
An official website of the United States government
Here’s how you know
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites. .

Coronavirus Disease (COVID-19) Best Practice Case Studies
The COVID-19 incident period ended on May 11, 2023. FEMA will continue to provide funeral assistance until Sept. 30, 2025, to those who have lost loved ones due to this pandemic.
The following is a collection of key findings and considerations for jurisdictions and communities regarding ongoing COVID-19 pandemic operations across the country. They cover topics such as:
- Government Engagement with Citizens
- Considerations for People with Disabilities
- Community Emergency Response Teams
- Volunteer Management
The COVID-19 Best Practices are searchable by title or keyword below, and they can be filtered by FEMA's community lifelines and core capabilities .
Community lifelines enable the continuous operation of essential government and business functions to promote public health and safety and economic security.
Core capabilities are distinct, critical elements that are necessary to achieve our National Preparedness Goal .
For more information on these COVID-19 best practices, organizations and individuals can email the FEMA Continuous Improvement Team .
Search for Best Practice Case Studies
FEMA does not endorse any non-government entities, organizations, or services. Claims made by third parties have not been independently verified by FEMA.
Education and Employment Support for People with Disabilities During COVID-19
Accessibility of covid-19 information-sharing and public communications for people with disabilities, disaster shelter services for people with disabilities during covid-19, crisis counseling services for people with disabilities during covid-19, healthcare considerations for people with disabilities during covid-19.
WHO COVID-19 dashboard
WHO Health Emergencies Programme
- African Region
- Eastern Mediterranean Region
- European Region
- Region of the Americas
- South-East Asia Region
- Western Pacific Region
- World Bank Income Group
- High Income
- Lower Middle Income
- Upper Middle Income
- Country, territory or area
- Afghanistan
- American Samoa
- Antigua and Barbuda
- Bolivia (Plurinational State of)
- Bonaire, Sint Eustatius and Saba
- Bosnia and Herzegovina
- British Virgin Islands
- Brunei Darussalam
- Burkina Faso
- Cayman Islands
- Central African Republic
- Cook Islands
- Côte d'Ivoire
- Democratic People's Republic of Korea
- Democratic Republic of the Congo
- Dominican Republic
- El Salvador
- Equatorial Guinea
- Falkland Islands (Malvinas)
- Faroe Islands
- French Guiana
- French Polynesia
- Guinea-Bissau
- Iran (Islamic Republic of)
- Isle of Man
- Kosovo (In accordance with UN Security Council Resolution 1244 (1999))
- Lao People's Democratic Republic
- Liechtenstein
- Marshall Islands
- Micronesia (Federated States Of)
- Netherlands (Kingdom of the)
- New Caledonia
- New Zealand
- Norfolk Island
- North Macedonia
- Northern Mariana Islands (Commonwealth of the)
- occupied Palestinian territory, including east Jerusalem
- Papua New Guinea
- Philippines
- Pitcairn Islands
- Puerto Rico
- Republic of Korea
- Republic of Moldova
- Russian Federation
- Saint Barthélemy
- Saint Helena
- Saint Kitts and Nevis
- Saint Lucia
- Saint Martin (French part)
- Saint Pierre and Miquelon
- Saint Vincent and the Grenadines
- Sao Tome and Principe
- Saudi Arabia
- Sierra Leone
- Sint Maarten (Dutch part)
- Solomon Islands
- South Africa
- South Sudan
- Switzerland
- Syrian Arab Republic
- Timor-Leste
- Trinidad and Tobago
- Turkmenistan
- Turks and Caicos Islands
- United Arab Emirates
- United Kingdom of Great Britain and Northern Ireland
- United Republic of Tanzania
- United States of America
- United States Virgin Islands
- Venezuela (Bolivarian Republic of)
- Wallis and Futuna
- Circulation
- More resources
Coronavirus (COVID-19) cases, %%COUNTRY%% data
Source: world health organization.
All data represents the date of reporting as opposed to date of symptom onset. All data is subject to continuous verification and may change based on retrospective updates to accurately reflect trends, changes in country case definitions and/or reporting practices. Significant data errors detected or reported to WHO may be corrected at more frequent intervals with some countries performing retrospective bulk corrections may lead to the appearance of significant spikes or negative values which are verified and validated by WHO.
