled NCI clinical trials published in the New England Journal of Medicine .
May 30, 2003 —Overseen by an Interagency Oncology Task Force (IOTF), FDA and NCI entered into an agreement to share knowledge and resources to facilitate the development of new cancer drugs and speed their delivery to patients. The goal of the IOTF is to leverage the expertise and capabilities of both agencies to streamline and accelerate the overall development of diagnostic, preventive, and therapeutic interventions for cancer.
June 24, 2003 —Results of the Prostate Cancer Prevention Trial, testing the effectiveness of finasteride to prevent the disease, were announced about a year earlier than expected. Men taking finasteride had 25% fewer prostate cancer diagnoses than men on the placebo. There was a note of caution, however; the men who did develop prostate cancer while taking finasteride were more likely to have high-grade tumors.
September 2, 2003 —Death rates from the four most common cancers—lung, breast, prostate, and colorectal—continued to decline in the late 1990s according to data from the Annual Report to the Nation on the Status of Cancer, 1975-2000. This report provides an annual update of cancer incidence, mortality, and trends in the United States. NCI has partnered with The Centers for Disease Control and Prevention, the American Cancer Society, and the North American Association of Central Cancer Registries on the report since 1998.
November 6, 2003 —NCI scientists demonstrated that the growth factors interleukin-2 (IL-2) and IL-15 have contrasting roles in the life and death of lymphocytes, an observation that has implications for the immunotherapy of cancer and autoimmune diseases.
September 13, 2004 —NCI announced the Alliance for Nanotechnology in Cancer, a five-year initiative to integrate nanotechnology development into basic and applied cancer research to facilitate the rapid application of this science to the clinic. Nanotechnology is a field of research that deals with the engineering and creation of things from materials that are less than 100 nanometers (one-billionth of a meter) in size, especially single atoms or molecules. Nanotechnology offers the means to target treatments directly and selectively to cancerous cells and neoplasms.
December 10, 2004 —According to research supported by NCI, and performed in collaboration with the National Surgical Adjuvant Breast and Bowel Project and Genomic Health Inc., a new molecular test can predict the risk of breast cancer recurrence and may identify women who will benefit most from chemotherapy.
February 16, 2005 —In preparation for the new generation of molecular-based oncology medical products and as an initiative of NCI’s and FDA's Interagency Oncology Task Force, the agencies jointly established an NCI-FDA Research and Regulatory Review Fellowship program, designed to train researchers to bridge the processes from scientific discovery through clinical development and regulatory review of new oncology products.
April 25, 2005 —The Herceptin Adjuvant (HERA) (Breast International Group [BIG] 01-01) Trial showed the combination of the targeted agent trastuzumab (Herceptin) and standard chemotherapy cuts the risk of HER-2-positive breast cancer recurrence by more than half compared with chemotherapy alone. For women with this type of aggressive breast cancer, the addition of trastuzumab to chemotherapy appears to virtually reverse prognosis from unfavorable to good.
May 6, 2005 —NCI announced the Community Networks Program, a five-year initiative to reduce cancer disparities in minority and underserved populations through community participation in education, research, and training.
September 16, 2005 —Preliminary results from a large clinical trial of digital versus film mammography showed no difference in detecting breast cancer for the general population of women in the trial. However, those women with dense breasts, who are pre- or perimenopausal or who are younger than age 50, may benefit from having a digital rather than a film mammogram.
September 28, 2005 —NCI and the National Institute of Neurological Disorders and Stroke (NINDS) created Rembrandt (Repository for Molecular Brain Neoplasia Data), a joint informatics initiative to molecularly characterize a large number of primary brain tumors and to correlate those data with extensive retrospective and prospective clinical data.
October 2005 —NCI initiated the Patient Navigator Research Program (PNRP) to assess the impact of patient navigators on providing timely and quality standard cancer care to patients following an abnormal cancer finding. The PNRP was designed to encourage research collaborations and partnerships with organizations serving diverse underserved communities within cancer care delivery systems.
October 5, 2005 —The Annual Report to the Nation on the Status of Cancer , 1975-2002, showed observed cancer death rates from all cancers combined dropped 1.1% per year from 1993 to 2002. The report's authors attribute the declines in death rates to progress in prevention, early detection, and treatment.
October 11, 2005 —NCI announced the Transdisciplinary Research on Energetics and Cancer initiative to study the effects of diet, weight, and physical activity on cancer and to answer critical questions to help guide our nation's public health efforts.
November 7, 2005 —NCI launched a cancer biorepository pilot project designed to standardize biospecimen collection and management among investigators of Specialized Programs of Research Excellence for prostate cancer to enhance the quality and availability of various biospecimens and associated data for the broader scientific community.
December 7, 2005 —Results from several studies presented at the San Antonio Breast Cancer Symposium validated that a test called Oncotype DX can predict the risk of breast cancer recurrence in a sizable group of patients. The studies also appeared to identify which of those patients might benefit most from chemotherapy. The studies were heralded by researchers as an important moment in the move toward individualized cancer care.
December 13, 2005 —NCI and the National Human Genome Research Institute launched a comprehensive effort to accelerate an understanding of the molecular basis of cancer through the application of genome analysis technologies, especially large-scale genome sequencing. The overall effort, called The Cancer Genome Atlas, began with a pilot project to determine the feasibility of a full-scale effort to systematically explore the universe of genomic changes involved in all types of human cancer.
April 17, 2006 —Initial results of the Study of Tamoxifen and Raloxifene showed that the drug raloxifene, used to prevent and treat osteoporosis in postmenopausal women, works as well as tamoxifen in reducing breast cancer risk for postmenopausal women at increased risk of the disease.
May 23, 2006 —The Trial Assigning Individualized Options for Treatment (Rx) or TAILORx was launched to examine whether genes that are frequently associated with risk of recurrence for women with early-stage breast cancer can be used to assign patients to the most appropriate and effective treatment.
June 7, 2006 —Gene profiling, a molecular technique that examines many genes simultaneously, was shown to accurately distinguish between two types of immune cell tumors, Burkitt's lymphoma and diffuse large B-cell lymphoma (DLBCL). Burkitt's lymphoma and DLBCL appear similar when viewed under a microscope but correct diagnosis is critical because each requires very different treatments.
June 8, 2006 —NCI announced FDA approval of the human papillomavirus (HPV) vaccine, based on the research of NCI scientists Douglas Lowy, M.D., and John Schiller, Ph.D. Nearly two decades before, researchers at NCI and other institutions began searching for the underlying causes of cervical cancer. That scientific quest led to the vaccine Gardasil (human papillomavirus [HPV] vaccine, quadrivalent), which protects against infection from the two types of human papillomavirus that cause the majority of cervical cancers worldwide.
June 29, 2006 —Researchers at NCI identified a link between inherited and acquired genetic factors that dramatically increase the chance of developing a very common type of melanoma.
August 1, 2006 —NCI researchers published a model for estimating an individual’s 5-year risk of melanoma, based on visual inspection of the patient’s back as well as risk factors identified in a large U.S. case-control study, and incidence rates for melanoma in the U.S. population. The Melanoma Risk Assessment Tool can be used by health professionals to identify individuals at increased risk of melanoma, help them plan for regular screening, and potential
October 5, 2006 —The Biomarkers Consortium, a public-private biomedical research partnership composed of The Foundation for the National Institutes of Health, NIH, FDA, and the Pharmaceutical Research and Manufacturers of America, formed to search for and validate new biomarkers to accelerate the delivery of new technologies, medicines, and therapies for prevention, early detection, diagnosis, and treatment of disease.
October 18, 2006 —NCI released new data from the Cancer Genetic Markers of Susceptibility (CGEMS) study on prostate cancer intended to help identify genetic factors that influence the disease and could be integral to the discovery and development of new, targeted therapies. This was the first public release of a whole-genome association study of cancer—such studies examine the entire genome, with no assumptions about which genetic alterations cause cancer.
March 28, 2007 —Magnetic Resonance Imaging (MRI) scans of women who were diagnosed with cancer in one breast detected over 90% of cancers in the other breast that were missed by mammography and clinical breast exam at initial diagnosis, according to an American College of Radiology Imaging Network study supported by NCI. Adding an MRI scan to the diagnostic evaluation effectively doubled the number of cancers immediately found in these women.
April 1, 2007 —NCI and Cancer Genetic Markers of Susceptibility researchers reported that a variation in a portion of DNA strongly predicts prostate cancer risk and that this common variation may be responsible for up to 20% of prostate cancer cases in white men in the United States.
April 18, 2007 —A report using data from NCI’s Surveillance, Epidemiology and End Results (SEER) program showed that a sharp decline in the rate of new breast cancer cases in 2003 may be related to a national decline in the use of hormone replacement therapy (HRT). Age-adjusted breast cancer incidence rates in women in the United States fell 6.7% from 2002 to 2003. Prescriptions for HRT also declined rapidly in 2002 and 2003.
May 8, 2007 —Researchers from NCI and Baylor College of Medicine found that people infected with the hepatitis C virus are at an increased risk of developing certain lymphomas (cancers of the lymphatic system).
June 14, 2007 —NCI launched the three-year pilot phase of a new program that will help bring state-of-the-art cancer care to patients in community hospitals across the United States. The NCI Community Cancer Centers Program was designed to encourage collaboration between private-practice medical, surgical and radiation oncologists and NCI’s network of 63 NCI-designated Cancer Centers principally based at large research universities.
October 15, 2007 — The Annual Report to the Nation on the Status of Cancer , 1975-2004, showed cancer death rates decreased on average 2.1% per year from 2002 through 2004, nearly twice the annual decrease of 1.1% per year from 1993 through 2002.
November 1, 2007 —NCI sponsored a symposium, HIV/AIDS Research at the National Cancer Institute: A Record of Sustained Excellence, to celebrate the achievements in HIV/AIDS research by former and current NCI scientists, and announce future plans for continuing efforts to combat HIV infection, the devastating consequences of AIDS, and AIDS-related cancers.
November 27, 2007 —A new model for calculating invasive breast cancer risk (the CARE model) was found to give better estimates of the number of breast cancers that would develop in African American women 50 to 79 years of age than an earlier model which was based primarily on data from white women.
January 2008 —Scientists reported that results of a randomized phase III clinical trial show that a combination of low oral doses of difluoromethylornithine and sulindac greatly reduces the recurrence of colon polyps and is safe and well tolerated.
March 6, 2008 —DNA mutations found in a type of non-Hodgkin lymphoma that has a poor prognosis led researchers to a better understanding of how the cancer develops and how it might be treated.
April 21, 2008 —Researchers identified a pattern of gene activity in mice that may help to predict individual risk for breast cancer metastasis and survival in humans. A single gene called bromodomain 4 (Brd4) regulates the expression of this pattern, also called a signature. Researchers found that one result of this Brd4 regulation is the suppression of tumor growth and metastasis in a mouse model of cancer.
June 23, 2008 —NCI researchers found that cells from a blood-borne cancer called multiple myeloma rely on the activity of a single protein, IRF4, for the activation of a wide range of genes responsible for cell survival and spread. Blocking the production of this protein can be strikingly effective in eliminating cancer cells in laboratory models of multiple myeloma.
January 1, 2009 —Scientists identified mutations in a gene that predict a high likelihood of relapse in children with acute lymphoblastic leukemia (ALL). Although further research is needed, the findings are likely to provide the basis for future diagnostic tests to assess the risk of treatment failure. By using a molecular test to identify this genetic marker in ALL patients, physicians should be better able to determine appropriate therapies.
February 11, 2009 —Researchers established that abnormal white blood cells can be present in patients' blood more than six years prior to the diagnosis of a chronic form of lymphocytic leukemia. This finding may lead to a better understanding of the cellular changes that characterize the earliest stages of the disease and how it progresses.
March 18, 2009 —A new report from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial, designed to provide answers about the effectiveness of prostate cancer screening, showed that six annual screenings for prostate cancer led to more diagnoses of the disease, but no fewer prostate cancer deaths.
August 14, 2009 —Results of a randomized phase III clinical trial show that targeted therapy with the drug imatinib mesylate (Gleevec) reduces disease recurrence following surgery to remove a localized gastrointestinal stromal tumor.
October 5, 2009 —Researchers identified a gene that may play a role in the growth and spread of a childhood cancer called rhabdomyosarcoma, which develops in the body's soft tissues. The finding revealed a potential new target for the treatment of this disease.
October 7, 2009 —Researchers found that a small RNA molecule, known as a microRNA, may help physicians identify liver cancer patients who, in spite of their poor prognosis, could respond well to treatment with a biological agent called interferon.
December 18, 2009 —Initial results from a large, randomized clinical trial for patients with multiple myeloma, a cancer of the blood and bone marrow, showed that patients who received the oral drug lenalidomide (Revlimid, also known as CC-5013) following a blood stem cell transplant avoided recurrences longer than patients who received a placebo.
January 6, 2010 —Researchers with a study conducted at NCI, the National Institute for Allergy and Infectious Diseases, and the National Human Genome Research Institute, discovered genetic mutations that may contribute to the development of an aggressive form of non-Hodgkin lymphoma. These findings provided insight into a mechanism that cancer cells may use to survive, thus identifying potential new targets for treatment of the disease.
January 19, 2010 —Researchers found that the most common form of malignant brain cancer in adults, glioblastoma multiforme, is not a single disease but appears to be four distinct molecular subtypes that respond to aggressive chemotherapy and radiation differently, according to a study by The Cancer Genome Atlas Research Network.
April 19, 2010 —Long-term results show that Raloxifene, a common osteoporosis drug, prevented breast cancer to the same degree, but with fewer serious side-effects than the drug Tamoxifen that had been in use many years for breast cancer prevention as well as treatment. Raloxifene retained 76% of the effectiveness of Tamoxifen in preventing invasive disease and grew closer to Tamoxifen in preventing noninvasive disease. In particular, there was significantly less endometrial cancer with raloxifene use.
November 4, 2010 —The National Lung Screening Trial, a randomized national trial involving more than 53,000 current and former heavy smokers ages 55 to 74, compared the effects of two screening procedures for lung cancer—low-dose helical computed tomography (CT) and standard chest X-ray—on lung cancer mortality and found 20% fewer lung cancer deaths among trial participants screened with low-dose helical CT.
November 10, 2010 —Researchers discovered mutations in a particular gene that affects the treatment prognosis for some patients with acute myeloid leukemia, an aggressive blood cancer that kills 9,000 Americans annually.
December 23, 2010 —NCI announced major changes to the long-established Clinical Trials Cooperative Group Program that conducts many of the nationwide trials of new cancer therapies. In a major transformation, NCI intends to consolidate the nine groups that currently conduct trials in adult cancer patients into four state-of-the-art entities that will design and perform improved trials of cancer therapies. The changes are designed to provide greater benefits for cancer patients and more information for researchers. These moves come in response to an NCI-requested April 2010 report from the Institute of Medicine, which called for a series of changes to the cooperative groups program, including restructuring. The NCI Cooperative Group program, founded over 50 years ago, involves more than 3,100 institutions and 14,000 investigators, and the program enrolls over 25,000 patients in clinical trials each year.
March 10, 2011 —The number of cancer survivors in the United States increased to 11.7 million in 2007, according to a report released by NCI and CDC. There were 3 million cancer survivors in 1971 and 9.8 million in 2001.
March 31, 2011 —Rates of death in the United States from all cancers for men and women continued to decline between 2003 and 2007, the most recent reporting period available, according to the latest Annual Report to the Nation on the Status of Cancer. The report also finds that the overall rate of new cancer diagnoses for men and women combined decreased an average of slightly less than 1% per year for the same period.
June 5, 2011 —NCI announced clinical trial results showing that in a high-risk form of pediatric acute lymphoblastic leukemia, a high-dose schedule of a drug raises already high cure rates even higher.
June 29, 2011 —An analysis of genomic changes in ovarian cancer has provided the most comprehensive and integrated view of cancer genes for any cancer type to date. Ovarian serous adenocarcinoma tumors from 500 patients were examined by The Cancer Genome Atlas (TCGA) Research Network. TCGA researchers completed whole-exome sequencing, which examines the protein-coding regions of the genome, on an unprecedented 316 tumors.
September, 8, 2011 —The NCI-sponsored Costa Rica Vaccine Trial was designed to assess the efficacy of Cervarix in a community-based setting. Two doses of the human papillomavirus vaccine (HPV) Cervarix were as effective as the current standard three-dose regimen after four years of follow-up.
January 19, 2012 —A clinical trial has shown that addition of chemotherapy to radiation therapy leads to a near doubling of median survival time in patients with a form of brain tumor (oligodendroglioma) that carries a chromosomal abnormality called the 1p19q co-deletion.
March 2, 2012 —The Diesel Exhaust in Miners Study looked at 12,315 workers at 8 non-metal mining facilities in the United States. Federal government scientists reported that heavy exposure to diesel exhaust increased risk of death from lung cancer.
March 8, 2012 —In a new examination of United States cancer incidence data, investigators reported that incidence trends have remained roughly constant for glioma, the main type of brain cancer hypothesized to be related to cell phone use.
May 21, 2012— In a study that spanned 20 years, the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, sponsored by NCI, found that sigmoidoscopy is effective in reducing the rates of new cases and deaths due to colorectal cancer. Researchers found that overall colorectal cancer mortality (deaths) was reduced by 26% and incidence (new cases) was reduced by 21% as a result of screening with sigmoidoscopy.
September 24, 2012 —A study from The Cancer Genome Atlas captured a complete view of genomic alterations in breast cancer and classified them into four intrinsic subtypes, one of which shares many genetic features with high-grade serous ovarian cancer, the most malignant form of ovarian cancer which accounts for up to 70% of all ovarian cancer cases.
September 27, 2012 —Scientists may have discovered why a protein called MYC can provoke a variety of cancers. Like many proteins associated with cancer, MYC helps regulate cell growth. A study carried out by researchers at NIH and colleagues found that, unlike many other cell growth regulators, MYC does not turn genes on or off, but instead boosts the expression of genes that are already turned on.
2013 —NCI established the RAS Initiative to mobilize the cancer research community to develop ways to understand and target cancers driven by mutant RAS genes in an open model of collaboration among government, academic, and industry researchers. More than 30 percent of all human cancers are driven by mutations of the RAS family of genes. This approach is called a "hub and spoke" model. The Frederick National Laboratory for Cancer Research (FNLCR) acts as the hub that connects to the larger community of RAS researchers around the world combining efforts and creating new ways to approach the complex issue of RAS.
September 19, 2013 —A world-wide competition to bring emerging breast cancer technologies to market was launched by the Avon Foundation for Women, in partnership with NCI and the Center for Advancing Innovation. The Avon Foundation funded $250,000 in grants to launch the Breast Cancer Start-up Challenge aimed at teams of business, legal, medical/scientific, engineering, and computer science students, as well as seasoned entrepreneurs. Teams were offered the opportunity to create strategic business plans and the potential to start new companies based on the development of 10 unlicensed breast cancer inventions by turning them into commercially marketed products. Breast cancer inventions include therapeutics, diagnostics, prognostics, one device, one vaccine, and a health IT invention, all from the NCI intramural Center for Cancer Research and Avon Foundation-funded university labs.
October 10, 2013 —Glioblastoma multiforme (GBM) was the first cancer type to be systematically studied by The Cancer Genome Atlas Research Network (TCGA) in 2008. In a new, complementary report, TCGA experts examined more than 590 GBM samples—the largest to date utilizing genomic characterization techniques and nearly 400 more than were examined in 2008—to identify several additional significantly mutated genes in GBM.
November 13, 2013 —A trial conducted by researchers at NCI showed adult patients with a type of cancer known as Burkitt lymphoma had excellent long-term survival rates—upwards of 90 percent—following treatment with low-intensity chemotherapy regimens. Standard treatment for Burkitt lymphoma involves high-dose chemotherapy, which has a high rate of toxicity, including death, and cures only 60 percent of adult patients.
November 20, 2013 —NCI scientists report that the incidence of oropharyngeal cancer significantly increased during the period 1983-2002 among people in countries that are economically developed. Recent studies from several countries have reported rising incidence of oropharyngeal cancers and subsequent studies have shown the human papilloma virus (HPV) as the potential cause. Researchers note that prophylactic HPV vaccine has been shown to protect against oral HPV infection, suggesting an additional benefit of vaccination programs for both women and men.
March 1, 2014 —NCI transformed its longstanding Cooperative Group program into the new National Clinical Trials Network (NCTN). Recent advances in deciphering the cancer genome have enabled the development of targeted therapies. To explore targeted therapies, cancer clinical trials need to screen large numbers of patients with the same or different histologic tumor types to identify those patients whose tumors contain the distinct molecular targets of the therapies being tested. NCI’s NCTN was developed to meet these new scientific challenges and is organized to take maximal advantage of the opportunities afforded by the improved understanding of tumor biology as well as the improved efficiencies created by the centralization and streamlining of many critical functions, such as tissue banks, ethics approvals, and imaging support.
March 5, 2014— Ten winners of a world-wide competition to bring emerging breast cancer research technologies to market faster were announced today by the Avon Foundation for Women, in partnership with the NCI, and the Center for Advancing Innovation (CAI). Avon is providing $250,000 in funding for this challenge.
August 18, 2014 —In NCI’s 5 to 6-year ALCHEMIST Trial (Adjuvant Lung Cancer Enrichment Marker Identification and Sequencing Trials), 6,000-8,000 participant’s surgically removed tumors will be tested in a central laboratory for genetic changes in the epidermal growth factor receptor (EGFR) gene and anaplastic lymphoma kinase (ALK) gene. ALCHEMIST represents three integrated, precision medicine trials that are designed to identify people with early-stage lung cancer who have tumors that harbor EGFR and ALK gene alterations and evaluate whether drug treatments targeted against those molecular changes can lead to improved survival compared to current standard of care therapy alone (e.g., chemotherapy with or without radiotherapy after complete surgical resection as prescribed by a participant’s treating physician).
August 30, 2014 —In a large international collaborative analysis of risk factors for non-Hodgkin lymphoma (NHL), NCI scientists were able to quantify risk associated with medical history, lifestyle factors, family history of blood or lymph-borne cancers, and occupation for 11 different NHL subtypes, including less common subtypes. These findings provide crucial insight into the diverse factors that drive different NHL subtypes and correspond with their biological and clinical characteristics.
October 7, 2014 —President Obama announced that John Schiller, Ph.D., Laboratory of Cellular Oncology (LCO), Center for Cancer Research, NCI; and Douglas Lowy, M.D., also from LCO and NCI (then) deputy director, would be recipients of the National Medal of Technology and Innovation—the nation's highest honor for technological achievement. The honorees received their medals at a White House ceremony later in 2014 as recognition for their outstanding contributions to discoveries that enabled the development of HPV vaccines.
2014 —The NCI Community Oncology Research Program (NCORP) is launched. NCORP is a national network of investigators, cancer care providers, academic institutions, and other organizations. NCORP replaced NCI's previously supported community networks: Community Clinical Oncology Program and the NCI Community Cancer Centers Program. NCORP conducts multi-site cancer clinical trials and studies in diverse populations in community-based healthcare systems across the United States and Puerto Rico with a goal of NCORP bringing cancer clinical trials and cancer care delivery research to individuals in their own communities.
2015 —President Obama announced a research effort focusing on bringing precision medicine to many aspects of healthcare. $216 million in funding was allocated to NCI and FDA for the initiative. Researchers at NCI intend to use this approach to find new, more effective treatments for various kinds of cancer based on increased knowledge of the genetics and biology of the disease and scientists hope to apply precision medicine to all areas of health and healthcare.
January 27, 2015 —In the largest prospective study to date of image-guided technology for identifying suspicious regions of the prostate to biopsy, NCI researchers compared the ability of this technology to detect high-risk prostate cancer with that of the current standard of unguided prostate biopsy. The image-guided approach, called MR/US fusion biopsy, combines targeted magnetic resonance (MR) imaging with transrectal ultrasound (US) to identify regions of suspected cancer to biopsy, whereas the current standard of detection, performed with ultrasound alone, involves biopsy of the entire prostate with twelve needles to remove core samples from separate areas of the organ.
April 20, 2015 —A new NCI study shows that inherited variations in a known tumor suppressor gene among children and adolescents with osteosarcoma, a cancer of the bone, are more common than previously thought. Older patients who are also susceptible to this malignancy were not found to carry mutations in the gene, known as TP53.
June 1, 2015 —Investigators for the nationwide trial, NCI-MATCH (Molecular Analysis for Therapy Choice), announced that the precision medicine trial will open to patient enrollment. NCI-MATCH analyzes patients’ tumors to determine whether they contain gene abnormalities for which a targeted drug exists and assigns treatment based on the abnormality. The study was co-developed by NCI and the ECOG-ACRIN Cancer Research Group, a cooperative group that was formed by the merger of the Eastern Cooperative Oncology Group (ECOG) and the American College of Radiology Imaging Network (ACRIN).
August 13, 2015 —Using novel large-scale imaging technology, NCI intramural researchers announced they have mapped the spatial location of individual genes in the nucleus of human cells and identified 50 cellular factors required for the proper three-dimensional (3D) positioning of genes. These spatial locations play important roles in gene expression, DNA repair, genome stability, and other cellular activities.
January 12, 2016 —During his 2016 State of the Union Address, President Obama called on Vice President Biden to lead a new, national “Moonshot” initiative to eliminate cancer as we know it. The goal is to double the rate of progress against cancer, achieving in five years what otherwise would have taken ten. The White House announced a $1 billion initiative to jumpstart this work.
May 16, 2016 —NCI scientists found that leisure-time physical activity was associated with lower risks of 13 cancer types (esophageal adenocarcinoma, liver, lung, kidney, gastric cardia, endometrial, myeloid leukemia, myeloma, colon, head and neck, rectal, bladder, and breast). Most of these associations were evident regardless of body mass index or smoking history. These findings confirm and extend the evidence for a benefit of physical activity on cancer risk and support its role as a key component of population-wide cancer prevention.
June 29, 2016 —NCI’s Genomic Data Commons (GDC) is announced. This data sharing platform promotes precision medicine in oncology. It is an expandable knowledge network supporting the import and standardization of genomic and clinical data from cancer research programs. The GDC contains NCI-generated data from some of the largest and most comprehensive cancer genomic datasets, including The Cancer Genome Atlas (TCGA) and Therapeutically Applicable Research to Generate Effective Therapies (TARGET). As more researchers add clinical and genomic data to the GDC, it will become an even more powerful tool for making discoveries about the molecular basis of cancer that may lead to better care for patients.
July 11, 2016 —In the spirit of collaboration inspired by the Cancer Moonshot, the Department of Veterans Affairs (VA), the Department of Defense (DoD), and NCI announced a new tri-agency coalition to help cancer patients by enabling their oncologists to more rapidly and accurately identify effective drugs to treat cancer based on a patient’s unique proteogenomic profile. The APOLLO Network (Applied Proteogenomics OrganizationaL Learning and Outcomes) will look at both a patient’s genes (genomic analysis) and the expression of these genes in the form of proteins (proteomic analysis) to create the nation’s first system in which cancer patients are routinely screened for genomic abnormalities and proteomic information to match their tumor types to targeted therapies. Initially, APOLLO is focusing on a combined cohort of 8,000 cancer patients within the nation’s two largest healthcare systems — the VA and DoD — with the aim of expanding the program to additional cancer types and making findings available to physicians across the country.
September 7, 2016 —NCI Acting Director Douglas Lowy, M.D., accepted the recommendations of a Blue Ribbon Panel (BRP) on 10 scientific approaches most likely to make a decade’s worth of progress against cancer in five years under the Cancer Moonshot. The report was presented by the BRP to the National Cancer Advisory Board (NCAB), and it was subsequently considered and accepted by the NCAB with revisions that reflect NCAB’s discussion.
December 7, 2016— In a study of an immune therapy for colorectal cancer that involved a single patient, researchers identified a method for targeting the cancer-causing protein produced by a mutant form of the KRAS gene.
December 28, 2016 —In an early-phase intramural clinical trial of a new oral drug, selumetinib, children with the common genetic disorder neurofibromatosis type 1 (NF1) and plexiform neurofibromas, tumors of the peripheral nerves, tolerated selumetinib and, in most cases, responded to it with tumor shrinkage. At present, no therapies are considered effective for NF1-related large plexiform neurofibromas, but, in this trial, partial responses, meaning 20 percent or more reduction in tumor volume, were observed in over 70 percent of the patients. NF1 affects 1 in 3,000 people.
NCI Legislative Chronology
February 4, 1927 —Senator M. M. Neely, West Virginia, introduced Senate Bill 5589 to authorize a reward for the discovery of a successful cure for cancer. The reward was to be $5 million.
March 7, 1928 —Senator M. M. Neely introduced Senate Bill 3554 to authorize the National Academy of Sciences to investigate the means and methods for affording Federal aid in discovering a cure for cancer and for other purposes.
April 23, 1929 —Senator W. J. Harris, Georgia, introduced Senate Bill 466 to authorize the Public Health Service and the National Academy of Sciences jointly to investigate the means and methods for affording Federal aid in discovering a cure for cancer and for other purposes.
April 2, 1937 —Senator Homer T. Bone, Washington, introduced Senate Bill 2067 authorizing the Surgeon General of the Public Health Service to control and prevent the spread of the disease of cancer, authorizing an annual appropriation of $1 million.
April 29, 1937 —Congressman Maury Maverick, Texas, introduced House Resolution 6767 to promote research in the cause, prevention, and methods of diagnosis and treatment of cancer, to provide better facilities for the diagnosis and treatment of cancer, to establish a National Cancer Center in the Public Health Service, and for other purposes. It authorizes an appropriation of $2,400,000 for the first year and $1 million annually thereafter.
August 5, 1937 —The National Cancer Institute Act establishes the National Cancer Institute as the federal government’s principal agency for conducting research and training on the cause, diagnosis, and treatment of cancer. The bill also calls upon NCI to assist and promote similar research at other public and private institutions. An appropriation of $700,000 for each fiscal year is authorized. (P.L. 75-244)
March 28, 1938 —House Joint Resolution 468, 75th Congress, was passed, "To dedicate the month of April in each year to a voluntary national program for the control of cancer."
July 1, 1944 —The Public Health Service Act, P.L. 410, 78th Congress, provided that "The National Cancer Institute shall be a division in the National Institute of Health." The act also revised and consolidated many revisions into a single law. The limit of $700,000 annual appropriation was removed.
December 23, 1971 —The National Cancer Act of 1971 provides increased authorities and responsibilities for the NCI Director; initiating a National Cancer Program; establishing a 3-member President's Cancer Panel and a 23-member National Cancer Advisory Board, the latter replacing the National Advisory Cancer Council; authorizing the establishment of 15 new research, training, and demonstration cancer centers; establishing cancer control programs as necessary for cooperation with state and other health agencies in the diagnosis, prevention, and treatment of cancer; and providing for the collection, analysis, and dissemination of all data useful in the diagnosis, prevention, and treatment of cancer, including the establishment of an international cancer data research bank. (P.L. 92-218)
November 9, 1978 —The Community Mental Health Centers Act amends the National Cancer Act to emphasize education and demonstration programs in cancer treatment and prevention, and stipulates that NCI devote more resources to prevention, focusing particularly on environmental, dietary and occupational cancer causes. (P.L. 95-622)
November 4, 1988 —The Health Research Extension Act of 1988 provides a two-year extension, which reaffirms the special authorities of NCI and added information dissemination mandates. A representative from the Department of Energy was added to the National Cancer Advisory Board as an ex officio member. (P.L. 100-607)
June 10, 1993 —The NIH Revitalization Act of 1993 encourages NCI to expand and intensify its efforts in breast cancer and other women's cancers and authorized increased appropriations. Similar language is included for prostate cancer. (P.L. 103-43)
August 13, 1998 —The Stamp Out Breast Cancer Act establishes a special alternative rate of postage up to 25% higher than a regular first-class stamp. 70% of the profits from the sale of the stamp, also referred to as a semipostal, would go to the NIH to fund breast cancer research; the remaining 30% would go to the U.S. Department of Defense breast cancer research. (PL 105-41)
July 10, 2000 —The Radiation Exposure Compensation Amendments of 1999 allow more workers who handled radioactive material for weapons programs to be eligible to receive federal compensation for radiation-induced illness. (P.L. 106-245)
July 28, 2000 —The Semipostal Authorization Act gives the U.S. Postal Service the authority to issue semipostal stamps, which are sold at a premium in order to help provide funding for a particular area of research. The law also extends the Breast Cancer Stamp Act until July 29, 2002. (P.L. 106-253)
January 4, 2002 —The Best Pharmaceuticals for Children Act is designed to improve the safety and efficacy of pharmaceuticals for children, by reauthorizing legislation that encourages pediatric drug research by giving drug companies an incentive of six months of additional market exclusivity to test their products for use in children. (P.L. 107-109)
May 14, 2002 —The Hematologic Cancer Research Investment and Education Act of 2002 directs the NIH Director, through the NCI Director, to conduct and support research on blood cancers. In addition, the CDC is directed to establish and carry out an information and education program. (P.L. 107-172)
September 10, 2002 —The Public Health Security and Bioterrorism Preparedness and Response Act contains a provision instructing Federal agencies to stockpile and distribute potassium iodide (KI) to protect the public from thyroid cancer in the event of a radiation emergency. (P.L. 107-188)
June 30, 2005 —The Patient Navigator Outreach and Chronic Disease Prevention Act of 2005 amends the Public Health Service Act to authorize a demonstration grant program to provide patient navigator services to reduce barriers and improve health care outcomes. The bill directs the HHS Secretary to require each recipient of a grant under this section to use the grant to recruit, assign, train, and employ patient navigators who have direct knowledge of the communities they serve to facilitate the care of individuals who have cancer or other chronic diseases. The bill also directs the HHS Secretary to coordinate with, and ensure the participation of, the Indian Health Service, NCI, the Office of Rural Health Policy, and such other offices and agencies as deemed appropriate by the Secretary, regarding the design and evaluation of the demonstration programs. (P.L. 109-18)
November 11, 2005 —The 2-Year Extension of Postage Stamp for Breast Cancer Research extends the U.S. Postal Service's authority to issue special postage stamps to help provide funding for breast cancer research through December 31, 2007. (P.L. 109-100)
January 12, 2007 —The Gynecologic Cancer Education and Awareness Act of 2005, or "Johanna's Law" directs the HHS Secretary to carry out a national campaign to increase the awareness and knowledge of health care providers and women with respect to gynecologic cancers. (P.L. 109-475)
April 20, 2007 —The National Breast and Cervical Cancer Early Detection Program Reauthorization Act of 2007 allows states to apply for federal waivers to spend a greater share of funds on hard-to-reach underserved women. This bill authorizes funding up to $275 million by 2012; $201 million is authorized for 2007. (P.L. 110-18)
September 27, 2007 —The FDA Amendments Act of 2007 amends the Federal Food, Drug, and Cosmetic Act to reauthorize the collection of prescription drug user fees for FY2008–FY2012. Requires NIH to expand the clinical trial registry ( clinicaltrials.gov ) and creates a clinical trial results database. (P.L. 110-85)
December 12, 2007 —The Breast Cancer Research Stamp Reauthorization Act extends through December 31, 2011, provisions requiring the U.S. Postal Service to issue a special postage stamp which contributes to funding breast cancer research. (P.L. 110-150)
July 29, 2008 —The Caroline Pryce Walker Childhood Cancer Act of 2007 amends the Public Health Service Act to advance medical research and treatments into pediatric cancers, ensure patients and families have access to the current treatments and information regarding pediatric cancers, establish a population-based national childhood cancer database, and promote public awareness of pediatric cancers. (P.L. 110-287)
October 8, 2008 —The Breast Cancer and Environmental Research Act of 2007 amends the Public Health Service Act to authorize the Director of the National Institute of Environmental Health Sciences to make grants for the development and operation of research centers regarding environmental factors that may be related to the etiology of breast cancer. The bill establishes an Interagency Breast Cancer and Environmental Research Coordinating Committee within HHS. (P.L. 110-354)
February 4, 2009 —The Children's Health Insurance Program Reauthorization Act of 2009 increases the tax on cigarettes by 62 cents to $1.01 per pack and raises taxes on other tobacco products, in order to offset the cost of the program expansion. (P.L. 113-3)
February 17, 2009 —The American Recovery and Reinvestment Act of 2009 provides $10 billion in additional funding for the NIH; of which NCI received $1.3 billion in Recovery Act funds to be distributed during the two-year span of 2009 and 2010. (P.L. 111-5)
June 21, 2009 —The Family Smoking Prevention and Tobacco Control Act provides the FDA with the authority to regulate tobacco products and establishes within the FDA, the Center for Tobacco Products to implement this act. The Act allows the Secretary of HHS to restrict the sale or distribution and the advertising or promotion of tobacco products, if appropriate for the protection of the public health, and to the full extent permitted by the First Amendment. (P.L. 111-31)
March 23, 2010 —The Patient Protection and Affordable Care Act (HR 3590), the health care reform bill, establishes a private non-profit institute called the Patient-Centered Outcomes Research Institute to conduct comparative clinical effectiveness research, obtain and use data from the Federal government, and establish advisory panels to advise on research priorities, among other provisions. The bill requires NIH to conduct research to develop and validate new screening tests for breast cancer. The bill also requires the NIH Director to establish a Cures Acceleration Network (CAN) program, which shall award grants and contracts to eligible entities to accelerate the development of high need cures and therapies, including the development of medical products, drugs or devices, or biological products. (P.L. 111-148)
March 31, 2010 —The Prevent All Cigarette Trafficking Act of 2009 prevents tobacco smuggling, ensures the collection of all tobacco taxes, and includes smokeless tobacco as a regulated substance. The bill amends the federal criminal code to treat cigarettes and smokeless tobacco as non-mailable and prohibit such items from being deposited in or carried through the U.S. mail. (P.L.111-154)
December 23, 2011 —The Breast Cancer Research Stamp Reauthorization Act reauthorized provisions requiring the U.S. Postal Service to issue a special postage stamp which contributes to funding breast cancer research, extending them through 2015. (P.L. 112-80)
January 2, 2013 —The Recalcitrant Cancer Research Act of 2012 passed as an amendment to the National Defense Authorization Act for Fiscal Year 2013. The legislation calls for NCI to develop a scientific framework for research on two cancers that have a five-year relative survival rate of less than 20 percent, and are estimated to cause the death of at least 30,000 individuals in the United States per year. Pancreatic cancer and lung cancer meet these criteria. (P.L. 112-239)
December 11, 2015 —The Breast Cancer Stamp Reauthorization Act reauthorized the issuance of semipostal stamps for breast cancer research, through 2019. (P.L. 114-19)
December 13, 2016— The 21 st Century Cures Act increases funding for biomedical research, and aims to enhance the speed at which drugs are developed and approved. Key NIH provisions aim to coordinate policies relating to early career investigators, improve loan repayment programs, and streamline procedural requirements for attendance at scientific meetings. The bill reauthorizes the NIH for FY2018-FY2020 and creates a $4.8 billion NIH Innovation Account. This account supports the work of the Beau Biden Cancer Moonshot at a level of $1.8 billion over seven years, as well as the Precision Medicine Initiative, the BRAIN Initiative, and specific regenerative medicine research. The funds in the Account must be appropriated annually.
Biographical Sketch of NCI Director Dr. W. Kimryn Rathmell