In the context of WHO's statistical reporting of COVID-19 data, it is important to note that only confirmed cases are included in case and death counts. In guidance updated on 22 July 2023; there are two alternative definitions for 'Confirmed case of SARS-CoV-2 infection' in international surveillance reporting, although some departures may exist due to local adaptations:
a) A person with a positive Nucleic Acid Amplification Test (NAAT), regardless of clinical criteria OR epidemiological criteria. b) A person meeting clinical criteria AND/OR epidemiological criteria (suspect case A) with a positive professional-use or self-test SARS-CoV-2 Antigen-RDT.
Additionally, WHO only disseminates data as reported by its Member States. From the 31 December 2019 to the 21 March 2020, WHO collected the numbers of confirmed COVID-19 cases and deaths through official communications under the International Health Regulations (IHR, 2005), complemented by monitoring the official ministries of health websites and social media accounts.
Since 22 March 2020, global data has been compiled through WHO region-specific dashboards, and/or aggregate count data reported directly to WHO headquarters by Member States. Statistical counts include both domestic and repatriated cases. Case detection, definitions, testing strategies, reporting practice, and lag times (e.g. time to case notification, and time to reporting of deaths) differ between countries, territories and areas. These factors, amongst others, influence the counts presented with variable under or overestimation of true case and death counts, and variable delays to reflecting these statistics at a global level. Please note that statistics do not necessarily reflect the actual number of cases and deaths or the actual number of countries where cases and deaths are occurring, as a number of countries have stopped reporting or changed their frequency of reporting.
Trends in COVID-19 cases, %%COUNTRY%%
Recent covid-19 cases reported to who (weekly).
%%COUNTRY%%, July 2023 - present
Total COVID-19 cases reported to WHO (weekly)
%%COUNTRY%%, January 2020 - present
A number of countries have stopped reporting or changed their frequency of reporting COVID-19 case and death counts to WHO. An outcome of these differences in reporting is that WHO may receive daily data from some countries, while other countries may only report data to WHO once every 14 days. In addition, countries differ in how they choose to report statistics; some countries provide their data attributed to specific dates while others who report less frequently may group data from 7 days into a single statistic attributed to a week in their reporting. As of 25 August 2023, WHO declared that it is no longer necessary for Member States to report daily counts of cases and deaths to WHO and requested strengthening of weekly reporting.
Reported data is still available attributed to specific dates (daily data) here as a download . This dashboard presents the same statistics as weekly figures in charts in order to mitigate against the visual misinterpretation of data. Should daily data have been presented here, many countries would show zero counts for multiple consecutive days due in part to the differences in how they choose to report. While weekly intervals do not completely mitigate against this, the approach reduces the risk that some dashboard users might infer zero cases or deaths when lack of data is often due to reporting differences.
What do negative counts of cases or deaths mean? All data is subject to continuous verification and may change based on retrospective updates to accurately reflect trends, changes in country case definitions and/or reporting practices. Significant data errors detected or reported to WHO may be corrected by Member States at more frequent intervals with some countries performing retrospective bulk corrections in their reporting. Bulk corrections may lead to the appearance of significant spikes or negative values which are verified and validated by WHO.
Aggregate groups (weekly data to week end date)
Covid-19 cases, country level trends, percent change based on previous 28 days source: world health organization, glossary and definitions.
| Confirmed COVID-19 case | Although COVID-19 defines the symptomatic disease caused by SARS-CoV-2, the cases are presented in this dashboard meet one of two alternate definitions of confirmed case of SARS-CoV-2 infection in international surveillance reporting: a) A person with a positive Nucleic Acid Amplification Test (NAAT), regardless of clinical criteria* OR epidemiological criteria*.
|
|---|---|
| Last 7 days | ‘Last 7 days’ refers to the most recent complete epidemiological week (commonly referred to as an 'epi week'). |
| Last 28 days | ‘Last 28 days’ refers to the four preceding most recently complete epidemiological weeks. |
| WHO Regions | The World Health Organization (WHO) is divided into six regions with regional offices, each responsible for addressing health challenges and promoting public health within its designated geographical area. These regions serve as administrative units that allow the WHO to tailor its efforts to the specific needs, priorities, and health conditions of member countries within each region. |
| World Bank Income Groups | The World Bank classifies economies into income groups based on their Gross National Income (GNI) per capita. These annually updated classifications help the World Bank and other organizations analyze and understand global economic trends, allocate resources, and design development policies. |
Data sources
| COVID-19 case data | From the 31 December 2019 to the 21 March 2020, WHO collected the numbers of confirmed COVID-19 cases and deaths through official communications under the International Health Regulations (IHR, 2005), complemented by monitoring the official ministries of health websites and social media accounts. Since 22 March 2020, global data is compiled through WHO region-specific dashboards, and/or aggregate count data reported to WHO headquarters. WHO COVID-19 Dashboard is updated every Friday for the period of two weeks prior. Counts primarily reflect laboratory-confirmed cases and deaths, based upon WHO case definitions; although some departures may exist due to local adaptations. Counts include both domestic and repatriated cases. Case detection, definitions, testing strategies, reporting practice, and lag times (e.g. time to case notification, and time to reporting of deaths) differ between countries, territories and areas. These factors, amongst others, influence the counts presented with variable under or overestimation of true case and death counts, and variable delays to reflecting these data at a global level. All data represent date of reporting as opposed to date of symptom onset. All data are subject to continuous verification and may change based on retrospective updates to accurately reflect trends, changes in country case definitions and/or reporting practices. Significant data errors detected or reported to WHO may be corrected at more frequent intervals. |
|---|---|
| Population data | Estimated populations and projections are drawn from: , Population Division. World Population Prospects 2019, Online Edition. Rev. 1 (2020 projections). (population as of 1 January by country, year, age and gender; last updated by Eurostat on 2021-02-12; last year of data: 2020). . Estimates of population for Bonaire, Sint Eustatius and Saba.*Total population for France has been adjusted to account for the following overseas territories (French Guiana, Guadeloupe, Martinique, Mayotte, Réunion, Saint Martin). |
Copyright and licensing
| Copyright | Attribution 4.0 International (CC BY 4.0) |
|---|---|
| License | The World Health Organization (“WHO”) encourages public access and use of the data that it collects and publishes on its web site data.who.int. The data are organized in datasets and made available in machine-readable format (“Datasets”). The Datasets have been compiled from data provided by WHO’s Member States under the WHO policy on the use and sharing of data collected by WHO in Member States outside the context of public health emergencies. Use of the data derived from the Datasets, which may appear in formats such as tables and charts, is also subject to these Terms and Conditions. Datasets may include data describing the Dataset called “Metadata”. If any datasets are credited to a source other than WHO, then those materials are not covered by these Terms and Conditions, and permission should be sought from the source provided. You are responsible for determining if this is the case, and if so, you are responsible for obtaining any necessary permission from the sources indicated. The risk of claims resulting from infringement of any third-party-owned component in the materials rests solely with you. You may use our application programming interfaces (“APIs”) to facilitate access to the Datasets, whether through a separate web site or through another type of software application. By using the Datasets or any presentations of data derived from them, or by using our APIs in connection with the Datasets, you agree to be bound by these Terms and Conditions, as may be amended from time to time by WHO at