W. Kimryn Rathmell, M.D., Ph.D., M.M.H.C., was sworn in as the 17th NCI director on December 18, 2023. She previously led the Vanderbilt University Medical Center as physician-in-chief and chair of the Department of Medicine.
Dr. Rathmell is a recipient of the 2019 Louisa Nelson Award for Women of Achievement, Vision, and Inspiration , the 2019 Eugene P. Schonfeld Award from the Kidney Cancer Association , and the Paragon Award for Research Excellence from the Doris Duke Foundation . She was a leader of The Cancer Genome Atlas’s (TCGA) kidney cancer projects and served as a TCGA analysis working group member across the spectrum of cancers, winning the 2020 American Association for Cancer Research Team Science Award . She has served on the NCI Board of Scientific Advisors , and the Forbeck Foundation Scientific Advisory Board.
Dr. Rathmell has held leadership positions with the American Society of Clinical Oncology and the American Society for Clinical Investigation, serving as secretary–treasurer and president. As a result of her efforts, Dr. Rathmell has been elected to the Association of American Physicians, the American Academy of Arts and Sciences, and the National Academy of Medicine.
Dr. Rathmell’s specialty is the research and treatment of complex and hereditary kidney cancers. She also focuses on underlying drivers of kidney cancers using genetic, molecular, and cell biology to develop interventions to improve patients’ lives. Dr. Rathmell’s research has resulted in more than 250 articles in leading peer-reviewed journals, including The New England Journal of Medicine, Nature, Proceedings of the National Academy of Sciences, and the Journal of Clinical Investigation.
Dr. Rathmell earned undergraduate degrees in biology and chemistry from the University of Northern Iowa and her Ph.D. in biophysics and M.D. from Stanford University. She completed an internal medicine internship at the University of Chicago and an internal medicine residency, medical oncology fellowship, and postdoctoral studies at the University of Pennsylvania. In 2022, she completed her Master of Management in Health Care from the Vanderbilt University Owen Graduate School of Management.
NCI Directors
National cancer institute research programs.
The National Cancer Institute leads the National Cancer Program through its operation of research components that provide support for extramural and intramural cancer-related research and through its outreach and collaborations within the cancer community worldwide.
Cancer research is conducted with NCI funding in nearly every state in the United States and more than 20 foreign countries, in addition to research conducted at its own facilities. NCI supports cancer research training, education, and career development, and provides leadership for setting national priorities in cancer research.
NCI Research Components
Center for cancer research, division of cancer epidemiology and genetics, division of cancer biology, division of cancer control and population sciences, division of cancer prevention, division of cancer treatment and diagnosis, division of extramural activities, center for cancer genomics, center for cancer training, center for global health, center for strategic scientific initiatives, center to reduce cancer health disparities, office of hiv and aids malignancy, small business innovation research development center, office of cancer centers, frederick national laboratory for cancer research.
The CCR is the largest division of the NCI intramural research program and comprises over 230 basic and clinical research groups located on two campuses outside of Washington, D.C.
The CCR is home to an extraordinary group of scientists and clinicians exploring the cutting-edge of cancer and HIV/AIDS research. Our scientists work on a wide spectrum of biological and biomedical problems ranging from visualizing and understanding the structure of individual genes and proteins, developing novel methods for drug discovery, to inventing biomedical devices and technology and creating innovative ways to treat patients in the NIH Clinical Center.
Our scientists enjoy complete intellectual freedom and are expected to creatively and innovatively explore the most important questions in the field of cancer research and treatment. We support projects over a long time horizon allowing our investigators to pursue some of the most difficult, high-risk problems in the field and we are always on the lookout for new challenges and the most pressing problems in modern cancer research.
The success of the CCR is grounded in an exceptionally strong discovery research program which provides the foundation for the seamless translation of insights into basic cellular and molecular processes to clinical applications and patient care. Examples of our success are the development of ground-breaking immunotherapy approaches, HIV/AIDS test and the creation of human papilloma virus vaccine.
The CCR is a unique place of science where we combine diverse expertise with the freedom to thoroughly pursue the most pressing questions in cancer biology and treatment.
Additional information is available at https://ccr.cancer.gov
Through its broad programs in epidemiology, genetics, statistics, and related areas, the intramural Division of Cancer Epidemiology and Genetics (DCEG) carries out population-based and interdisciplinary research both nationally and internationally to discover the genetic and environmental determinants of cancer. DCEG is uniquely positioned to conduct value-added epidemiologic research projects that are high-risk in nature and require (a) long-term commitments of scientific staff and funding support through contracts, (b) a coordinated national programmatic approach, or (c) a rapid response to emerging public health or scientific issues. The Division develops multi-disciplinary infrastructures and resources for use throughout the scientific community, including database management software for genome-wide association studies, biospecimen inventories, family-based studies, a variety of software packages for exposure assessment, and interactive cancer mortality atlases to generate leads into the environmental determinants of cancer. DCEG also has a firm commitment to training the next generation of scientists, and has trainees from the predoctoral to postdoctoral stage. The research conducted by the Division often provides a scientific basis for public health recommendations and policies.
The Epidemiology and Biostatistics Program consists of five branches that conduct independent and collaborative epidemiologic and biostatistical investigations to identify the distribution, characteristics, and causes of cancer in human populations. The Program investigates demographic variation in the occurrence of cancer by age, race, gender, geography, and over time. Special emphasis is placed on the carcinogenic effects of occupational and environmental exposures, ionizing and non-ionizing radiation, dietary and metabolic factors, medicinal agents such as hormones, infectious agents, and host factors including genetic susceptibility to cancer-causing exposures. The Program also develops biostatistical methods for family-based and population-based studies on cancer etiology and prevention.
The Human Genetics Program provides an expanded focus for interdisciplinary research into the genetic determinants of human cancer. Its branches and laboratory explore and identify heritable factors that predispose to cancer, including studies of gene-environment interactions. Program investigators study cancer-prone families to identify and clone predisposing genes; investigate the prevalence of identified genes in the general population; conduct pharmacogenetic studies to evaluate genetic polymorphisms as determinants of cancer risk and treatment outcomes; conduct integrative analyses of environmental and germline risk factors with comprehensive data on histological and molecular profiling of tumors and their precursors, including somatic genomic analyses; and translate advances in molecular genetics into evidence-based management strategies. The Laboratory of Translational Genomics examines validated regions of the genome associated with cancer risk, laying the groundwork for functional studies to determine the causal variants and biological mechanisms involved. These activities are complemented by the NCI Cancer Genomics Research Laboratory, where genome-wide association studies and next generation sequencing are carried out to uncover the heritable components to cancer.
Fellows in the DCEG Fellowship Program work with world class scientists to explore the causes of cancer and new approaches to its prevention. Predoctoral and postdoctoral fellows carry out, analyze, and publish population, family, and laboratory-based studies. They gain experience in diverse study designs, novel analytic techniques, and genomics and informatics. Professional skills development and preparation for future careers in epidemiology and related areas are an integral part of the program. For more information and to apply, visit our Web site at: http://dceg.cancer.gov/fellowship-training .
Additional information is available at http://dceg.cancer.gov .
The Division of Cancer Biology (DCB) supports basic research in all areas of cancer biology and provides the research foundation that improves understanding of the disease. This basic research may lead to new approaches for prevention, diagnosis, and treatment. Research on basic cancer biology provides the building blocks to new treatments and clinical trials. DCB provides scientific management for approximately 2,000 grants each year. DCB facilitates investigator-initiated research by working with individual investigators, professional societies, and research institutions to provide information, advice, and guidance on opportunities for research support. At the forefront of cancer research, DCB establishes program priorities by identifying and addressing emerging scientific areas or gaps in the scientific research portfolio and reports on scientific progress and program accomplishments to the scientific community, NCI, Congress, and the public.
Basic research is supported by the Division in the following major research areas: cancer cell biology; cancer immunology, hematology, and etiology; DNA and chromosome aberrations; structural biology and molecular applications; tumor biology and microenvironment; and tumor metastasis.
Special research programs within DCB include: Physical Sciences-Oncology Network, Cancer Systems Biology Consortium, Oncology Models Forum, Barrett's Esophagus Translational Research Network, New Approaches to Synthetic Lethality for Mutant KRAS-Dependent Cancers, Molecular and Cellular Characterization of Screen-Detected Lesions, Fusion Oncoproteins in Childhood Cancers, and Cancer Tissue Engineering Collaborative.
In addition, the Division sponsors several resources for cancer researchers including bioinformatics tools for analyzing data, such as a state-of-the-art X-ray crystallography experimental facility funded through the GM/CA CAT Project , and data and specimen repositories such as The Chernobyl Tissue bank and The International Registry of Werner Syndrome .
Additional information is available at https://cancer.gov/dcb .
The Division of Cancer Control and Population Sciences (DCCPS), NCI’s bridge to public health research, practice, and policy, plays a unique role in reducing the burden of cancer in America. DCCPS, an extramural division, supports research in surveillance, epidemiology, health services, behavioral science, and cancer survivorship. The division also plays a central role within the federal government as a source of expertise and evidence on issues such as the quality of cancer care, the economic burden of cancer, geographic information systems, statistical methods, communication science, comparative effectiveness research, obesity and tobacco control, and the translation of research into practice.
The DCCPS philosophy that scientific progress in the 21st century will depend on the transdisciplinary integration of research methods, models, and levels of analysis drives the focus on varied and complex expertise and backgrounds of the division’s scientific staff. In addition to an emphasis on epidemiology and biostatistics, DCCPS has made a special effort to recruit experts in disciplines such as communication, anthropology, outcomes research, psychometrics, medical genetics, health psychology, economics, social work, policy analysis, geography, and family medicine. DCCPS programs include: Behavioral Research Program, Epidemiology & Genomics Research Program, Healthcare Delivery Research Program, and Surveillance Research Program. The Office of Cancer Survivorship is housed within DCCPS and promotes a better understanding of the unique needs of cancer survivors and how to address those needs.
Additional information is available at http://cancercontrol.cancer.gov .
The Division of Cancer Prevention (DCP) conducts and supports research to determine a person's risk of developing cancer and to find ways to reduce that risk. Through laboratory, clinical, and epidemiologic research, scientists have shown that the diseases of cancer occur not as single, catastrophic events, but rather as the result of a complex and long-evolving molecular process. The intervals between initiation of the cancer process and occurrence of the invasive disease vary by organ and tissue sites, and some may take decades. DCP research portfolio focuses across this span, with a goal to detect changes and intervene early in the cancer process to prevent disease and death.
Research groups include: Chemopreventive Agent Development Research Group, Community Oncology and Prevention Trials Research Group, Nutritional Science Research Group, Cancer Biomarkers Research Group, Early Detection Research Group, Biometry Research Group, and four organ system research groups.
Additional information is available at http://prevention.cancer.gov .
The Division of Cancer Treatment and Diagnosis (DCTD) takes prospective detection and treatment leads, facilitates their paths to clinical application, and expedites the initial and subsequent large-scale testing of new agents, biomarkers, imaging tests, and other therapeutic interventions (radiation, surgery, immunotherapy) in patients. Investigators supported by the division engage in scientifically sound, high-risk research that may yield great benefits for patients with cancer, but are too difficult or risky for industry or academia to pursue. This includes a particular emphasis on the development of distinct molecular signatures for cancer, refined molecular assays, and state-of-the-art imaging techniques that will guide oncologic therapy in the future as well as a commitment to precision medicine initiatives.
The division has eight major programs that work together to bring unique molecules, diagnostic tests, and therapeutic interventions from the laboratory bench to the patient bedside: The Biometric Research Program, The Cancer Diagnosis Program, The Cancer Imaging Program, The Cancer Therapy Evaluation Program, The Developmental Therapeutics Program, The Radiation Research Program, The Translational Research Program, and The Office of Cancer Complementary and Alternative Medicine.
Additional information is available at http://dctd.cancer.gov
The Division of Extramural Activities (DEA) was established to provide NCI and the scientific community with expert scientific review of the merits of extramural research, procedures, and policies to help the Institute achieve its goal. DEA coordinates NCI's extramural initiatives by guiding funding, providing scientific peer review and oversight, coordinating advisory committees, establishing policies and procedures, managing extramural staff training and career development, and coding and tracking NCI's research portfolio. DEA staff members serve as chief NCI liaisons to the extramural cancer research community, processing approximately 12,000 grant applications for referral and recruiting thousands of scientific experts to review approximately 3,000 grants per year. The DEA's Committee Management Office handles the complex preparation and logistics required for NCI's advisory groups to function productively and for the HHS Secretary's Advisory Committee on Genetics, Health, and Society to act in its prescribed role.
Additional information is available at http://deainfo.nci.nih.gov .
NCI established the Center for Cancer Genomics (CCG) in 2011 to develop and apply genome science to improve the diagnosis and treatment of cancer patients. CCG promotes collaborations of national and international agencies, academic researchers, and community physicians to foster research based on genomes, gene expression, proteomics, and other technologies to usher in a modern era of integrated and individualized prevention, diagnosis, and treatment of cancer, while ensuring responsible use of genetic information. Through research on the structure and function of the molecular make-up of human tumor cells and the human genome, researchers funded by CCG have identified many genes involved in cancer that are informing knowledge of biologic function, drug development, and DNA-based diagnostics.
CCG and the offices it oversees—The Cancer Genome Atlas (TCGA) and the Office of Cancer Genomics (OCG)—manage multiple programs. These offices serve to advance CCG's goal of ushering in a modern era of diagnosis, treatment, and prevention based on the study of genomes. Programs include: Genomic Data Commons, Cancer Driver Discovery Program, Cancer Genome Characterization Initiative, Cancer Target Discovery and Development Network, Human Cancer Models Initiative, and Therapeutically Applicable Research to Generate Effective Treatments.
Additional information is available at https://www.cancer.gov/ccg .
The Center for Cancer Training (CCT) is committed to catalyzing the development of a 21st century workforce capable of advancing cancer research through a scientifically integrated approach. CCT coordinates and provides research training and career development activities for NCI's laboratories, clinics, and other research groups. These cancer training and career development opportunities cover a broad spectrum of disciplines for individuals at career stages ranging from high school and graduate students to scientists, clinicians, and health care professionals. CCT is responsible for developing, coordinating, and implementing opportunities for support of cancer research training, career development, and education at institutions nationwide. CCT identifies workforce needs in cancer research and adapts NCI's training and career development programs and funding opportunities to address these needs. CCT creates new opportunities that enhance recruiting and retention, increase partnerships, and generate diversity awareness.
Additional information is available at http://www.cancer.gov/cct .
The Center for Global Health (CGH) was established in 2011 to help reduce the global burden of cancer. CGH develops initiatives and collaborates with other NCI divisions, NCI-designated cancer centers, and countries to support cancer control planning build capacity, and support cancer research and cancer research networks in low- and middle-income countries. CGH serves as the focal point for all global health activities within NCI by leading the development of global cancer research priorities, providing strategic vision to the global cancer community, and pursuing strategies directed towards control of cancer on a global scale.
CGH conducts and supports international cancer research, training, health information dissemination, and other relevant biomedical research programs. It coordinates collaborations and partnerships with other agencies and organizations engaged in efforts to improve global health. Research programs and initiatives include: Cancer Control Planning, Capacity Building, and Cancer Research and Research Networks.
Additional information is available at https://www.cancer.gov/about-nci/organization/cgh .
The Center for Strategic Scientific Initiatives (CSSI) focuses on creating and uniquely implementing exploratory programs focused on the development and integration of advanced technologies, trans-disciplinary approaches, infrastructures, and standards to accelerate the creation of publicly available, broadly accessible, multi-dimensional data, knowledge, and tools to empower the entire cancer research continuum for patient benefits. Since its inception, CSSI has undertaken a number of programs and initiatives that have contributed significantly to addressing major barriers and opportunities in cancer research. These initiatives are also designed to enable advances that can be translated to the clinic and substantially impact patient care.
CSSI programs build databases, knowledge, tools and extramural trans-disciplinary scientific teams to promote the themes of the center. Offices include: CSSI Office of the Director, Office of Cancer Clinical Proteomics Research , and Office of Cancer Nanotechnology Research .
Additional information can be found at http://cssi.cancer.gov/ .
NCI established the Center to Reduce Cancer Health Disparities (CRCHD) in 2001 to help reduce the unequal burden of cancer in our society by leading NCI’s efforts in workforce diversity by training students and investigators from diverse backgrounds. CRCHD strengthens NCI’s cancer research portfolio to address cancer health disparities throughout NCI, builds regional networks to foster collaboration, enhances capacity in disparities research and career development, and disseminates culturally appropriate, evidence-based cancer information to underserved communities. The National Outreach Network (NON) seeks to strengthen NCI's ability to develop and disseminate culturally appropriate, evidence-based cancer information that is tailored to the specific needs and expectations of underserved communities, working through NON community health educators located at NCI-designated Cancer Centers.
CRCHD supports the following research programs: Community Networks Program Centers, Partnerships to Advance Cancer Health Equity, Basic Cancer Research Program, Continuing Umbrella of Research Experiences, and Geographical Management of Cancer Health Disparities Program.
More information is available at http://crchd.cancer.gov .
The Office of HIV and AIDS Malignancy (OHAM) is responsible for broad oversight of HIV/AIDS and HIV malignancy research throughout NCI. OHAM coordinates and prioritizes NCI research in HIV/AIDS and HIV malignancy and also directly initiates and manages certain research programs. NCI has been at the forefront of HIV/AIDS research since the beginning of the AIDS epidemic and NCI scientists have made a number of critical research contributions.
NCI currently supports robust and varied research through OHAM’s two main programs. The AIDS Malignancy Program identifies new initiatives for international activities, such as the initiative to Strengthen Capacity for HIV-Associated Malignancy Research in Africa , and oversees programs that NCI co-manages with other Institutes. The AIDS Cancer Clinical Program oversees clinical programs in OHAM, including the AIDS Malignancy Consortium and the AIDS and Cancer Specimen Resource .
More information is available at https://oham.cancer.gov .
Small Business Innovation Research (SBIR) and Small Business Technology Transfer (STTR) programs at NCI are managed by the SBIR Development Center. These programs are NCI's engine of innovation for developing and commercializing novel technologies and products to prevent, diagnose, and treat cancer. A range of funding opportunities is offered to the small business community. The center offers advice for applicants and fosters partnerships and collaborations between small businesses and third-party organizations. In addition, the center serves as a mentor to SBIR-funded companies regarding their technology development plans, and their regulatory and commercialization strategies, helping to accelerate the development of novel technologies and products. The primary goal of these efforts is to enhance the return on investment of the SBIR program for the benefit of the cancer community and public health in general. SBIR and STTR serve as two of the largest sources of early-stage technology financing in the United States.
More information is available at http://sbir.cancer.gov .
The Office of Cancer Centers (OCC) program supports 72 NCI-designated Cancer Centers nationwide that are actively engaged in transdisciplinary research to reduce cancer incidence, morbidity, and mortality. These NCI-designated Cancer Centers are a major source of discovery of the nature of cancer and the development of more effective approaches to cancer prevention, diagnosis, and therapy. They also deliver medical advances to patients and their families, educate health-care professionals and the public, and reach out to underserved populations. They are characterized by strong organizational capabilities, institutional commitment, and trans-disciplinary, cancer-focused science; experienced scientific and administrative leadership, and state-of-the-art cancer research and patient care facilities.
NCI-designated Cancer Centers are funded through the P30 Cancer Center Support Grant. These awards fund formal research programs that foster interactions between basic laboratory, clinical, and population scientists; access for investigators to shared services and technologies that are necessary to their research efforts; and other scientific infrastructure.
Additional information can be found at http://cancercenters.cancer.gov .
The Frederick National Laboratory for Cancer Research (FNLCR) is a Federally Funded Research and Development Center (FFRDC) operated by Leidos Biomedical Research, Inc., for NCI. The lab provides quick response capabilities and meets special long-term research and development needs for NCI. FFRDC also supports other Institutes of NIH and a wide range of research collaborations and partnerships with third parties, consistent with NCI’s mission. Activities include building cross-disciplinary collaborations and teams, bridging the gap between late discovery and early development of diagnostics and therapeutics, developing cross-cutting technology platforms, and developing data standards. The overarching goal is to accelerate treatments for cancer and AIDS patients.
FNLCR has advanced technologies and innovative platforms that support NCI’s mission, from basic research to translational and clinical studies. These include Cancer Model Development, Genetics and Genomics, Proteins and Proteomics, Clinical Assay Development, Nanotechnology Characterization, High-Performance Biomedical Computing, and Advanced Biomedical Imaging.
Additional information is available at http://frederick.cancer.gov .
This page last reviewed on March 26, 2024
Connect with Us
- More Social Media from NIH
For the best browsing experience please enable JavaScript. Instructions for Microsoft Edge and Internet Explorer , other browsers