its sole discretion. Unless specifically indicated otherwise, these Datasets are provided to you under a Creative Commons Attribution 4.0 International License (CC BY 4.0), with the additional terms below. The basic terms applicable to the CC BY 4.0 license may be accessed here. By downloading or using the Datasets, you agree to comply with the terms of the CC BY 4.0 license, as well as the following mandatory and binding addition: Any dispute relating to the interpretation or application of this license shall, unless amicably settled, be subject to conciliation. In the event of failure of the latter, the dispute shall be settled by arbitration. The arbitration shall be conducted in accordance with the modalities to be agreed upon by the parties or, in the absence of agreement, with the UNCITRAL Arbitration Rules. The parties shall accept the arbitral award as final. |
| Permission type | Publicly accessible |
| Prohibited uses | You shall not attempt to de-anonymise the Datasets or use the Datasets in a manner that falsifies or misrepresents their content. You shall not, in connection with your use of the Datasets published on data.who.int, state or imply that WHO endorses, or is affiliated with, you, or that WHO endorses your use of data.who.int, or any content, output, or analysis resulting from or related to the data.who.int, or any entity, organization, company, product or services. |
| Citation | World Health Organization 2023 data.who.int, WHO Coronavirus (COVID-19) dashboard > Cases [Dashboard]. https://data.who.int/dashboards/covid19/cases |
| Disclaimer | WHO reserves the right at any time and from time to time to modify or discontinue, temporarily or permanently, the Datasets, or any means of accessing or utilizing the Datasets with or without prior notice to you. All references to Kosovo should be understood to be in the context of the United Nations Security Council resolution 1244 (1999). A dispute exists between the Governments of Argentina and the United Kingdom of Great Britain and Northern Ireland concerning sovereignty over the Falkland Islands (Malvinas). The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by WHO in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by WHO to verify the accuracy of the Datasets. However, the Datasets are being provided without warranty of any kind, either expressed or implied. You will be solely responsible for your use of the Datasets. In no event shall WHO be liable for any damages arising from such use. For full disclaimers, terms of use and your indemnification of WHO, please visit . |
- Mission and objectives
- History and achievements
- Secretariat
- Celebrating over two decades of advancing and supporting health policy and systems research
- Working in partnership
- Supporting the generation of knowledge
- Strengthening capacities
- Embedded research
- Evidence synthesis
- Gender and intersectionality
- Primary health care
- Systems thinking
- Subscribe to our newsletter »
- All publications
- Core documents
- Project documents
- Teaching and training material »
- Feature stories
- Current calls »
- Archive of past calls »
- What we do /
- Thematic areas of focus /
- Primary health care /
Primary health care case studies in the context of the COVID-19 pandemic
Section navigation.
- Primary Health Care Systems (PRIMASYS)
Since 2020, the COVID-19 pandemic has showcased the importance of primary health care (PHC) and revealed health system strengths as well as weaknesses.
As a defining global and national policy priority, COVID-19 has had enormous impacts on country health systems, often unveiling inequities as well as governance, stewardship and leadership challenges. COVID-19 demonstrates that trust between communities and service providers, and effective collaboration across sectors, are essential elements of successful public health responses and primary care continuity.
In 2015, the Alliance commissioned Primary Health Care Systems (PRIMASYS) case studies in twenty low- and middle-income countries (LMICs). Building on these case studies, the Alliance commissioned nearly 50 case studies led by in-country research teams to examine PHC in in the context of the COVID-19 pandemic. These case studies apply the Astana PHC Framework considering primary care, multisectoral policy and action and community engagement. The case studies aim to advance the science and lay a groundwork for improved policy efforts to advance PHC in LMICs.
Nearly 50 case studies commissioned across all six WHO regions
Case studies
New case studies are being added as they are completed.

Afghanistan: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Afghanistan in the context of the COVID-19 pandemic between March 2020 and...

Bhutan: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Bhutan in the context of the COVID-19 pandemic between March 2020 and June...

Cameroon: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Cameroon in the context of the COVID-19 pandemic between March 2020 and August...

Colombia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Colombia. The case study is part of a collection of case studies providing...

Egypt: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Egypt in the context of the COVID-19 pandemic between January 2020 and August...

Ethiopia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Ethiopia in the context of the COVID-19 pandemic between March 2020 and March...

Georgia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Georgia in the context of the COVID-19 pandemic between March 2020 and July...

Ghana: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Ghana. The case study is part of a collection of case studies providing...

Indonesia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Indonesia in the context of the COVID-19 pandemic between March 2020 and July...

Jordan: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Jordan in the context of the COVID-19 pandemic between January 2020...

Kenya: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Kenya. The case study is part of a collection of case studies providing critical...

Kuwait: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Kuwait in the context of the COVID-19 pandemic between March 2020 and December...

Lao People’s Democratic Republic: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Lao People’s Democratic Republic. The case study is part of...

Lebanon: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Lebanon in the context of the COVID-19 pandemic between March 2020 and December...

Malaysia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Malaysia. The case study is part of a collection of case studies providing...

Maldives: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in the Maldives in the context of the COVID-19 pandemic. The case study is part...

Mexico: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Mexico. The case study is part of a collection of case studies providing critical...

Mongolia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Mongolia in the context of the COVID-19 pandemic between March 2020...

Morocco: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Morocco in the context of the COVID-19 pandemic between January 2020...

Myanmar: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Myanmar in the context of the COVID-19 pandemic between March 2020...

Nepal: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Nepal in the context of the COVID-19 pandemic between March 2020 and June 2021....

Nigeria: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Nigeria. The case study is part of a collection of case studies providing critical...

Oman: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Oman in the context of the COVID-19 pandemic between January 2020 and August...

Pakistan: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Pakistan in the context of the COVID-19 pandemic between January 2020 and June...

Peru: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Peru. The case study is part of a collection of case studies providing critical...

Philippines: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in the Philippines in the context of the COVID-19 pandemic between January 2020...

Qatar: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Qatar in the context of the COVID-19 pandemic between January 2020...

Republic of Korea: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in the Republic of Korea in the context of the COVID-19 pandemic between March...

Rwanda: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Rwanda. The case study is part of a collection of case studies providing critical...

Saudi Arabia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Saudi Arabia in the context of the COVID-19 pandemic between March 2020 and...

Singapore: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Singapore. The case study is part of a collection of case studies...

South Africa: a primary health care case study in the context of theCOVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in South Africa in the context of the COVID-19 pandemic between March...

Sri Lanka: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Sri Lanka in the context of the COVID-19 pandemic between March 2020...

Sudan: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Sudan in the context of the COVID-19 pandemic between March 2020...

The Islamic Republic of Iran: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in the Islamic Republic of Iran in the context of the COVID-19 pandemic between...

Timor-Leste: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Timor-Leste in the context of the COVID-19 pandemic between March 2020 and...

Tunisia: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Tunisia in the context of the COVID-19 pandemic between January 2020 and August...

Uganda: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Uganda. The case study is part of a collection of case studies providing critical...

United Arab Emirates: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in United Arab Emirates in the context of the COVID-19 pandemic between January...