- About cancer
- Get involved
- Our research
- Funding for researchers
- Cancer types
- Cancer in general
- Causes of cancer
- Coping with cancer
- Health professionals
- Do your own fundraising
- By cancer type
- By cancer subject
- Our funding schemes
- Applying for funding
- Managing your research grant
- How we deliver our research
- Find a shop
- Shop online
- Our eBay shop
- Our organisation
- Current jobs
- Cancer news

A history of these pages
Cancer Research UK's About Cancer pages began life as CancerHelp UK. This was one of the first comprehensive cancer websites based in the UK.
Our pages include information about:
- the causes of cancer, how to reduce your risk and healthy living
- cancer symptoms and cancer screening
- cancer tests and treatments
- coping with a diagnosis of cancer and the treatment side effects
- research and clinical trials
The information is accessible, comprehensive and easy to read.
Co founders
The co founders of CancerHelp UK were Nick James and Sally Tweddle.
Nick James is a cancer specialist at the University Hospitals Birmingham NHS Foundation Trust. He is also a Professor of Oncology at the University of Birmingham Institute for Cancer Studies.
Sally Tweddle was an educationalist with an interest in literacy. Her husband's cancer and their search for cancer information online inspired CancerHelp UK.
To begin with, the Medical School server at the University of Birmingham hosted CancerHelp UK.
The management of the site passed to The Cancer Research Campaign in 2000. In 2002, The Cancer Research Campaign and the Imperial Cancer Research Fund merged. Together they formed Cancer Research UK. CancerHelp UK is now the About cancer section of Cancer Research UK's website.
Sarah Jane (Sally) Tweddle (1955–1999)
Sally was instrumental in setting up CancerHelp UK in 1994. At the time, most online cancer information was aimed at professionals. There was little information available for patients and relatives.
Sally’s background was in education. She saw how to present effective, detailed online material to the general public. The website launch was a success.
Sally earned a prestigious Fellowship in Cancer Education from the Cancer Research Campaign. In this role, she promoted the transmission of cancer information to the general public and to medical students.
Sadly, in 1999 Sally was diagnosed with a widespread cancer of the duodenum. She died peacefully at her home with her family around her, as she had wished.
Related links
About cancer research uk's patient and health information.
The history of Cancer Research UK's patient and health information website, how the information is produced and the processes we go through to make sure our information is accurate, up-to-date and engaging.
About cancer homepage
Find out about possible causes of cancer, how cancer starts and grows, tests to diagnose it, and general information about treatments.
It’s a worrying time for many people and we want to be there for you whenever - and wherever - you need us. Cancer Chat is our fully moderated forum where you can talk to others affected by cancer, share experiences, and get support. Cancer Chat is free to join and available 24 hours a day.
Visit the Cancer Chat forum
About Cancer generously supported by Dangoor Education since 2010.

Find a clinical trial
Search our clinical trials database for all cancer trials and studies recruiting in the UK
Cancer Chat forum
Talk to other people affected by cancer
Nurse helpline 0808 800 4040
Questions about cancer? Call freephone 9 to 5 Monday to Friday or email us
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cold Spring Harb Perspect Biol
- v.13(6); 2021 Jun
A History of Cancer Research: Tumor Viruses
Early studies of transmissible tumors in chickens provided evidence that viruses such as avian leukosis virus (ALV) and Rous sarcoma virus (RSV) can cause cancer in these animals. Doubts about the relevance to human tumors and failures to replicate some early work meant the field of tumor virology followed a bumpy course. Nevertheless, viruses that can cause cancers in rodents and humans were ultimately identified, and several Nobel prizes were awarded for work in this area. In this excerpt from his forthcoming book on the history of cancer research, Joe Lipsick looks back at the early history of tumor virus research, from some of the early false starts and debates, to discovery of reverse transcriptase, and identification of human papilloma virus (HPV) as the major cause of cervical cancer.
HERE A CHICK, THERE A CHICK
The early twentieth century witnessed the rise and ignoble fall of Fibiger's Nobel Prize–winning “discovery” of worms as a cause of cancer. But all was not rotten in the state of Denmark. Elsewhere at the University of Copenhagen, Vilhelm Ellerman and Oluf Bang were also testing whether cancer might be an infectious disease. In 1908 they published a paper entitled “Experimental Leukemia in Chickens.” They had found that leukemia, a cancer of the blood cells, could be transmitted from one bird to another by injection ( Fig. 1 ). Furthermore, the causative agent was able to pass through filters too fine to permit passage of any cells, animal or bacterial. Such filterable agents, first discovered in plants, eventually became known as viruses. Ellermann and Bang had discovered avian leukosis virus (ALV), the first known tumor virus. For reasons that remain unclear, their work did not attract the attention it deserved. One criticism was that although one could transmit this leukemia by injection, there was no observable transmission from bird to bird in the absence of injection. Furthermore, not every injected animal developed the disease (∼40%), and those that did often took a while to do so (6–12 mo). There was also a concern that the increased number of white blood cells might be a physiological response to infection, rather than a true malignant proliferation. Finally, it was not then widely accepted that animals, particularly non-mammals, were good models for human disease.

Ellermann and Bang's drawings of normal chicken bone marrow ( left ) and leukemic chicken bone marrow ( right ). The normal marrow contains dense, dark trabeculae of bone. The cells in the spaces between trabeculae are nucleated erythrocytes (red blood cells). The leukemic marrow contains little bone, many immature leukocytes (white blood cells, later shown to be B lymphocytes), and very few erythrocytes. (Reprinted from Ellermann V, Bang O. 1909. Z Hygeine Infektionskrakheiten 63: 231–273.)
Two years after Ellermann and Bang had published their work, Peyton Rous at the Rockefeller Institute described a transmissible sarcoma in chickens ( Fig. 2 ). The original tumor “was found in a barred Plymouth Rock hen of light color and pure blood” that was brought to him by a chicken breeder. Rous minced the tumor into small pieces, injected part into the other breast of the same chicken and part into two other chickens of the same brood. The original chicken died of widespread cancer 35 d later. By this time, one of the other injected chickens had also developed a palpable tumor. In his initial report Rous noted, “The tumor is at best so difficult of propagation that no attempts have been made to determine whether it can be transmitted by cell-fragments, or by cell-free derivatives.”

The origins of Rous sarcoma virus. ( Top ) A sarcoma caused by injection of fragments of the transmissible tumor. ( Bottom ) Histopathologic evidence of a sarcoma invading into muscle. (Reprinted from Rous P. 1910. J Exp Med 12: 696–705.)
However, within a year Rous had found that by passage from chicken to chicken, the transmissible tumor had become increasingly aggressive and was now capable of metastasizing. By 1911 he was able to follow in the footsteps of Bang and Ellermann and transmit this cancer by a filterable agent. This virus eventually became known as Rous sarcoma virus (RSV). As before, the work was not generally accepted as proof that cancer could be caused by an infectious agent. On the contrary, physicians were spending considerable time and effort trying to disabuse the public of the view that human cancer was infectious. This mistaken belief often resulted in the shunning or even the quarantine of patients afflicted with cancer. In search of better career prospects, Rous stopped working on RSV a few short years after publishing his landmark paper in 1911.
Extracts of chicken tumors from Rous's laboratory did make it across the pond to England, only to become entangled in a rather Dickensian tale. It began with an unusual proposition made to a studious railway stationmaster named William Bullock. If Bullock would agree to take a wealthy but childless benefactor's name, he would be left a small fortune with which he could attend medical school. Thus, was he reborn as William Gye. He enrolled at Edinburgh University, pursued a career in cancer research, and eventually was able to repeat the experiments of Rous. Taking things one step further, he then found that he could amplify the infectious material in vitro using fragments of chicken embryos. He also claimed to have isolated similar infectious agents in tumors from mice, from rats, and from humans, all of which could cause tumors in chickens.
Gye then collaborated with J.E. Barnard, a wealthy hatter and amateur microscopist, to obtain what they believed were images of the infectious cancer virus particles. These studies were published in 1925 as back-to-back papers in The Lancet . Not surprisingly, this work attracted wide attention in the popular press, helping to again fuel fears about the infectious nature of human cancer. Ultimately, none of this work stood the test of time, except for Gye's replication of Rous's work on chicken viruses. Gye went on to become a very successful cancer research administrator, eventually serving as the Director of the Imperial Cancer Research Fund Laboratories at Mill Hill.
The field of tumor virology itself also followed a rather bumpy course. Although additional tumor viruses were isolated from chickens in Japan and elsewhere, critics harped on the lack of evidence for similar viruses in mammals. In 1933 Richard Shope at the Rockefeller Institute identified a virus capable of causing papillomas (warts) in rabbits. Rous himself propagated and studied this virus for many years. A few years later John Bittner discovered a transmissible mammary cancer in mice that was caused by a milk-borne virus that became known as mouse mammary tumor virus (MMTV). In the early 1950s, Ludwik Gross identified two more mouse tumor viruses, a murine leukemia virus and a polyoma virus, which caused many different types of cancer. Tumor viruses were then identified in a variety of other mammals, including rats, cats, cows, and monkeys.
An adenovirus isolated from human tissue was shown to cause cancer in rodents in 1962, but was ultimately found not to be a cause of human cancer. Simian vacuolating virus 40 (SV40), a contaminant discovered in cells used to produce polio vaccine, was also shown to cause cancer in rodents in 1962. However, there has been a lack of convincing evidence that SV40 causes human cancer, despite much effort.
Finally, in 1964 Michael Epstein and Yvonne Barr published evidence of the first human tumor virus. They had discovered a herpes-like virus in the lymphoblasts of patients with Burkitt's lymphoma, a cancer endemic in children in tropical Africa. Epstein–Barr virus was later shown to cause both mononucleosis (a benign proliferation of B lymphocytes) and a form of nasopharyngeal cancer endemic in certain regions of China. On the heels of the discovery of the first human tumor virus, Rous was finally awarded the Nobel Prize in Physiology or Medicine in 1966 for his discovery of a chicken sarcoma virus 55 years earlier.
THE HUMAN CONDITION
Rising political pressure in the 1970s caused President Richard Nixon to announce a “war on cancer.” Ironically, much of this pressure came from Mary Lasker, a champion of medical research whose husband Albert Lasker had created advertising campaigns that greatly increased the popularity of cigarettes ( Fig. 3 ). Viruses turned out to be important causes of cancer in domesticated animals, such as chickens, laboratory mice, house cats, and cattle. However, despite the expenditure of much effort and many dollars, viruses were not found to cause the majority of human cancers. There were a number of highly publicized false leads, derisively referred to as “rumor viruses.” These reports were most often a result of contamination of human cells by animal viruses in the laboratory. The Special Virus Cancer Program, a directed medical research effort within the National Cancer Institute (NCI), had been charged with the discovery of new human cancer viruses. The program began in 1964, grew to consume substantial resources, and was eventually discontinued in the late 1970s. In part this was due to criticism from scientists outside the walls of the NCI, who favored peer-reviewed research directed by independent individual investigators rather than a centralized bureaucracy that managed large research contracts.

The Laskers’ contributions to cancer dissemination ( top ) and to political pressure for increasing spending on research for a cancer cure ( bottom , advertisement in The Washington Post ). ( Top , From the collection of Stanford Research Into the Impact of Tobacco Advertising [tobacco.stanford.edu]; bottom , https://profiles.nlm.nih.gov/spotlight/tl/catalog/nlm:nlmuid-101584665X20-doc .)
Eventually other human tumor viruses were discovered. Most of these viruses cause relatively rare types of cancer (e.g., HTLV-I causes lymphoid cancers of the skin; HTLV-II causes a rare form of leukemia; HHV-8 causes Kaposi's sarcoma; MCV causes Merkel cell cancer). One notable exception is a family of human papilloma viruses (HPVs) very similar to those discovered in rabbits by Shope. Two such viruses (HPV16 and HPV18) were shown by Harald zur Hausen in the 1980s to be the major cause of cancer of the uterine cervix in women. HPV also causes head and neck cancers and anogenital cancers. These observations led to a Nobel Prize in Physiology or Medicine for zur Hausen in 2008, and to the creation of preventive HPV vaccines, the first of which was approved by the FDA for clinical use in 2006.
In addition to viruses that appear to directly cause human cancer, certain viruses and other infectious agents appear to cause cancer in part via the response of the host to infection. For example, infection with hepatitis B and C viruses is strongly associated with cancer of the liver, infection with Helicobacter pylori bacteria is strongly associated with cancer of the stomach, and infection with Schistosoma haematobium is strongly associated with bladder cancer in some countries. Hepatitis B virus and H. pylori have been shown to encode proteins that can promote cell proliferation. However, these cancers all appear to require repeated cycles of infection, chronic inflammation, and tissue repair, resulting in the continued proliferation of cells that have also been exposed to environmental carcinogens. The result is an unholy alliance of three old rivals—the irritation theory, the germ theory, and the mutagen theory of cancer.
THE RISE OF THE QUANTS
In the mid-twentieth century, a number of physicists turned their attention from physics to biology. A particularly influential book called What Is Life? by Erwin Schrödinger proposed that genetic information might be contained within a chemical form. This idea spurred a group of physicists-turned-biologists to focus their attention on simpler and simpler genetic systems that could be studied by quantitative methods. The result was the Phage Group led by Max Delbrück, Alfred Hershey, and Salvador Luria. By studying the viruses of bacteria (bacteriophage or phage), they and their colleagues were able to deduce many of the basic principles of molecular biology. A by-product of their efforts was the development of methods for quantitative virology, largely based on the plaque assay first described by Félix d'Hérelle in 1917.
Similar advances in animal virology required the development of methods for studying viruses in systems simpler than a whole animal. In the early twentieth century, Alexis Carrel, a Nobel Prize–winning French surgeon, developed and publicized rather complex and somewhat mystical methods for culturing fragments of tissue in the laboratory. In 1928 Carrel reported that he could use these cultures to propagate RSV. He also claimed to have kept a continuous culture of embryonic chicken heart cells alive for decades in his laboratory at the Rockefeller Institute. His work attracted the attention of Charles “Lucky Lindy” Lindbergh, who with Carrel sought a path to physical immortality ( Fig. 4 ). Eventually Carrel's immortal chicken heart experiments failed to be repeated by others. Most likely, new cells had been continually added via the embryo extracts used to “feed” the cultures. Carrel later returned to Europe, where he became an advocate of eugenics for the Vichy government in Nazi-occupied France, thus sharing sympathies with Lindbergh.

Charles Lindbergh, Alexis Carrel, and the quest for immortality. (Image from the National Portrait Gallery.)
The fields of animal cell culture and animal virology progressed slowly until the 1940s, when recurrent polio epidemics spurred intense interest in animal (including human) virology. In 1948, John Enders and his colleagues succeeded in propagating poliovirus in cultures of human embryonic tissue fragments. Their work led to the intensely competitive development of polio vaccines by Jonas Salk and Albert Sabin. Based on the work of Enders, in 1954 Renato Delbecco and Marguerite Vogt developed a plaque assay for poliovirus that was similar to the method used to study the viruses that had lysed bacteria. At the same time, Harry Eagle at the National Institutes of Health (NIH) was systematically determining the requirements for animal cell growth. The result was a defined medium that, when supplemented with relatively small amounts of animal serum, permitted the reproducible growth of animal cells in culture without the need for embryo extracts or plasma clots. Together these powerful methods were then applied to the quantitative study and isolation of mutants of an ever-increasing number of animal viruses, including other important human pathogens like influenza.
But what about tumor viruses? How could one study viruses that caused cells to proliferate rather than die? The key insight came from Howard Temin and Harry Rubin, a graduate student and a postdoctoral fellow working in Dulbecco's laboratory. They infected dishes of adherent fibroblasts from chicken embryos with different dilutions of RSV, layered agar over the cultures, and then watched and waited. Following infection with very dilute stocks of virus, distinct patches of transformed cells appeared ( Fig. 5 ). Normal fibroblasts are flat, spindly cells that stop proliferating once they touch one another (contact inhibition). By contrast, RSV-transformed fibroblasts round up and keep proliferating, eventually forming small mounds of cells (transformed foci) that are very refractile when seen through a phase-contrast microscope. The agar overlay was an important modification of the method described two years earlier by Manaker and Groupé, because it greatly decreased secondary foci caused by subsequent rounds of infection or by detachment and diffusion of transformed cells. Once again using the logic of the Phage School, Temin and Rubin were able to rapidly and readily quantitate stocks of a tumor virus in a far easier fashion than had been possible with assays in whole animals or chicken eggs. Temin and Rubin observed a linear relationship between the concentration of the virus and the number of foci that extended over a thousandfold range. These results implied that infection with a single viral particle was sufficient to cause the oncogenic transformation of a normal cell. Therefore, by isolating virus from a single focus formed at a low concentration of virus, one could isolate a biological clone that had arisen from a single virus particle.

Temin and Rubin's focus assay for morphologic transformation by Rous sarcoma virus. ( Left ) Experimental scheme. ( Center ) A transformed focus visualized by phase contrast microscopy. ( Right ) Relationship between viral concentration and number of foci. ( Center and right panels from Temin H, Rubin H. 1958. Virology 6: 669–688, with permission from Elsevier.)
PROVIRAL HERESY
Temin continued these studies in his own laboratory. He noticed that some isolates of RSV transformed cells with a cobblestone-like morphology (round), whereas other isolates of RSV transformed cells with a spindly morphology (fusiform) ( Fig. 6 ). Remarkably, these characteristics bred true. Cells transformed by a “round” variant of RSV and the progeny of these cells remained “round,” as did naive cells transformed by viruses isolated from “round” cells. Similarly, cells transformed by the “fusiform” variant of RSV and the progeny of those cells remained “fusiform,” as did naive cells transformed by viruses isolated from “fusiform” cells. Furthermore, the conversion of one viral variant into another occurred very rarely, if ever. These observations led Temin to propose that the transformed state was a stably inherited property of the infected cells. To account for this heritable state, he further proposed that the genetic material of the virus somehow became part of the genetic material of the cell.

Cells transformed by fusiform (f) variant and round (r) morphological variants of Rous sarcoma virus. (Photomicrograph by Peter Vogt from Coffin J, et al. 1997. Retroviruses . Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY, with permission from Peter Vogt.)
There were precedents for viral integration into the host genome in the world of bacteriophage biology. In the 1920s, Eugene and Elizabeth Wollman at the Institut Pasteur in Paris had discovered a latent form of bacteriophage that did not cause cells to lyse. Sadly, the Wollmans were deported from France and perished in Auschwitz. After the end of World War II, their former colleague Andre Lwoff continued their work. By 1949 he had shown that some bacteriophage could exist stably within bacteria in a nonlytic (lysogenic) state. This latent form of the virus (prophage) could be inherited during bacterial division and later be re-activated to produce virus in the absence of any additional infection. Careful studies eventually showed that lysogenic bacteriophage DNA becomes integrated into the genomic DNA of infected bacteria. Much of this latter work was done by François Jacob and by Elie Wollman, the surviving son of Eugene and Elizabeth.
Temin was reportedly unaware of this work because Delbrück (with whom Elie Wollman had trained) and his colleagues at Caltech did not believe in lysogeny. However, by 1962 Vogt and Dulbecco had provided evidence via nucleic acid hybridization that polyoma, a lytic DNA tumor virus originally discovered in mice, was retained in a nonlytic form in oncogenically transformed hamster cells. Soon thereafter, Temin presented similar evidence for the incorporation of the RSV genome into infected cells, although others questioned his results. Temin's proposal that RSV becomes integrated into the DNA of an infected chicken cell genome as a provirus was met with intense skepticism for another reason.
The genome of RSV was known to be composed of RNA, not DNA. Studies of other viruses like polio and influenza had provided examples of RNA serving as a template for the production of more RNA. However, it was generally believed that the flow of information from DNA to RNA to protein was unidirectional. Temin's provirus hypothesis required the heretical conversion of viral RNA into DNA prior to integration and stable inheritance as part of host cell genomic DNA. Temin used inhibitors of DNA synthesis, RNA transcription from DNA, and protein synthesis to obtain evidence consistent with his hypothesis. Viral infection required DNA synthesis, but not protein synthesis. By contrast, viral production by infected cells required RNA synthesis but not DNA synthesis ( Fig. 7 ). Further evidence for a DNA intermediate in viral replication was provided in 1970 by the experiments of David Boettiger in the Temin laboratory. He showed that incorporation of 5-bromodeoxyuridine, a thymidine analog, into the virus caused it to become sensitive to inactivation by ultraviolet light. Similar experiments were also reported by Piero Balduzzi, John Bader, and Herbert Morgan.

Experimental evidence for Temin's provirus hypothesis. Viral infection was prevented by inhibitors of DNA synthesis, but not inhibitors of protein synthesis. By contrast, virus production was prevented by an inhibitor of RNA transcription (actinomycin D), but not by inhibitors of DNA synthesis. (Reprinted from Temin H. 1972. Proc Natl Acad Sci 69: 1016–1020.)
Meanwhile, the criticism had been fierce and unrelenting. Michael Bishop, who would eventually propose his own controversial hypothesis about RSV, described his first encounter with Howard Temin at a scientific meeting in 1968 as follows:
The hypothesis had earned him little but ridicule and grief. So that summer evening, I watched with interest (and from a respectful distance) as Howard argued long into the night with skeptics and detractors. It was my first experience with a scientist who was essentially alone in his beliefs. What I witnessed was a lesson for a lifetime. The opposition to the provirus hypothesis that evening was strong, even vitriolic. In response, Howard was unfailingly patient and reasoned. He had no doubt that his hypothesis was correct, but he was open to constructive criticism, and he painstakingly tried to refute each opposing argument, even those that had no force other than their animus.
Eventually Temin proved to be right. In 1970 he and Satoshi Mizutani reported the existence of an enzyme within detergent-disrupted RSV virions that could indeed convert RNA into DNA. An RNA-dependent DNA polymerase was independently discovered in a murine leukemia virus by David Baltimore, a virologist who had also trained with Renato Dulbecco and was studying the mechanisms of replication of different types of animal viruses. The result was a scientific earthquake, similar in magnitude to that of New Madrid in 1812, which was said to have caused the Mississippi River to run backward. Because of the unprecedented reversal of flow of genetic information from RNA to DNA, this new viral enzyme became known as “reverse transcriptase.” The RNA tumor viruses that encode this enzyme became known as “retroviruses.”
Physical proof of the existence of a DNA provirus came shortly thereafter. Jan Svoboda, a talented virologist, had persisted in studying the biology of RSV behind the Iron Curtain in what was then Czechoslovakia. In the early 1960s he and his colleagues had been able to transform rat fibroblasts by coculture with RSV-infected chicken cells. However, the rat cells themselves were unable to produce infectious RSV unless fused to normal chicken cells. Although these findings supported the provirus theory, Temin himself remained skeptical of this evidence. In 1972, using the same methods and logic by which Oswald Avery and colleagues had first shown that DNA was the genetic material of bacteria, Miroslav Hill and Jana Hillova sealed the deal. They showed that purified genomic DNA from rat cells transformed by RSV could be introduced into uninfected chicken cells, resulting in the production of infectious RSV.
In 1975, Temin and Baltimore received a Nobel Prize in Physiology or Medicine for the discovery of reverse transcriptase, a prize they shared with their mentor Renato Dulbecco for his (and Marguerite Vogt's) work on polyomavirus. Along with the awarding of a Nobel Prize to Peyton Rous in 1966 for the discovery of RSV, this event prompted Peter Duesburg (a fellow retrovirologist) to quip, “One sick chicken, two Nobel prizes.” But that was hardly the end of the story.
From the forthcoming volume Stalking the Enemy Within: A History of Cancer Research , by Joseph Lipsick
Additional Perspectives on A History of Cancer Research available at www.cshperspectives.org
SUGGESTED READING
The phage school, cell culture, and the birth of quantitative animal virology.
- Dulbecco R, Vogt M. 1954. Plaque formation and isolation of pure lines with poliomyelitis viruses . J Exp Med 99 : 167–182. 10.1084/jem.99.2.167 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eagle H. 1955. Nutrition needs of mammalian cells in tissue culture . Science 122 : 501–514. 10.1126/science.122.3168.501 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Judson HF. 1996. The eighth day of creation: makers of the revolution in biology . Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY. [ Google Scholar ]
- Skloot R. 2010. The immortal life of Henrietta Lacks . Crown/ Random House, New York. [ Google Scholar ]
- Watson JD, Stent GS, Cairns J. 2000. Phage and the origins of molecular biology . Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY. [ Google Scholar ]

The Discovery and Assay of RNA Tumor Viruses
- Coffin JM, Hughes SH, Varmus HE editors. 1997. Retroviruses . Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY. [ PubMed ] [ Google Scholar ]
- Ellermann V, Bang O. 1909. Experimental leukemia in chickens II . Z Hygiene Infektionskrakheiten 63 : 231–272. [English translation available in Some classics in experimental oncology (ed. Shimkin M), NIH Publication No 80-2120 (1980)]. 10.1007/BF02227892 [ CrossRef ] [ Google Scholar ]
- Rous P. 1910. A transmissible avian neoplasm (sarcoma of the common fowl) . J Exp Med 12 : 696–705. 10.1084/jem.12.5.696 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rous P. 1911. Transmission of a malignant growth by means of a cell-free filtrate . J Am Med Assoc 56 : 198. [ Google Scholar ]
- Temin HM, Rubin H. 1958. Characteristics of an assay for Rous sarcoma virus and Rous sarcoma cells in tissue culture . Virology 6 : 669–688. 10.1016/0042-6822(58)90114-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
The Discovery of Reverse Transcriptase
- Baltimore D. 1970. RNA-dependent DNA polymerase in virions of RNA tumour viruses . Nature 226 : 1209–1211. 10.1038/2261209a0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Temin HM, Mizutani S. 1970. RNA-dependent DNA polymerase in virions of Rous sarcoma virus . Nature 226 : 1211–1213. 10.1038/2261211a0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
The Provirus Hypothesis
- Baltimore D. 1995. Thinking about Howard Temin . Genes Dev 9 : 1303–1307. 10.1101/gad.9.11.1303 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cooper GM, Temin RG, Sugden B editors. 1995. The DNA provirus: Howard Temin's scientific legacy . ASM Press, Washington, DC. [ Google Scholar ]
- Hill M, Hillova J. 1972. Virus recovery in chicken cells tested with rous sarcoma cell DNA . Nat New Biol 237 : 35–39. 10.1038/newbio237035a0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Svoboda J. 2008. The turns of life and science . Adv Cancer Research 99 : 1–32. 10.1016/S0065-230X(07)99001-6 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Temin HM. 1976. The DNA provirus hypothesis . Science 192 : 1075–1080. 10.1126/science.58444 [ PubMed ] [ CrossRef ] [ Google Scholar ]
The Search for Human Tumor Viruses
- Epstein MA, Achong BG, Barr YM. 1964. Virus particles in cultured lymphoblasts from Burkitt's lymphoma . Lancet 283 : 702–703. 10.1016/S0140-6736(64)91524-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Javier RT, Butel JS. 2008. The history of tumor virology . Cancer Res 68 : 7693–7706. 10.1158/0008-5472.CAN-08-3301 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moore PS, Chang Y. 2010. Why do viruses cause cancer? Highlights of the first century of human tumour virology . Nat Rev Cancer 10 : 878–889. 10.1038/nrc2961 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wade N. 1971. Special virus cancer program: travails of a biological moonshot . Science 174 : 1306–1311. 10.1126/science.174.4016.1306 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zur Hausen H. 2009. The search for infectious causes of human cancer: where and why? Virology 392 : 1–10. 10.1016/j.virol.2009.06.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is the History of Breast Cancer?
- Ancient to Modern Times
- Notable Scientists
Advancements in Care
- Population Risk
- Family History
Frequently Asked Questions
Cancer is as old as humanity, and breast cancer is a fantastic example of how our thinking about what causes cancer and how to treat it has changed over the centuries .
Medicine has changed greatly since the ancient Egyptians. Even in the last few decades, there’s been a revolution in cancer care, with new treatment types and approaches to even the most tenacious metastatic foe.
This article reviews the history of breast cancer research and developments in caring for breast cancer patients. Read on to learn what’s been discovered about the risk of developing breast cancer and how treatments have changed over the years.
Verywell / Jessica Olah
From Ancient to Modern Times
The first recorded reports of breast cancer and its treatment were discovered on ancient papyrus out of Egypt. The Edwin Smith papyrus is dated 1600 BCE, but was possibly a copy of an older document, maybe as old as 2500 or 3000 BCE.
The papyrus described several cases of tumors growing in the breast and how they were treated using a “fire drill”—a tool that burnt the skin to destroy the cancerous tissue. The text describes the condition as untreatable.
The term cancer wasn’t coined until 400 BCE by Hippocrates, who hypothesized it was an imbalance of humors (blood, phlegm, yellow bile, and black bile).
Starting with Hippocrates’s humors, the road to understanding breast cancer is paved with many ideas which seem odd to modern minds:
- It was thought in ancient times that possibly menopause caused cancer—which makes sense since cancers are more likely to develop as we age.
- In 1680, Francois de la Boe Sylvius hypothesized that the body’s lymphatic fluids turned acidic, leading to cancer.
- Claude-Deshais Gendron built on this lymphatic theory, suggesting that cancers arise when the nerve and glandular tissue are mixed with lymph.
- In 1713, Bernardino Ramazzini hypothesized that nuns developed more breast cancers because of their celibacy. While this seems a little out there, we actually now know that hormonal changes during pregnancy, childbirth, and breastfeeding have a protective effect against breast cancers.
- Breast cancer doesn’t just happen in celibate females, though, so Frederich Hoffman of Prussia suggested that sexually active females who develop breast cancer get this disease because the sex they’re having is “too vigorous” and blocks their lymph from draining.
- Italian physician Giovanni Morgagni blamed curdled milk in the breast for causing cancers, building off hundreds of autopsies of patients.
- Johannes de Gorter proposed pus-filled inflammations as leading to cancer in the breast.
- French surgeon Claude-Nicolas Le Cat suggested that depressive mental disorders led to breast cancer. During the 1750s, he and other surgeons pursued breast cancer surgeries that removed the breast, lymph nodes, and muscles.
Disputed Theories
Unfounded theories into the causes of breast cancer weren’t just popular in ancient times. In more recent decades, several modern conveniences have been named (and disproven) as causes of breast cancer.
People have suggested that antiperspirants, bras, miscarriages, and abortions may play a role in the development of breast cancer. Large modern studies have proven these theories wrong.
Notable Scientists
William Halsted, Johns Hopkins : Building off of the work of surgeons including Le Cat, Halsted developed the radical mastectomy in 1894. This surgery removed not only the breast, but also the underlying muscles and nearby lymph nodes. While disfiguring, this surgery was the most effective treatment for breast cancer for decades to come.
J. Collins Warren, Harvard Medical School : In the 1930s, Warren developed the needle biopsy and started using a frozen sectioning technique to diagnose breast cancer under the microscope. This technique is still used today as a simple, reliable tool to diagnose tumors in the breast.
Sir Geoffrey Keynes, St. Bartholomew’s Hospital in London : In 1937, Keynes described additional therapies, including medical radiation , being used to treat any cancer remaining after breast-sparing surgery.
Robert Egan, University of Texas : In 1962, Egan showed mammograms could detect undiscovered cancers and other breast tumors. This imaging test allows early detection of small breast tumors and helps improve breast cancer surgery. Egan’s studies led to mammography being widely used as a screening tool through the 1960s.
Elwood Jensen, University of Cincinnati : In 1967, Jensen first described finding estrogen and progesterone receptors in breast cancers. These receptors communicate with the body’s hormones and help the cancers grow. The discovery of drugs that block these hormones or their receptors revolutionized breast cancer treatment.
Gianni Bonadonna, Istituto Nazionale dei Tumori : In 1975, Bonadonna was the first to show chemotherapy treatment with cyclophosphamide, methotrexate, and fluorouracil could treat breast cancers—an important shift away from radical surgical approaches to breast cancer treatment.
Hans Holmström, University of Gothenburg : As surgeries for breast cancer became less invasive, Holmström developed new techniques for breast reconstruction , publishing the transverse rectus abdominis myocutaneous (TRAM) flap surgery in 1973.
Dora Richardson and Arthur Walpole, ICI Pharmaceuticals : Chemist Richardson first synthesized the drug Nolvadex (tamoxifen) in 1962 while developing birth control. A research team led by Walpole developed the drug as a breast cancer treatment.
Tamoxifen is a hormone therapy that blocks the action of estrogen in the body, can shrink breast tumors, and increases the survival of breast cancer patients with hormone-reactive tumors. The drug, first launched in the UK in 1973 and approved by the Food and Drug Administration (FDA) in 1977, changed breast cancer treatment.
Robert Weinberg Lab, Massachusetts Institute of Technology : This team discovered the HER2 gene in the early 1980s. Between 20% and 25% of breast cancers over-express this gene, leading to aggressive disease and worse outcomes. This discovery led the way to understanding that several distinct subclasses of breast cancer react to treatments in specific ways. Understanding the genetics of any given tumor has helped doctors treat individual patients in personalized ways.
Bernard Fischer, University of Pittsburgh : Fisher’s study, the National Surgical Adjuvant Breast and Bowel Project, was published in 1989. It scientifically compared different treatments for breast cancer. The results provided scientific support that combining surgery, chemotherapy, and radiation lengthened life in breast cancer patients, even those with advanced cancers.
Mary-Claire King, UC Berkeley : In the 1990s, King’s group discovered the BRCA1 mutation , linked to a hereditary disease that increases a person’s risk of developing breast, ovarian, and other cancers. Her work on hereditary breast cancers reinforced the importance of genetics on cancer development. BRCA1 and BRCA2 were cloned by a team led by Mark Skolnick at Myriad Genetics in the mid-1990s.
Chemotherapy
Starting in the 1970s, the first drugs were developed as cancer treatments. These chemotherapies, including Adriamycin (doxorubicin) , killed any fast-growing cells in the body and therefore had side effects. Other notable chemotherapies include Taxol (paclitaxel), released in 1994, and Xeloda (capecitabine) , released in 1998.
Hormonal Therapy
Later in the 1970s, hormonal therapies , including tamoxifen, showed promise for treating breast cancers and eventually keeping them in check after remission.
In 1996 another hormone therapy, Arimidex (anastrozole), was used successfully to treat estrogen receptor-positive advanced breast cancer in postmenopausal females. Anastrozole was the first aromatase inhibitor (a drug that blocks estrogen production in the body) to be approved for cancer therapy.
The 1980s saw improvements in surgery options for people with breast cancer. In 1985, surgeons developed breast-conserving surgery, also called a lumpectomy .
Instead of removing the entire breast, the lumpectomy aims to remove just the cancerous tissue. It’s often used alongside radiation and chemotherapies with similar rates of overall and disease-free survival.
Biologics and Targeted Therapy
In the 1990s, biologics for breast cancer entered the treatment scene. These drugs are actually antibodies, very similar to the antibodies your immune system makes naturally. Antibodies are very specific to the target they are created against, so they tell the body to attack cancer cells without hurting other cells.
Released in 1998, Herceptin (trastuzumab) is a biologic that targets cancer cells that over-express the HER2 gene. It is used to treat females with HER2-positive metastatic breast cancer . In 2013, improvements to the original drug were released as Kadcyla (also known as ado-trastuzumab emtansine or T-DM1), an antibody linked to a drug that can kill cancer cells.
Other important improvements in targeted therapies in the last few years have played an important role in improving breast cancer survival.
In 2019 a new therapy targeted against the PIK3CA mutation was approved by the FDA. Between 30% and 40% of breast cancer patients have a mutation in the PIK3CA gene. The drug Piqray (alpelisib) can slow the growth of advanced hormone receptor-positive and HER2-negative (HR+/HER2-) breast cancers and improve progression-free survival.
Another new target for breast cancer therapies is cyclin-dependent kinases. These are important for cell growth, so inhibiting them can slow the progression of HR+/HER2- advanced breast cancers. Drugs that act against this target include Ibrance (palbociclib) and Kisqali (ribociclib), both of which are given alongside hormone therapies.
A third new target for breast cancer treatment is the enzyme PARP, which normally acts to help repair damaged genes. Blocking this repair mechanism can help kill cancer cells that have BRCA mutations because their genes have too many mistakes to keep functioning.
Targeted therapies including Lynparza (olaparib), Rubraca (rucaparib), Zejula (niraparib), and Talzenna (talazoparib) are all important new treatments for BRCA-positive breast cancers.
Genetic Profiles
The most recent advancements in breast cancer treatment involve the implementation of genetic information to the personalization of breast cancer treatment. An article published in the journal Nature in 2000 changed the game on cancer genetics by creating “molecular portraits” of breast cancer.
The researchers found specific genes expressed by cancer cells that give doctors a better idea of if cancer will come back after treatment. These gene profiles were developed into tests that doctors can use to help guide treatment decisions and are even used in breast cancer staging.
One of the biggest advancements in breast cancer treatment has been using genetic information to make treatment decisions—not only in determining the potential recurrence of cancer, but also in determining what treatments might work best against any given cancer.
By analyzing the genetic attributes of a person’s cancer, doctors can separate patients into multiple breast cancer subtypes. Breast cancer is no longer considered one disease but rather a mixture of at least four diseases:
- Hormone receptor-positive and HER2-negative cancer
- Hormone receptor-positive and HER2-positive cancer
- Hormone receptor-negative and HER2-positive cancer
- Triple-negative cancer
Different treatments are useful for each of these cancer subtypes. For example, for hormone therapy to work, the cancer cells need to be hormone receptor-positive. For HER2-targeted therapies to work, the patient’s cancer needs to be expressing higher-than-normal levels of the HER2 protein.
Altogether, our understanding of breast cancer and the best approaches for treating it have improved greatly, even to the point where some patients with advanced cancers no longer need chemotherapy.
Advancements in Identifying Population Risk
In addition to the impact of genetic analysis on breast cancer treatment, another significant advancement in breast cancer care is identifying specific groups at high risk of developing breast cancers or that are more at risk of dying from them.
Ensuring that these groups have adequate access to and guidelines for screening and other preventative measures is important in helping improve breast cancer survival rates and care.
An American Cancer Society report from 2017 indicated that while breast cancer survival is up, Black females are 42% more likely to die from breast cancer than White females.
Breast cancer rates have also been rising in Asian American females for multiple decades. Specifically, immigrant Asian American females have about a three times higher risk of developing breast cancer than Asian American females who lived more than half their lives in the United States.
Certain ethnicities, including Ashkenazi Jewish, are at a higher risk of carrying inherited breast cancer genes, like the BRCA1 and BRCA2 mutations. Researchers estimate that one in 40 individuals of this population carries a BRCA mutation.
The medical community has also been learning more about males who get breast cancer. Typically one in 1,000 males will be diagnosed with breast cancer. These cancers are typically diagnosed at a more advanced stage and have fewer effective treatment options. Males with the BRCA mutations are at a higher risk of developing breast and several other cancers.
Having a Family History of Breast Cancer
Multiple genes, including the BRCA genes, can cause inherited breast cancers to run in families.
The BRCA mutations are the best known and increase the risk of developing breast, ovarian, and other cancers. But this risk can be mitigated to an extent with lifestyle changes, preventative surgeries and therapies, regular checkups, and screening scans for cancer development.
It also isn’t a given that you’ll develop breast or another cancer just because you have a BRCA mutation, another inherited cancer syndrome, or a family history of breast cancer.
Having a family history of breast cancer means some of your blood relatives have had breast cancer. If that relative is closely related, like a mother or sister, or developed breast cancer before 50, there may be more reason to suspect a genetic link.
But this doesn’t mean that you will necessarily have breast cancer or that you have a genetic variant that’s likely to increase your risk. A family history of breast cancer is just a signal to your doctor that this may be worth watching or testing.
Only about 10% of breast cancer patients have a family history of the disease, so it’s not as telling of an indicator as you might think.
Breast cancer has a long and winding history. Ancient Egyptians documented the condition, but it was considered incurable. Surgery was developed as a treatment in the 1700s and refined in the late 1800s. In the 1930s and following decades, radiation therapy and chemotherapy were developed, along with diagnostic techniques.
Major advancements have disrupted how we manage and treat this cancer over the last several decades. These include hormonal therapy, targeted therapy, and genetic profiling.
These days, breast cancer has a high five-year survival rate and effective treatment options because of years of research into new drugs, new surgeries, and new approaches to diagnosing and understanding breast cancer.
A Word From Verywell
One thing is for sure when you’re researching breast cancer treatments: You’re not alone. More than a quarter of a million females are diagnosed with breast cancer every year in the United States.
The sheer volume of breast cancer patients means that even hard-to-treat breast cancers are continually reaping the benefits of research advancements and ongoing clinical trials.
Breast cancer has paved the way for researchers to understand other types of cancers and how best to treat them. New types of drugs and diagnostics can help improve outcomes.
The radical mastectomy was developed in the late 1800s by William Halsted, but the first surgery to remove an entire cancerous breast probably happened before then.
There’s no way to know who the first person to discover breast cancer might have been, but the oldest description of breast cancer found comes from the ancient Egyptians. The surgical papyrus, a medical text that may date back to 3000-2500 BCE, describes cases of breast cancer.
There is no way to determine when the first known case of breast cancer occurred. Breast cancer and other cancers are likely as ancient as humanity. The earliest descriptions of breast cancer were published in the surgical papyrus of the ancient Egyptians, a medical text that dates back to 3000-2500 BCE.
The first real curative treatments for breast cancer were extensive surgeries pioneered during the 1880s and improved throughout the 1900s. Over the years, newly developed ways of treating breast cancer have allowed doctors to scale back the extent and use of breast removal surgeries.
Starting around the 1930s, radiation was developed as a breast cancer treatment. Chemotherapy became popular in the 1970s, and soon hormonal treatments were also being used to effectively treat breast cancer.
The first biologics to treat breast cancer arrived on the scene in the 1990s, and now genetic analysis of breast cancers is driving a personalized medicine revolution that has made staging and treatment of cancers more complex, but more effective.
Ades F, Tryfonidis K, Zardavas D. The past and future of breast cancer treatment—from the papyrus to individualised treatment approaches . ecancer . 2017;11:746. doi:10.3332/ecancer.2017.746
Lakhtakia R. A brief history of breast cancer: part I — surgical domination reinvented . Sultan Qaboos Univ Med J . 14(2):e166-e169.
American Cancer Society. Understanding what cancer is: ancient times to present .
Lukong KE. Understanding breast cancer — the long and winding road . BBA Clin . 2017;7:64-77. doi:10.1016/j.bbacli.2017.01.001
American Cancer Society. History of cancer epidemiology: 18th century to present .
Maurer Foundation. A brief history of breast cancer .
American Cancer Society. Disproven or controversial breast cancer risk factors .
National Cancer Institute. Milestones in cancer research and discovery .
Young RH, Louis DN. The Warrens and other pioneering clinician pathologists of the Massachusetts General Hospital during its early years: an appreciation on the 200th anniversary of the hospital founding . Mod Pathol . 2011;24(10):1285-1294. doi:10.1038/modpathol.2011.132
Lakhtakia R, Chinoy RF. A brief history of breast cancer: part II — evolution of surgical pathology . Sultan Qaboos Univ Med J . 14(3):e319-e322.
Egan RL. Mammography, an aid to diagnosis of breast carcinoma . JAMA . 1962;182(8):839-843. doi:10.1001/jama.1962.03050470017004
Holmström H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report . Scand J Plast Reconstr Surg . 1979;13(3):423-427. doi:10.3109/02844317909013092
Quirke VM. Tamoxifen from failed contraceptive pill to best-selling breast cancer medicine: a case-study in pharmaceutical innovation . Front Pharmacol . 2017;8:620. doi:10.3389/fphar.2017.00620
Food and Drug Administration. Highlights of prescribing information — Soltamox .
Lakhtakia R, Burney I. A brief history of breast cancer: part III — tumour biology lays the foundation for medical oncology . Sultan Qaboos Univ Med J . 15(1):e34-e38.
Hurst JH. Pioneering geneticist Mary-Claire King receives the 2014 Lasker~Koshland Special Achievement Award in Medical Science . J Clin Invest . 2014;124(10):4148-4151. doi:10.1172/JCI78507
American Cancer Society. Targeted drug therapy for breast cancer .
American Cancer Society. FDA approves first PI3K inhibitor for breast cancer .
Perou CM, Sørlie T, Eisen MB, et al. Molecular portraits of human breast tumours . Nature . 2000;406(6797):747-752. doi:10.1038/35021093
National Cancer Institute. Female breast cancer subtypes .
American Cancer Society. Breast cancer facts & figures 2017-2018 .
Morey BN, Gee GC, von Ehrenstein OS, et al. Higher breast cancer risk among immigrant Asian American women than among US-born Asian American women . Prev Chronic Dis . 2019;16:E20. doi:10.5888/pcd16.180221
Tufts Medical Center. History of breast cancer care .
Johns Hopkins Medicine. Family history of breast cancer .
National Breast Cancer Foundation. Myth: if you have a family history of breast cancer, you are likely to develop breast cancer, too .
National Cancer Institute. Female breast cancer — cancer stat facts .
By Jennifer Welsh Jennifer Welsh is a Connecticut-based science writer and editor with over ten years of experience under her belt. She’s previously worked and written for WIRED Science, The Scientist, Discover Magazine, LiveScience, and Business Insider.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 27 March 2024
How does a cancer vaccine work?
- Liam Drew 0
Liam Drew is a freelance writer based near London, UK.
You can also search for this author in PubMed Google Scholar
Vaccines are usually used to prevent infectious diseases. A therapeutic cancer vaccine is different. Rather than teaching the immune system to recognize pathogens in advance of an infection, these vaccines use identifying proteins produced by cancer cells, known as antigens, to provoke a powerful immune response to existing tumours.
A variety of approaches
The first step is to deliver antigens to immune cells called dendritic cells. These present antigens to other immune cells, and stimulate a response. In the past decade, several approaches have emerged 1 . One delivers antigens that are shared by many people with the same type of cancer ( 2 ). Others, including those that make use of messenger RNA (mRNA) technology, are highly personalized to the unique neoantigens produced by an individual’s tumour ( 3 ). Other personalized approaches involve injecting dendritic cells that are pre-loaded with cancer antigens ( 1 ), or generating antigens inside the body and promoting their uptake by dendritic cells in situ ( 4 ).
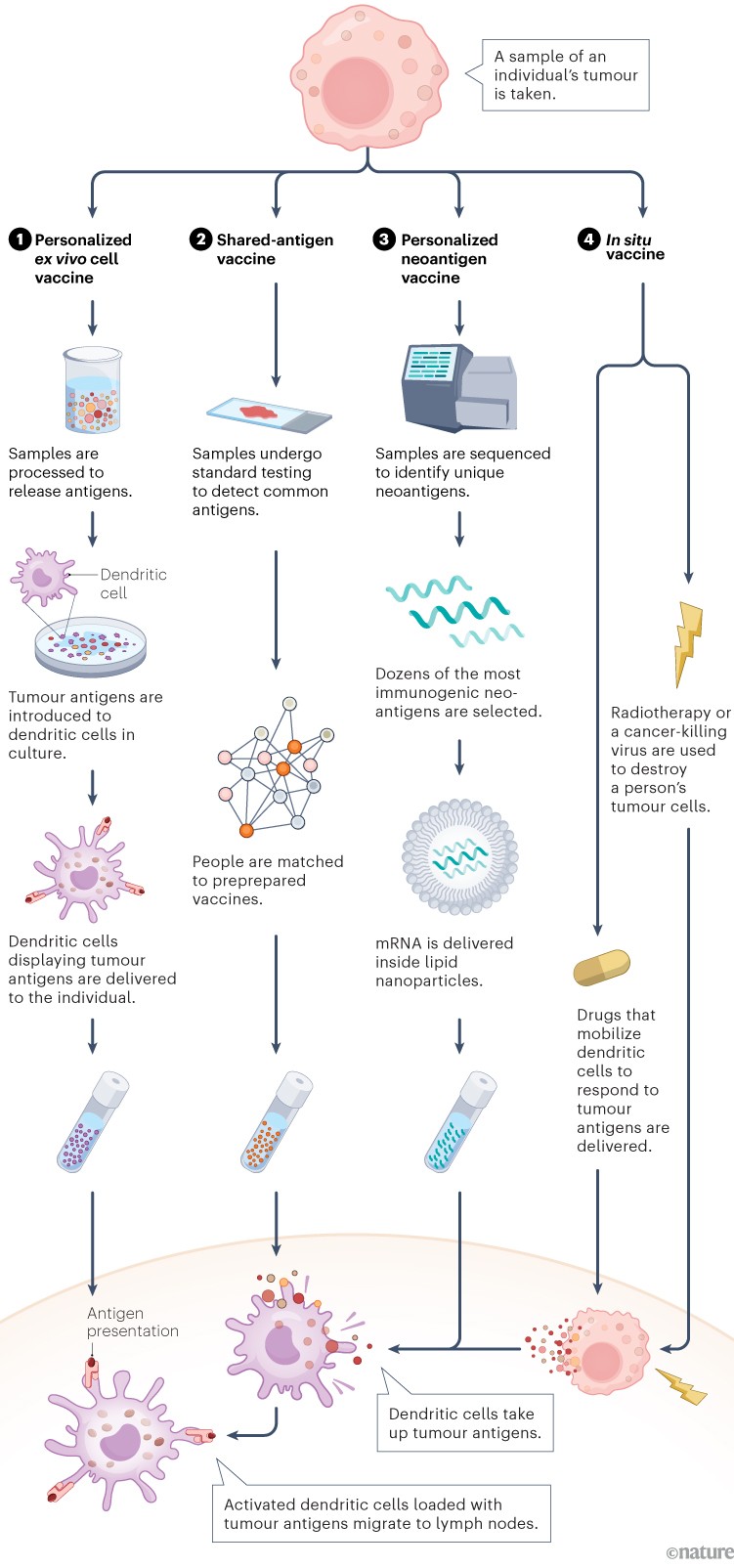
Infographic: Alisdair Macdonald
Mounting a response
Unlike preventive vaccines, which focus mainly on activating antibody-producing B cells, a therapeutic cancer vaccine must generate a strong T-cell response. Dendritic cells loaded with tumour antigens bind and activate CD8 + cytotoxic T cells, which can then mount an attack on the tumour 2 .
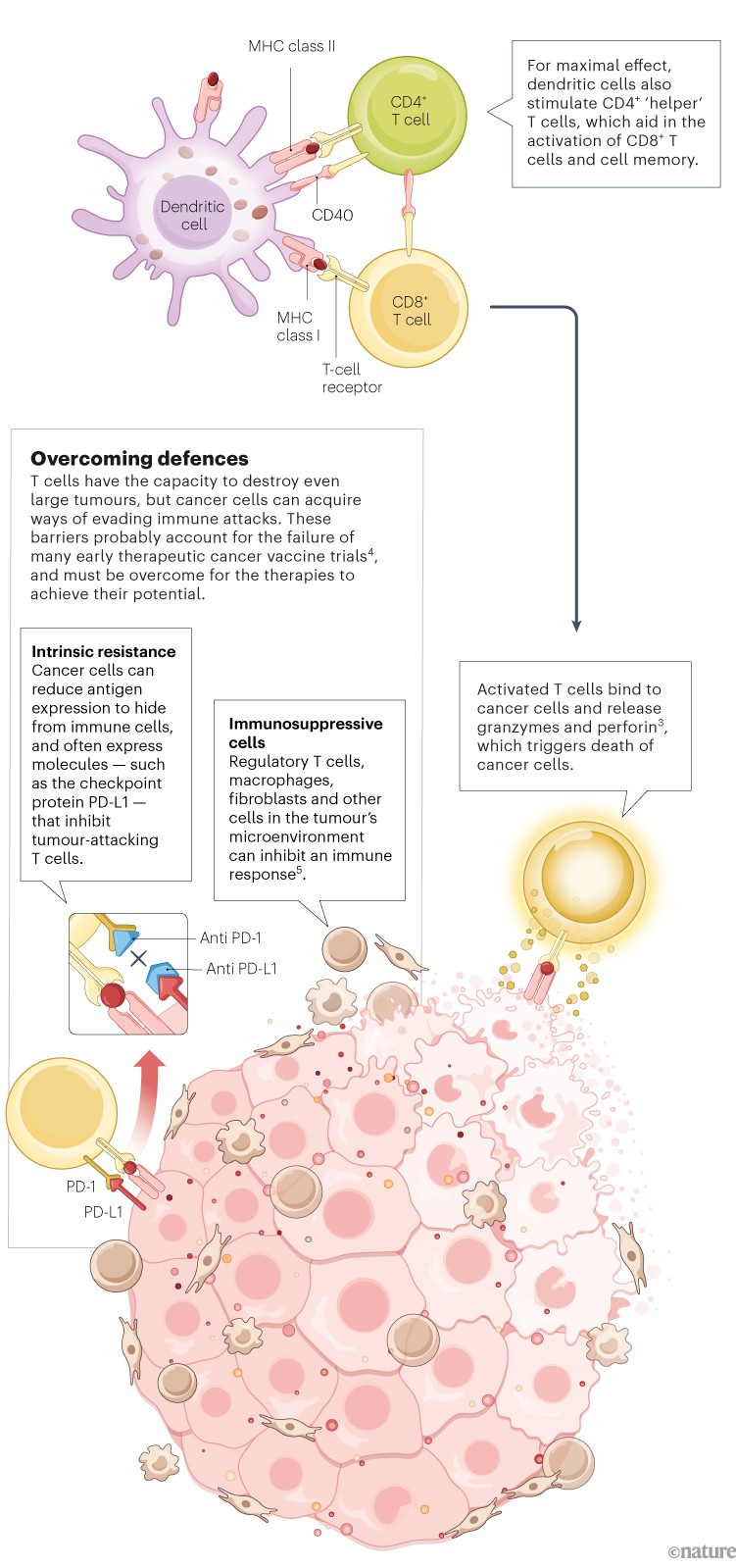
Promising results
Numerous therapeutic cancer vaccines, on the basis of a variety of approaches, are showing encouraging results in trials.
Pancreatic cancer: In a phase I trial of a personalized mRNA vaccine, half of the participants developed T cells targeted to cancer neoantigens 6 . Recurrence-free survival in this group was longer compared with those who did not respond.
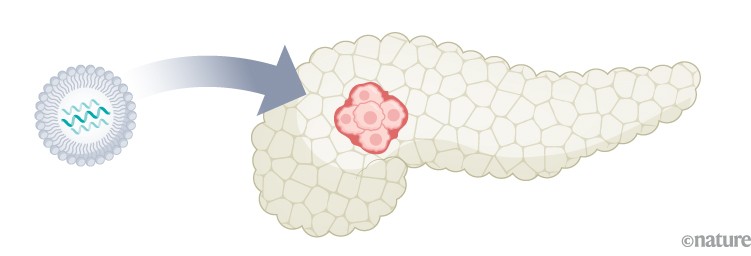
Melanoma: A phase II trial of a personalized mRNA vaccine showed a 44% decrease in the risk of post-surgical recurrence or death 7 . A phase III trial is under way, with final results expected in 2029.
Lymphoma: A phase I/II trial of an in situ vaccine that combined radiotherapy with signalling molecules that mobilize and activate dendritic cells showed evidence of tumour regression in 8 of 11 people who were treated 1 .

Obstacles ahead
The future development and the clinical uptake of therapeutic cancer vaccines will be shaped by several factors.

Unwieldy trials. Testing multiple combinations of agents makes clinical trials more complex. Another complicating factor is timing when to give a vaccine relative to other interventions, such as surgery.
Immunity monitoring. Tracking acquired immunity is important for assessing vaccine efficacy. For cancer vaccines, new T-cell monitoring techniques are needed.
Scalability. Personalized cancer vaccines could pose logistical challenges. Streamlining production will be essential to keep costs down and availability high.
Nature 627 , S34-S35 (2024)
doi: https://doi.org/10.1038/d41586-024-00841-y
This article is part of Nature Outline: Cancer vaccines , a supplement produced with the financial support from Moderna . Nature maintains full independence in all editorial decisions related to the content. About this content .
Lin, M. J. et al. Nature Cancer 3 , 911–926 (2022).
Article PubMed Google Scholar
Laidlaw, B. J., Craft, J. E. & Kaech, S. M. Nature Rev. Immunol. 16 , 102–111 (2016).
Waldman, A. D., Fritz, J. M. & Lenardo, M. J. Nature Rev. Immunol. 20 , 651–668 (2020).
Saxena, M. et al. Nature Rev. Cancer 21 , 360–378 (2021).
Sellars, M. C., Wu, C. J. & Fritsch, E. F. Cell 185 , 2770–2788 (2022).
Rojas, L. A. et al. Nature 618 , 144–150 (2023).
Carvalho, T. Nature Med. 29 , 2379–2380 (2023).
Download references
Related Articles

Sponsor feature: Revolutionizing cancer research with the power of mRNA
- Personalized medicine

Video: Cancer-busting vaccines
Outline 27 MAR 24

Cancer-vaccine trials give reasons for optimism

TRBC1-targeting antibody–drug conjugates for the treatment of T cell cancers
Article 27 MAR 24

Mobile delivery of COVID-19 vaccines improved uptake in rural Sierra Leone
News & Views 13 MAR 24

Ambitious survey of human diversity yields millions of undiscovered genetic variants
News 19 FEB 24
Postdoctoral Fellowships-Metabolic control of cell growth and senescence
Postdoctoral positions in the team Cell growth control by nutrients at Inst. Necker, Université Paris Cité, Inserm, Paris, France.
Paris, Ile-de-France (FR)
Inserm DR IDF Paris Centre Nord
Zhejiang Provincial Hospital of Chinese Medicine on Open Recruitment of Medical Talents and Postdocs
Director of Clinical Department, Professor, Researcher, Post-doctor
Hangzhou, Zhejiang, China
The First Affiliated Hospital of Zhejiang Chinese Medical University
Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Warmly Welcomes Talents Abroad
“Qiushi” Distinguished Scholar, Zhejiang University, including Professor and Physician
No. 3, Qingchun East Road, Hangzhou, Zhejiang (CN)
Sir Run Run Shaw Hospital Affiliated with Zhejiang University School of Medicine
Global Faculty Recruitment of School of Life Sciences, Tsinghua University
The School of Life Sciences at Tsinghua University invites applications for tenure-track or tenured faculty positions at all ranks (Assistant/Ass...
Beijing, China
Tsinghua University (The School of Life Sciences)
Faculty Positions at Great Bay University, China
We are now seeking outstanding candidates in Physics, Chemistry and Physical Sciences.
Dongguan, Guangdong, China
Great Bay University, China (GBU)
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
What to Know About Rising Rates of 'Early-Onset' Cancer
BY KATHY KATELLA March 4, 2024

Many people think of the first few decades of adulthood as a time of exploration—to focus on a career, make new friends (or even find a spouse), travel the world, or just have fun. Whichever path they choose, the last thing on their mind is cancer. But cancer is occurring in more adults at younger ages—before they turn 40 or 50 and sometimes even earlier.
These are called “early-onset” cancers, which are diagnosed in adults between the ages of 18 and 49. Because advancing age is the top risk factor for cancer in general, the recent rise in early-onset cancers is worrisome.
Many individuals in this age group are too young for recommended routine cancer screenings—for example, mammography screening typically starts at age 40 and colonoscopies at age 45. And busy lives make it difficult to keep up with routine primary care visits, where family history might prompt a doctor to suggest an earlier screening. Others may not go to the doctor because they have limited or no health insurance—or they believe their health problems are not serious enough to warrant a visit. This can result in diagnosis delays, which raise the risk of cancer potentially being diagnosed at a more advanced stage, which may be harder to treat.
Why are younger people getting cancer? “It's such an important question, and it points to the need for more research in all kinds of domains—in population science, behavioral health, public health, and basic science as well,” says Veda Giri, MD , a Yale Medicine medical oncologist and director of Yale Cancer Center’s Early-Onset Cancer Program at Smilow Cancer Hospital , which brings together such components as research, clinical services, and care from psycho-oncologic specialists, including psychiatrists and social workers.
“So, right now, we are focusing on recognizing that early-onset cancer is a different type of cancer and providing more support for these younger patients,” Dr. Giri says.
Below, Yale Medicine specialists who care for patients with early-onset cancer answer questions about the uptick in diagnoses and the importance of family history.
How are early-onset cancers different from other types of cancer?
Age itself is the first and obvious difference. “Early-onset” can be defined in various ways based on the cancer type. “For example, early-onset breast cancer refers to a diagnosis in someone younger than age 45, while early-onset colorectal cancer is a diagnosis that occurs in someone younger than 50,” says Dr. Giri. “To be as inclusive as possible, the Early-Onset Cancer Program at Yale is addressing the needs of patients diagnosed with cancer between the ages of 18 and 49.”
At age 50, cell damage begins to build up in the body, and the rate of cancer incidence climbs steeply through the following decades. A cancer diagnosis before age 50 is not uncommon, but it’s also not the trajectory most people expect, considering the median age for a cancer diagnosis is 66 years old.
Another difference is that certain cancers, such as breast cancer, tend to be more aggressive in younger adults, says Yale Medicine’s Mariya Rozenblit, MD , a medical oncologist.
“While older women are more likely to be diagnosed with slow-growing, estrogen-positive tumors, younger women have more triple-negative and human epidermal growth factor receptor 2 [HER2] breast cancers, which are more aggressive types,” Dr. Rozenblit says. The latter cancers often require more aggressive treatments, especially if the cancer is already spreading in the body, and those treatments can have significant side effects, she adds.
“Younger women diagnosed with breast cancer are also more likely to have a genetic mutation than older women,” says Dr. Rozenblit. But she cautions that while genetics are getting more attention, mutations like BRCA only account for about 20% of early-onset breast cancers. “So, there are clearly other contributing factors that we don’t yet know,” she says. “The good news is that once breast cancer is diagnosed, the prognosis is usually very good. The treatments can be long, but we still have very high cure rates, and these younger women often end up doing extremely well.”
Jeremy Kortmansky, MD , a Yale Medicine medical oncologist specializing in gastrointestinal cancers , also sees differences when younger adults are diagnosed with colorectal cancer. “Some of the molecular characteristics and pathways of how something becomes cancerous are different between the older and younger groups,” he says. “Younger adults tend to have a more aggressive-appearing cancer. They also tend to present at a more advanced stage that is not solely explained by a delay in diagnosis.”
Some of this may be explained by the fact that they are too young for routine screening, but there's probably more to the story. We just don’t have answers yet, he adds.
What types of cancers are on the rise in younger adults?
While some cancers have been declining in older people, various reports and studies have shown that cancer is on the rise in younger adults. One of the most recent is Cancer Statistics, 2024 , an American Cancer Society (ACS) annual report on cancer facts and trends. Published in January, the report revealed that while cancer deaths are falling, new cases are ticking upwards—from 1.9 million in 2022 to over 2 million in 2023.
More of those new cases involve younger people. The ACS report showed younger adults to be the only age group with an increase in overall cancer incidence between 1995 and 2020—the rate has risen by 1% to 2% each year during that time period.
The ACS report also showed continued increases in such common cancers as breast, prostate , and endometrial in young adults, as well as colorectal and cervical cancers. Colorectal cancer, while still overwhelmingly a disease that affects older people, is now the leading cause of cancer death in men younger than 50 and second in women in that age group. The numbers have been rising steadily in people 55 and younger since the mid-1990s, according to the ACS.
As for cervical cancer, the ACS report had both good and bad news. Rates of cervical cancer dropped significantly in women in their 20s, who were among the first to get the human papillomavirus (HPV) vaccine , which can prevent more than 90% of HPV-attributable cancers . But for women ages 30 to 44, rates rose 1.7% each year from 2012 through 2019. The increase highlights the need for more screening in younger women and a broader uptake for the vaccine, according to the ACS report.
How can family history help adults who are too young for routine screenings?
Because doctors and researchers don’t yet know why early-onset cancers are increasing, they are focusing on efforts to diagnose these cancers early, when they are typically more treatable. And family history has emerged as a key factor in early diagnosis.
This is partly because young adults don’t always meet the recommended age for routine screenings that are available for some of these cancers. For instance, because colonoscopy screening typically starts at age 45, most cases in adults younger than 45 are not identified until they start noticing signs and symptoms.
But talking to a doctor about a family history of colorectal cancer could prompt a screening referral at a younger age. “If there is a family history of either cancer or polyps, we usually start colonoscopy screening 10 to 15 years before the family member who had it was diagnosed,” says Dr. Kortmansky. “So, if a first-degree relative was diagnosed with cancer at 45, you would start screening at 30.”
Likewise, women who are at average risk for breast cancer may start mammography screening at age 40, according to U.S. Preventive Services Task Force (USPTF) recommendations updated in 2023 . But women with a family history of breast cancer are generally advised to start when they are 10 years younger than the first-degree relative (a mother and/or sister) was at their time of diagnosis.
“We’re beginning to recognize that family history is very important,” says Dr. Rozenblit. “For young women who have a significant family history of cancer in the family, we are starting to refer them to a high-risk clinic —even if the cancer in their family is not breast cancer.”
Depending on family history, calculators can be used to further estimate a patient's cancer risk, and advanced screening like MRIs or other diagnostic procedures may be offered, adds Dr. Giri.
“Family history can inform genetic testing to find out whether a person has a mutation that makes them predisposed to developing a certain type of cancer,” she says. “But even if patients test negative for genetic mutations, family history may be a reason to follow them more closely.”
How can early-onset cancer affect a younger adult’s life?
Nancy Borstelmann, PhD, MPH, LCSW , co-director of Yale’s Early-Onset Cancer Program, says that while a cancer diagnosis and treatment are challenging for most people, there are some heightened and unique concerns for someone in their 20s, 30s, or 40s.
One key example is family planning, since some cancers and treatments can create challenges with being able to become pregnant or produce sperm. “It depends on each person’s situation—for example, their age, type of cancer, and treatment plan. But patients may face a decision about freezing eggs or embryos , or whether to consider sperm banking,” Borstelmann says. “Reproductive concerns can add to the distress that cancer patients are already experiencing, and they are important issues for patients and their doctors to discuss. Additional challenges include worries about insurance coverage and the financial impact of taking steps related to family planning .”
Younger women may also be concerned that cancer treatment could pose a risk of early menopause. Chemotherapy may induce menopause, or, in some cases, hormonal treatments are part of a treatment plan specifically designed to produce an early menopause. Whatever the cause, Borstelmann notes, early menopause shortens a person’s fertility window and can have other effects on their overall physical and emotional well-being.
Body image is yet another concern. There are many aspects to body image, but, for some, a clearly visible issue to manage is hair loss, which can be a side effect of chemotherapy, Borstelmann says. “For some, it's very distressing.”
Sexual function and sexual health issues are also common and can range from changes in bodily sensation (for example, for a woman who has had a mastectomy) to erectile dysfunction (for example, after prostate cancer treatment). Younger individuals diagnosed with any type of cancer, however, may struggle with the direct or indirect impact of cancer on their sexual health and how they feel about their bodies. Some describe a sense of loss and fear related to developing or sustaining intimate relationships.
What’s more, because cancer is happening at such young ages, even after treatment, there is the possibility that the cancer could come back, which is especially difficult for survivors who still have decades of life ahead of them. This is a particular concern for those with thyroid cancer , who face a risk of recurrence that is highest in the first five years after diagnosis and treatment, but persists throughout their lifetime, says Yale Medicine endocrine surgeon Courtney Gibson, MD, MS . “Since the life expectancy of young adults remains largely unchanged after a thyroid cancer diagnosis, the fact that recurrence can happen at any time is very unsettling,” she says. “However, we can provide reassurance that if it returns, we still have effective ways to treat it.”
Is there any way to avoid early-onset cancer?
The advice on the topic—for everyone—remains the same: Pay attention to exercise and nutrition, don’t smoke or drink too much alcohol, and be aware of family history and share it with a primary care physician, the doctors say.
Following up with a doctor and fully checking out any unusual symptoms can be critical, Dr. Kortmansky adds. “There is often a delay between the onset of symptoms and the actual diagnostic procedure to find the cancer,” he says. “Some of that may be driven by patients who think, ‘I'm only 40—it's probably not cancer, right?’ Other times, a physician may think rectal bleeding in a young patient is just a sign of hemorrhoids, so it’s important to advocate for yourself.”
At the same time, no patient should feel guilty or ashamed if they are diagnosed with cancer, Dr. Giri and Borstelmann say, describing two common reactions they say some of their young patients have. “It can be a human response to ask, ‘Did I do something wrong?’” Dr. Giri says. “I've seen this in some incredibly health-conscious patients who ate well and exercised. They feel completely thrown by this and need to know it’s not their fault.”
Each patient is different, and a key component of the Early-Onset Cancer Program at Yale is to ensure that patients have a place where they can talk about their feelings and experiences, Dr. Giri says. “Young people need to feel supported and holistically cared for through the course of their cancer and beyond,” she says.
More news from Yale Medicine
Too young to screen: breast cancer in younger women.

Genetic Testing for Hereditary Cancer: How it Works
13 Things To Know About Paxlovid, the Latest COVID-19 Pill
AACR Annual Meeting News: Read the latest session previews and recaps from the official news website.
Select "Patients / Caregivers / Public" or "Researchers / Professionals" to filter your results. To further refine your search, toggle appropriate sections on or off.
Cancer Research Catalyst The Official Blog of the American Association for Cancer Research

Home > Cancer Research Catalyst > Women in Cancer Research: 25 Years of Progress
Women in Cancer Research: 25 Years of Progress
In the early 1980s, the idea was first raised to the American Association for Cancer Research (AACR) Board of Directors to establish a constituency group for women working in the field of cancer research—a group committed to supporting the professional development of women and combating the challenges faced by women scientists.
At the time, only a quarter of U.S. medical school graduates and around 17% of the biomedical research workforce were women. Women comprised around 26% of the full-time faculty at universities, and of those, a mere 11% were tenured professors. Only two women had ever won the Nobel Prize in Physiology or Medicine, and only three had won the Nobel Prize in Chemistry. AACR had elected three women presidents—the first only 20 years prior, in 1961—and around 14% of its members were women.
The professional group Women in Cancer Research (WICR) was finally formed in 1988 and operated independently from but in close collaboration with AACR for its first decade. In partnership with AACR, WICR established a Directory of Members to facilitate communication and collaboration among women scientists; hosted several seminars, lectures, and workshops to discuss advancement opportunities for women in the field; and sponsored Student Travel Awards and networking receptions for AACR meetings.
In 1998, WICR was formally incorporated into the AACR as a constituency group, and its impact on the field has continued to grow. Currently, AACR has more than 25,000 women members, representing 44.6% of its total membership. Eight of the 15 members of the AACR Board of Directors; three of the last six AACR Presidents; the current AACR President-Elect, Patricia M. LoRusso, DO, PhD (hc), FAACR ; and the 2024-2025 AACR President-Elect, Lillian L. Siu, MD, FAACR ; are women. Further, during this year’s AACR Annual Meeting, more than 3,000 women will present meritorious posters.
“WICR has become a home for women scientists to network, discuss the challenges that continue to exist in the workplace, and learn how to advance in their careers,” said Margaret Foti, PhD, MD (hc) , chief executive officer of the AACR, during the celebration of WICR’s 20th anniversary . “It plays a critical role in the professional development of women in cancer science in medicine.”
As WICR gears up to celebrate a quarter century of supporting women scientists, providing critical mentorship and funding opportunities, and advocating for equality in cancer research, we spoke with two prominent members of the WICR Council—the governing board of WICR—to learn how the group has contributed to the progress of women in the field over the past 25 years.
Beverly D. Lyn-Cook, PhD: WICR Chairperson

Position: Senior research biologist at the U.S. Food and Drug Administration (FDA) National Center for Toxicological Research
AACR Member Since: 1991
Favorite WICR Activity: The Mentorship Breakfast at AACR Annual Meeting: “You have an opportunity to mentor women at all levels—undergraduates, graduates, postdocs, and young budding assistant professors seeking guidance on advancement in universities, industry, and the government.”
Serving as the WICR Chairperson during the celebration of its 25th anniversary brings back many memories, since I was present during its development. WICR was formed from the need for a voice at AACR to advocate for the development and advancement of women cancer researchers. At that time, very few women held leadership roles, chaired scientific sessions, gave major presentations at national meetings, or received major scientific awards given by AACR.
Since then, women have achieved great representation in various AACR leadership roles, including several presidents, members of the Board of Directors, and chairs of major scientific meetings. I have seen more young women reach professor status at universities and receive R01 grants in cancer research, serving as strong advocates for cancer research and survivorship.
I have watched this Council help foster these changes, working successfully with all administrations of the AACR as an advocate for advancing women in all levels of their careers. Although we have made great accomplishments, there remains the need for WICR to continue supporting the development of women, particularly those from diverse backgrounds. Fortunately, AACR leadership continues to be a strong advocate for the advancement of women in cancer research.
Sheila K. Singh, MD, PhD: Past WICR Chairperson

Position: Pediatric neurosurgeon at McMaster Children’s Hospital, professor of surgery and biochemistry and biomedical sciences and division head of Neurosurgery at Hamilton Health Sciences, and director of the Centre for Discovery in Cancer Research and Senior Canada Research Chair in Human Cancer Stem Cell Biology at McMaster University Medical Center in Hamilton, Ontario, Canada
AACR Member Since: 2015
Favorite WICR Activity: The Women and Power Workshop, held at the AACR Annual Meeting: “I love the huge demand and enthusiasm young scientists have for seeking this type of community.” And a bonus activity: “I also love attending the reception for the recipients of many of the AACR Scientific Achievement Awards, meeting these promising young scientists, and sharing career stories with them.”
Serving on the WICR Council has made me more aware and more proud of the amazing, distinguished women who have been key contributors to cancer research and clinical practice, with Dr. Edith Mitchell as a prime example. The story of her glorious career and life served to inspire me and, I think, all of AACR. We need these shining examples to give us something to strive for.
I also became very aware of the ongoing disparities and challenges women face in ascending to the highest level of institutional directorship; there are far fewer female leaders in cancer research in roles such as cancer center or institute directors, university deans, and department chairs. There are many complex reasons underlying this trend, including the challenges of childcare management as an early career researcher and the systemic sexism embedded in many institutions.
Women are now well represented in various fields of science at the trainee and early assistant professor level, but they’re not yet well represented at the full professor level. At any given time, around half of the researchers in my lab are amazing female scientists; my goal is to see them promoted throughout their career to the highest level of leadership.
Get Involved
WICR welcomes all AACR members, regardless of gender, who support the recognition, career development, and advancement of women in cancer research. Women are automatically granted membership to WICR upon joining the AACR. For more information about becoming a WICR member, visit their membership page .
Existing members of WICR can join one of the four WICR committees that plan, organize, and oversee various WICR initiatives, such as their scholarship awards program and their numerous events at the AACR Annual Meeting.
Accordingly, WICR will honor their 25th anniversary through a number of events at the AACR Annual Meeting 2024 , which will be held April 5-10 in San Diego. Highlights include the WICR 25th Anniversary Celebration Program and Networking Reception, the AACR-WICR Charlotte Friend Lecture , a Women and Power Workshop (sponsored by the Victoria’s Secret Global Fund for Women’s Cancers, in partnership with Pelotonia), and a meet-and-greet for WICR members and leadership.
Additionally, WICR is pleased to recognize early-career investigators who are recipients of WICR Scholar awards. In celebration of the WICR 25th anniversary, 25 WICR Scholars have been funded for participation in this year’s AACR Annual Meeting.
For more information on these events and other Annual Meeting 2024 programming, keep an eye on the WICR events page , where details will be updated as they become available.
- About This Blog
- Blog Policies
- Tips for Contributors

FDA Approves Two New Treatments for Acute Myeloid Leukemia

February Brings a Focus on Prevention
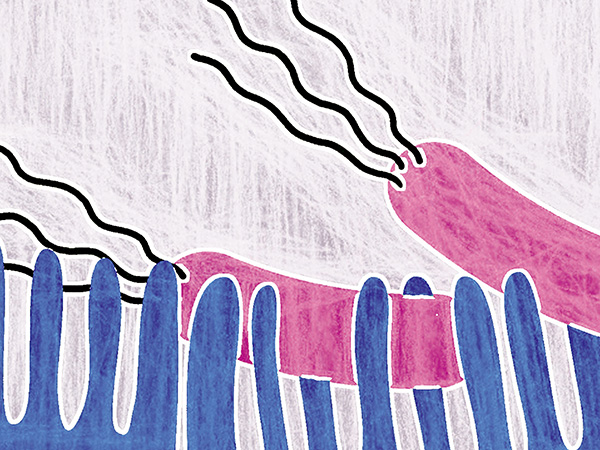
AACR Conference on the Microbiome, Viruses, and Cancer: Regulating Microbes to Reduce Chemotherapy Toxicity
Cancel reply
Your email address will not be published. Required fields are marked *
Join the Discussion (max: 750 characters)...
This site uses Akismet to reduce spam. Learn how your comment data is processed .
- Healthcare Professionals Membership
- What Is Cancer Research
- Various Types of Cancer
Mobile Menu Overlay
The White House 1600 Pennsylvania Ave NW Washington, DC 20500
FACT SHEET: President Biden Issues Executive Order and Announces New Actions to Advance Women’s Health Research and Innovation
In his State of the Union address, President Biden laid out his vision for transforming women’s health research and improving women’s lives all across America. The President called on Congress to make a bold, transformative investment of $12 billion in new funding for women’s health research. This investment would be used to create a Fund for Women’s Health Research at the National Institutes of Health (NIH) to advance a cutting-edge, interdisciplinary research agenda and to establish a new nationwide network of research centers of excellence and innovation in women’s health—which would serve as a national gold standard for women’s health research across the lifespan.
It is long past time to ensure women get the answers they need when it comes to their health—from cardiovascular disease to autoimmune diseases to menopause-related conditions. To pioneer the next generation of discoveries, the President and the First Lady launched the first-ever White House Initiative on Women’s Health Research , which aims to fundamentally change how we approach and fund women’s health research in the United States.
Today, President Biden is signing a new Executive Order that will direct the most comprehensive set of executive actions ever taken to expand and improve research on women’s health. These directives will ensure women’s health is integrated and prioritized across the federal research portfolio and budget, and will galvanize new research on a wide range of topics, including women’s midlife health.
The President and First Lady are also announcing more than twenty new actions and commitments by federal agencies, including through the U.S. Department of Health and Human Services (HHS), the Department of Defense (DoD), the Department of Veterans Affairs (VA), and the National Science Foundation (NSF). This includes the launch of a new NIH-wide effort that will direct key investments of $200 million in Fiscal Year 2025 to fund new, interdisciplinary women’s health research—a first step towards the transformative central Fund on Women’s Health that the President has called on Congress to invest in. These actions also build on the First Lady’s announcement last month of the Advanced Research Projects Agency for Health (ARPA-H) Sprint for Women’s Health , which committed $100 million towards transformative research and development in women’s health.
Today, the President is issuing an Executive Order that will:
- Integrate Women’s Health Across the Federal Research Portfolio . The Executive Order directs the Initiative’s constituent agencies to develop and strengthen research and data standards on women’s health across all relevant research and funding opportunities, with the goal of helping ensure that the Administration is better leveraging every dollar of federal funding for health research to improve women’s health. These actions will build on the NIH’s current policy to ensure that research it funds considers women’s health in the development of study design and in data collection and analysis. Agencies will take action to ensure women’s health is being considered at every step in the research process—from the applications that prospective grantees submit to the way that they report on grant implementation.
- Prioritize Investments in Women’s Health Research . The Executive Order directs the Initiative’s constituent agencies to prioritize funding for women’s health research and encourage innovation in women’s health, including through ARPA-H and multi-agency initiatives such as the Small Business Innovation Research Program and the Small Business Technology Transfer Program. These entities are dedicated to high-impact research and innovation, including through the support of early-stage small businesses and entrepreneurs engaged in research and innovation. The Executive Order further directs HHS and NSF to study ways to leverage artificial intelligence to advance women’s health research. These additional investments—across a wide range of agencies—will support innovation and open new doors to breakthroughs in women’s health.
- Galvanize New Research on Women’s Midlife Health . To narrow research gaps on diseases and conditions associated with women’s midlife health or that are more likely to occur after menopause, such as rheumatoid arthritis, heart attack, and osteoporosis, the President is directing HHS to: expand data collection efforts related to women’s midlife health; launch a comprehensive research agenda that will guide future investments in menopause-related research; identify ways to improve management of menopause-related issues and the clinical care that women receive; and develop new resources to help women better understand their options for menopause-related symptoms prevention and treatment. The Executive Order also directs the DoD and VA to study and take steps to improve the treatment of, and research related to, menopause for Service women and women veterans.
- Assess Unmet Needs to Support Women’s Health Research . The Executive Order directs the Office of Management and Budget and the Gender Policy Council to lead a robust effort to assess gaps in federal funding for women’s health research and identify changes—whether statutory, regulatory, or budgetary—that are needed to maximally support the broad scope of women’s health research across the federal government. Agencies will also be required to report annually on their investments in women’s health research, as well as progress towards their efforts to improve women’s health.
Today, agencies are also announcing new actions they are taking to promote women’s health research , as part of their ongoing efforts through the White House Initiative on Women’s Health Research. Agencies are announcing actions to:
Prioritize and Increase Investments in Women’s Health Research
- Launch an NIH-Cross Cutting Effort to Transform Women’s Health Throughout the Lifespan. NIH is launching an NIH-wide effort to close gaps in women’s health research across the lifespan. This effort—which will initially be supported by $200 million from NIH beginning in FY 2025—will allow NIH to catalyze interdisciplinary research, particularly on issues that cut across the traditional mandates of the institutes and centers at NIH. It will also allow NIH to launch ambitious, multi-faceted research projects such as research on the impact of perimenopause and menopause on heart health, brain health and bone health. In addition, the President’s FY25 Budget Request would double current funding for the NIH Office of Research on Women’s Health to support new and existing initiatives that emphasize women’s health research.
This coordinated, NIH-wide effort will be co-chaired by the NIH Office of the Director, the Office of Research on Women’s Health, and the institute directors from the National Institute on Aging; the National Heart, Lung, and Blood Institute; the National Institute on Drug Abuse; the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Institute on Arthritis, Musculoskeletal and Skin Diseases.
- Invest in Research on a Wide Range of Women’s Health Issues. The bipartisan Congressionally Directed Medical Research Program (CDMRP), led out of DoD, funds research on women’s health encompassing a range of diseases and conditions that affect women uniquely, disproportionately, or differently from men. While the programs and topic areas directed by Congress differ each year, CDMRP has consistently funded research to advance women’s health since its creation in 1993. In Fiscal Year 2022, DoD implemented nearly $490 million in CDMRP investments towards women’s health research projects ranging from breast and ovarian cancer to lupus to orthotics and prosthetics in women. In Fiscal Year 2023, DoD anticipates implementing approximately $500 million in CDMRP funding for women’s health research, including in endometriosis, rheumatoid arthritis, and chronic fatigue.
- Call for New Proposals on Emerging Women’s Health Issues . Today, NSF is calling for new research and education proposals to advance discoveries and innovations related to women’s health. To promote multidisciplinary solutions to women’s health disparities, NSF invites applications that would improve women’s health through a wide range of disciplines—from computational research to engineering biomechanics. This is the first time that NSF has broadly called for novel and transformative research that is focused entirely on women’s health topics, and proposals will be considered on an ongoing basis.
- Increase Research on How Environmental Factors Affect Women’s Health. The Environmental Protection Agency (EPA) is updating its grant solicitations and contracts to ensure that applicants prioritize, as appropriate, the consideration of women’s exposures and health outcomes. These changes will help ensure that women’s health is better accounted for across EPA’s research portfolio and increase our knowledge of women’s environmental health—from endocrine disruption to toxic exposure.
- Create a Dedicated, One-Stop Shop for NIH Funding Opportunities on Women’s Health. Researchers are often unaware of existing opportunities to apply for federal funding. To help close this gap, NIH is issuing a new Notice of Special Interest that identifies current, open funding opportunities related to women’s health research across a wide range of health conditions and all Institutes, Centers, and Offices. The NIH Office of Research on Women’s Health will build on this new Notice by creating a dedicated one-stop shop on open funding opportunities related to women’s health research. This will make it easier for researchers and institutions to find and apply for funding—instead of having to search across each of NIH’s 27 institutes for funding opportunities.
Foster Innovation and Discovery in Women’s Health
- Accelerate Transformative Research and Development in Women’s Health. ARPA-H’s Sprint for Women’s Health launched in February 2024 commits $100 million to transformative research and development in women’s health. ARPA-H is soliciting ideas for novel groundbreaking research and development to address women’s health, as well as opportunities to accelerate and scale tools, products, and platforms with the potential for commercialization to improve women’s health outcomes.
- Support Private Sector Innovation Through Additional Federal Investments in Women’s Health Research. The NIH’s competitive Small Business Innovation Research Program and the Small Business Technology Transfer Program is committing to further increasing—by 50 percent—its investments in supporting innovators and early-stage small businesses engaged in research and development on women’s health. These programs will solicit new proposals on promising women’s health innovation and make evidence-based investments that bridge the gap between performance of basic science and commercialization of resulting innovations. This commitment for additional funds builds on the investments the Administration has already made to increase innovation in women’s health through small businesses, including by increasing investments by sevenfold between Fiscal Year 2021 and Fiscal Year 2023.
- Advance Initiatives to Protect and Promote the Health of Women. The Food and Drug Administration (FDA) seeks to advance efforts to help address gaps in research and availability of products for diseases and conditions that primarily impact women, or for which scientific considerations may be different for women, and is committed to research and regulatory initiatives that facilitate the development of safe and effective medical products for women. FDA also plans to issue guidance for industry that relates to the inclusion of women in clinical trials and conduct outreach to stakeholders to discuss opportunities to advance women’s health across the lifespan. And FDA’s Office of Women’s Health will update FDA’s framework for women’s health research and seek to fund research with an emphasis on bridging gaps in knowledge on important women’s health topics, including sex differences and conditions that uniquely or disproportionately impact women.
- Use Biomarkers to Improve the Health of Women Through Early Detection and Treatment of Conditions, such as Endometriosis. NIH will launch a new initiative dedicated to research on biomarker discovery and validation to help improve our ability to prevent, diagnose, and treat conditions that affect women uniquely, including endometriosis. This NIH initiative will accelerate our ability to identify new pathways for diagnosis and treatment by encouraging multi-sector collaboration and synergistic research that will speed the transfer of knowledge from bench to bedside.
- Leverage Engineering Research to Improve Women’s Health . The NSF Engineering Research Visioning Alliance (ERVA) is convening national experts to identify high-impact research opportunities in engineering that can improve women’s health. ERVA’s Transforming Women’s Health Outcomes Through Engineering visioning event will be held in June 2024, and will bring together experts from across engineering—including those in microfluidics, computational modeling, artificial intelligence/imaging, and diagnostic technologies and devices—to evaluate the landscape for new applications in women’s health. Following this event, ERVA will issue a report and roadmap on critical areas where engineering research can impact women’s health across the lifespan.
- Drive Engineering Innovations in Women’s Health Discovery . NSF awardees at Texas A&M University will hold a conference in summer 2024 to collectively identify challenges and opportunities in improving women’s health through engineering. Biomedical engineers and scientists will explore and identify how various types of engineering tools, including biomechanics and immuno-engineering, can be applied to women’s health and spark promising new research directions.
Expand and Leverage Data Collection and Analysis Related to Women’s Health
- Help Standardize Data to Support Research on Women’s Health. NIH is launching an effort to identify and develop new common data elements related to women’s health that will help researchers share and combine datasets, promote interoperability, and improve the accuracy of datasets when it comes to women’s health. NIH will initiate this process by convening data and scientific experts across the federal government to solicit feedback on the need to develop new NIH-endorsed common data elements—which are widely used in both research and clinical settings. By advancing new tools to capture more data about women’s health, NIH will give researchers and clinicians the tools they need to enable more meaningful data collection, analysis, and reporting and comprehensively improve our knowledge of women’s health.
- Reflect Women’s Health Needs in National Coverage Determinations. The Centers for Medicare & Medicaid Services (CMS) will strengthen its review process, including through Coverage with Evidence Development guidance, to ensure that new medical services and technologies work well in women, as applicable, before being covered nationally through the Medicare program. This will help ensure that Medicare funds are used for treatments with a sufficient evidence base to show that they actually work in women, who make up more than half of the Medicare population.
- Leverage Data and Quality Measures to Advance Women’s Health Research. The Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration (HRSA) are building on existing datasets to improve the collection, analysis, and reporting of information on women’s health. The CDC is expanding the collection of key quality measures across a woman’s lifespan, including to understand the link between pregnancy and post-partum hypertension and heart disease, and plans to release the Million Hearts Hypertension in Pregnancy Change Package. This resource will feature a menu of evidence-informed strategies by which clinicians can change care processes. Each strategy includes tested tools and resources to support related clinical quality improvement. HRSA is modernizing its Uniform Data System in ways that will improve the ability to assess how women are being served through HRSA-funded health centers. By improving the ability to analyze data on key clinical quality measures, CDC and HRSA can help close gaps in women’s health care access and identify new opportunities for high-impact research.
Strengthen Coordination, Infrastructure, and Training to Support Women’s Health Research
- Launch New Joint Collaborative to Improve Women’s Health Research for Service Members and Veterans. DoD and VA are launching a new Women’s Health Research collaborative to explore opportunities that further promote joint efforts to advance women’s health research and improve evidence-based care for Service members and veterans. The collaborative will increase coordination with the goal of helping improve care across the lifespan for women in the military and women veterans. The Departments will further advance research on key women’s health issues and develop a roadmap to close pressing research gaps, including those specifically affecting Service women and women veterans.
- Coordinate Research to Advance the Health of Women in the Military. DoD will invest $10 million, contingent on available funds, in the Military Women’s Health Research Partnership. This Partnership is led by the Uniformed Services University and advances and coordinates women’s health research across the Department. The Partnership is supporting research in a wide range of health issues affecting women in the military, including cancers, mental and behavioral health, and the unique health care needs of Active Duty Service Women. In addition, the Uniformed Services University established a dedicated Director of Military Women’s Health Research Program, a role that is responsible for identifying research gaps, fostering collaboration, and coordinating and aligning a unified approach to address the evolving needs of Active Duty Service Women.
- Support EPA-Wide Research and Dissemination of Data on Women’s Health. EPA is establishing a Women’s Health Community of Practice to coordinate research and data dissemination. EPA also plans to direct the Board of Scientific Counselors to identify ways to advance EPA’s research with specific consideration of the intersection of environmental factors and women’s health, including maternal health.
- Expand Fellowship Training in Women’s Health Research. CDC, in collaboration with the CDC Foundation and American Board of Obstetrics and Gynecology, is expanding training in women’s health research and public health surveillance to OBGYNs, nurses and advanced practice nurses. Through fellowships and public health experiences with CDC, these clinicians will gain public health research skills to improve the health of women and children exposed to or affected by infectious diseases, mental health and substance use disorders. CDC will invite early career clinicians to train in public health and policy to become future leaders in women’s health research.
Improve Women’s Health Across the Lifespan
- Create a Comprehensive Research Agenda on Menopause. To help women get the answers they need about menopause, NIH will launch its first-ever Pathways to Prevention series on menopause and the treatment of menopausal symptoms. Pathways to Prevention is an independent, evidence-based process to synthesize the current state of the evidence, identify gaps in existing research, and develop a roadmap that can be used to help guide the field forward. The report, once completed, will help guide innovation and investments in menopause-related research and care across the federal government and research community.
- Improve Primary Care and Preventive Services for Women . The Agency for Healthcare Research and Quality (AHRQ) will issue a Notice of Intent to publish a funding opportunity announcement for research to advance the science of primary care, which will include a focus on women’s health. Through this funding opportunity, AHRQ will build evidence about key elements of primary care that influence patient outcomes and advance health equity—focusing on women of color—such as care coordination, continuity of care, comprehensiveness of care, person-centered care, and trust. The results from the funding opportunity will shed light on vital targets for improvements in the delivery of primary healthcare across a woman’s lifespan, including women’s health preventive services, prevention and management of multiple chronic diseases, perinatal care, transition from pediatric to adult care, sexual and reproductive health, and care of older adults.
- Promote the Health of American Indian and Alaska Native Women. The Indian Health Service is launching a series of engagements, including focus groups, to better understand tribal beliefs related to menopause in American Indian and Alaska Native Women. This series will inform new opportunities to expand culturally informed patient care and research as well as the development of new resources and educational materials.
- Connect Research to Real-World Outcomes to Improve Women’s Mental and Behavioral Health. The Substance Abuse and Mental Health Services Administration (SAMHSA) is supporting a range of health care providers to address the unique needs of women with or at risk for mental health and substance use disorders. Building on its current efforts to provide technical assistance through various initiatives , SAMHSA intends, contingent on available funds, to launch a new comprehensive Women’s Behavioral Health Technical Assistance Center. This center will identify and improve the implementation of best practices in women’s behavioral health across the life span; identify and fill critical gaps in knowledge of and resources for women’s behavioral health; and provide learning opportunities, training, and technical assistance for healthcare providers.
- Support Research on Maternal Health Outcomes. USDA will fund research to help recognize early warning signs of maternal morbidity and mortality in recipients of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and anticipates awarding up to $5 million in Fiscal Year 2023 to support maternal health research through WIC. In addition, research being conducted through the Agricultural Research Service’s Human Nutrition Research Centers is focusing on women’s health across the lifespan, including the nutritional needs of pregnant and breastfeeding women and older adults.
Stay Connected
We'll be in touch with the latest information on how President Biden and his administration are working for the American people, as well as ways you can get involved and help our country build back better.
Opt in to send and receive text messages from President Biden.
Seattle Children’s gets $50 million donation for cancer research
Seattle Children’s Hospital received a $50 million donation from the William Lawrence & Blanche Hughes Foundation to further childhood cancer research and prevention, the hospital announced Thursday.
The donation is one of the largest gifts given to the hospital by an individual donor in its history, according to a news release. The foundation is based in California and focuses its philanthropic efforts on furthering research on pediatric acute lymphocytic leukemia.
To honor the donation, the hospital will rename the Seattle Children’s Research Institute building, at 1920 Terry Ave., in honor of B. Wayne Hughes, founder of Public Storage and American Homes 4 Rent, who died in 2021.
“We are deeply grateful for the William Lawrence and Blanche Hughes Foundation and the Hughes family’s incredible generosity that will enable our talented teams to continue to expand their groundbreaking work,” Jeff Sperring, Seattle Children’s chief executive officer, said in a statement.
The $50 million donation is the latest to the hospital from the foundation. Previously, the hospital was given $50 million to fund pediatric immunotherapy cancer research.
Hughes started the foundation after losing his son, Parker, at age 8 to leukemia in 1998. The foundation was named after Hughes’ parents.
“My father, Wayne Hughes, always wanted to not only cure childhood leukemia but to help create a future free of pediatric cancers so that fewer families suffer the traumatic loss of a child,” Tamara Gustavson, director of the foundation, said in the release.
Correction: Hughes lost his son, Parker, to leukemia in 1998.
Most Read Local Stories
- These Puget Sound orcas could be designated as distinct species
- 'Belltown Hellcat' driver Miles Hudson charged with reckless driving
- Survey shows when Washingtonians leave tips and when they don't
- Missing Everett 4-year-old found dead, police say
- Police have video related to racial harassment of Utah team in Idaho
The opinions expressed in reader comments are those of the author only and do not reflect the opinions of The Seattle Times.

IMAGES
COMMENTS
Milestones in Cancer Research and Discovery. During the past 250 years, we have witnessed many landmark discoveries in our efforts to make progress against cancer, an affliction known to humanity for thousands of years. This timeline shows a few key milestones in the history of cancer research.
History of Cancer. 3000 BCE: The world's earliest known mention of cancer was found in a papyrus document from ancient Egypt. It described tumors found in the breast. The cancer was treated by destroying the tissue with a hot instrument called "the fire drill"—a technique we now call "cauterization.". Some writings have shown that ...
The History of Cancer. The study of cancer, called oncology, is the work of countless doctors and scientists around the world whose discoveries in anatomy, physiology, chemistry, epidemiology, and other related fields made oncology what it is today. Technological advances and the ever-increasing understanding of cancer make this field one of ...
The history of cancer describes the development of the field of oncology and its role in the history of medicine. Early diagnosis ... In 1973, cancer research led to a cold war incident, where co-operative samples of reported oncoviruses were discovered to be contaminated by HeLa.
The National Cancer Act of 1937. In 1937, Congress established the National Cancer Act of 1937 to provide additional support for cancer research—it was the first time Congress had appropriated funds toward a noncommunicable disease. The act, signed by President Franklin D. Roosevelt, established the National Cancer Institute (NCI) as the federal government's primary agency to address ...
History of Cancer Research. Cancer research is a vast field of medicine, with the oldest reference found to be of Le Clerc who suggested in 1727, to cut out swellings, polyps, and tumefactions before they became cancerous. Giovanni Morgagni of Padua pioneered the technique of doing autopsy to link the patient's disease to postmortem ...
History of Cancer Screening and Early Detection ... understood much about how cancer develops. Today, research is discovering new carcinogens, explaining how they cause cancer, and providing insight into ways to prevent cancer. By the middle of the 20th century, scientists had the instruments they needed to work
As part of our dedication to preserving the record of cancer research, and to celebrate our 100th Anniversary, the AACR has commissioned a series of historical review articles to be published serially in our flagship journal, Cancer Research. This history series is intended to cover the major scientific advances of the past 100 years in the ...
Cancer research until the 1980s was dominated by a tumour-centric view 7 postulating that mutations in oncogenes and tumour suppressor genes were sufficient to determine carcinogenesis and cancer ...
What is theCancer History Project. The goal of the Cancer History Project is twofold: to collect and preserve the history of cancer research, and to spark rigorous discussion of the achievements of the past half-century. Created to mark the 50th anniversary of the National Cancer Act of 1971, the Cancer History Project is a free historical ...
The International Journal of Cancer is a cancer journal from the Union for International Cancer Control covering experimental and clinical cancer research. This mini-review chronicles the history of cancer ranging from cancerous growths discovered in dinosaur fossils, suggestions of cancer in Ancient Egyptian papyri written in 1500-1600 BC ...
The act, which dramatically increased funding for cancer research, named MSK as one of only three institutions in the country designated as a Comprehensive Cancer Center, charged with translating laboratory research into clinical practice. MSK board member Benno Schmidt chaired the 26-member panel that developed the act.
The American Cancer Society was founded in 1913 by 10 doctors and five laypeople in New York City. It was originally called the American Society for the Control of Cancer (ASCC). At that time, a cancer diagnosis meant near-certain death. Rarely mentioned in public, this disease was steeped in fear and denial. Doctors sometimes did not even tell ...
It was the invention of the microscope that revealed the cancer cell itself. The early 20th century saw great strides made in understanding the structures, functions and chemistry of living organisms. Cancer research in cell culture, chemical carcinogens, diagnostic techniques and chemotherapy firmly established oncology as science. Researchers ...
About the AACR. President-Elect: Patricia M. LoRusso, DO, PhD (hc), FAACR (2023-2024) The AACR has more than 58,000 members residing in 141 countries and territories. Members include laboratory, translational, and clinical researchers; other health care professionals; and cancer advocates.
1907-1915: The Founding Years. [ Timeline of events, 1907-1915] The American Association for Cancer Research was founded in 1907 at a propitious time. European scientific advances in the late 19th century had set the stage for progress against cancer, a disease that had long been considered hopeless.
The National Cancer Institute (NCI) is the federal government's principal agency for cancer research and training. Established under the National Cancer Institute Act of 1937, NCI is part of the National Institutes of Health (NIH), one of 11 agencies that make up the Department of Health and Human Services (HHS).
During the 18th century, 3 important observations launched the field of cancer epidemiology (epidemiology is the study of causes, distribution, and control of diseases): In 1713, Bernardino Ramazzini, an Italian doctor, reported the virtual absence of cervical cancer and relatively high incidence of breast cancer in nuns and wondered if this ...
Credit us as authors by referencing Cancer Research UK as the primary source. Suggested styles are: Web content: Cancer Research UK, full URL of the page, Accessed [month] [year]. Publications: Cancer Research UK ([year of publication]), Name of publication, Cancer Research UK. Graphics (when reused unaltered): Credit: Cancer Research UK.
Fifteen years ago, the American Association for Cancer Research (AACR) marked its 100th anniversary with the launch of Landmarks in Cancer Research 1907 - 2007, a historical timeline of the seminal scientific discoveries and events that occurred throughout the AACR's first century of existence. The ensuing fifteen years have brought a rapid ...
Her husband's cancer and their search for cancer information online inspired CancerHelp UK. History. To begin with, the Medical School server at the University of Birmingham hosted CancerHelp UK. The management of the site passed to The Cancer Research Campaign in 2000. In 2002, The Cancer Research Campaign and the Imperial Cancer Research Fund ...
In this excerpt from his forthcoming book on the history of cancer research, Joe Lipsick looks back at the early history of tumor virus research, from some of the early false starts and debates, to discovery of reverse transcriptase, and identification of human papilloma virus (HPV) as the major cause of cervical cancer. Go to:
American Cancer Society. History of cancer epidemiology: 18th century to present. Maurer Foundation. A brief history of breast cancer. American Cancer Society. Disproven or controversial breast cancer risk factors. National Cancer Institute. Milestones in cancer research and discovery. Young RH, Louis DN.
The cancer research community has a shared goal: to improve patient lives through basic, translational, and clinical research. We began addressing this goal by focusing on understanding how cancer cells differ from normal cells, reasoning that the knowledge would inform us about exploitable cancer cell vulnerabilities.
Pancreatic cancer: In a phase I trial of a personalized mRNA vaccine, half of the participants developed T cells targeted to cancer neoantigens 6. Recurrence-free survival in this group was longer ...
New research published in JAMA Oncology shows that an estimated 1 in 9 cancer diagnoses were missed in the USA during the first part of the COVID-19 pandemic (March-December, 2020), translating to 134 395 undiagnosed cancers during that time . The authors, led by Todd Burus (Markey Cancer Center, University of Kentucky, Lexington, KY, USA), calculated the missing diagnoses by comparing ...
Age itself is the first and obvious difference. "Early-onset" can be defined in various ways based on the cancer type. "For example, early-onset breast cancer refers to a diagnosis in someone younger than age 45, while early-onset colorectal cancer is a diagnosis that occurs in someone younger than 50," says Dr. Giri. "To be as inclusive as possible, the Early-Onset Cancer Program at ...
Position: Senior research biologist at the U.S. Food and Drug Administration (FDA) National Center for Toxicological Research AACR Member Since: 1991 Favorite WICR Activity: The Mentorship Breakfast at AACR Annual Meeting: "You have an opportunity to mentor women at all levels—undergraduates, graduates, postdocs, and young budding assistant professors seeking guidance on advancement in ...
To narrow research gaps on diseases and conditions associated with women's midlife health or that are more likely to occur after menopause, such as rheumatoid arthritis, heart attack, and ...
Previously, the hospital was given $50 million to fund pediatric immunotherapy cancer research. Hughes started the foundation after losing his son, Parker, at age 8 to leukemia in 1998. The ...