Viet Nam: a primary health care case study in the context of the COVID-19 pandemic
This case study examines country-level primary health care (PHC) systems in Viet Nam. The case study is part of a collection of case studies...
- Introduction
- Conclusions
- Article Information
COVID-19 indicates coronavirus disease 2019; NYS, New York State.
Cycle threshold (Ct) values for polymerase chain reaction testing. A lower value corresponds to a higher nasopharyngeal viral load, with 40 being the internal threshold for negativity.
Nonauthor collaborators
- Associations Between Built Environment, Neighborhood SES, and SARS-CoV-2 Infection JAMA Research Letter July 28, 2020 This cross-sectional study investigates associations of residential building characteristics and markers of neighborhood socioeconomic status (SES) with screen-detected SARS-CoV-2 prevalence among pregnant women delivering in 2 New York City hospitals. Ukachi N. Emeruwa, MD, MPH; Samsiya Ona, MD; Jeffrey L. Shaman, PhD; Amy Turitz, MD; Jason D. Wright, MD; Cynthia Gyamfi-Bannerman, MD, MSc; Alexander Melamed, MD, MPH
- Prevalence of SARS-CoV-2 Antibodies in Health Care Personnel in the New York City Area JAMA Research Letter September 1, 2020 This seroprevalence survey study describes severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) seropositivity among health care workers at a New York City–based health system by age, sex, race, county of residence, and prior PCR-confirmed viral exposure. Joseph Moscola, PA, MBA; Grace Sembajwe, DSc, MSc, CIH; Mark Jarrett, MD, MBA, MS; Bruce Farber, MD; Tylis Chang, MD; Thomas McGinn, MD, MPH; Karina W. Davidson, PhD, MASc; Northwell Health COVID-19 Research Consortium
- Children in the Eye of the Pandemic Storm JAMA Pediatrics Editorial October 5, 2020 Jason G. Newland, MD, MEd; Kristina A. Bryant, MD
- Nonauthor Collaborator Supplement Added JAMA Pediatrics Correction August 1, 2021
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Zachariah P , Johnson CL , Halabi KC, et al. Epidemiology, Clinical Features, and Disease Severity in Patients With Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York. JAMA Pediatr. 2020;174(10):e202430. doi:10.1001/jamapediatrics.2020.2430
Manage citations:
© 2024
- Permissions
Epidemiology, Clinical Features, and Disease Severity in Patients With Coronavirus Disease 2019 (COVID-19) in a Children’s Hospital in New York City, New York
- 1 Department of Pediatrics, Columbia University Irving Medical Center, New York, New York
- 2 Department of Infection Prevention and Control, NewYork-Presbyterian Hospital, New York
- 3 Department of Emergency Medicine, Columbia University Irving Medical Center, New York, New York
- Editorial Children in the Eye of the Pandemic Storm Jason G. Newland, MD, MEd; Kristina A. Bryant, MD JAMA Pediatrics
- Research Letter Associations Between Built Environment, Neighborhood SES, and SARS-CoV-2 Infection Ukachi N. Emeruwa, MD, MPH; Samsiya Ona, MD; Jeffrey L. Shaman, PhD; Amy Turitz, MD; Jason D. Wright, MD; Cynthia Gyamfi-Bannerman, MD, MSc; Alexander Melamed, MD, MPH JAMA
- Research Letter Prevalence of SARS-CoV-2 Antibodies in Health Care Personnel in the New York City Area Joseph Moscola, PA, MBA; Grace Sembajwe, DSc, MSc, CIH; Mark Jarrett, MD, MBA, MS; Bruce Farber, MD; Tylis Chang, MD; Thomas McGinn, MD, MPH; Karina W. Davidson, PhD, MASc; Northwell Health COVID-19 Research Consortium JAMA
- Correction Nonauthor Collaborator Supplement Added JAMA Pediatrics
Question What are the clinical manifestations of children and adolescents hospitalized with coronavirus disease 2019 (COVID-19)?
Findings In this case series of 50 children and adolescents hospitalized with COVID-19 infection, respiratory symptoms, while common, were not always present. Children hospitalized with COVID-19 commonly had comorbidities, infants had less severe disease, those with obesity were likely to receive mechanical ventilation, and elevated markers of inflammation at admission and during hospitalization were associated with severe disease.
Meaning Expanded testing, maintaining a high suspicion for severe acute respiratory syndrome coronavirus 2 infection given the variable presentation of COVID-19, risk stratification, and recognition of findings suggestive of immune dysregulation are crucial to effective COVID-19 management in children.
Importance Descriptions of the coronavirus disease 2019 (COVID-19) experience in pediatrics will help inform clinical practices and infection prevention and control for pediatric facilities.
Objective To describe the epidemiology, clinical, and laboratory features of patients with COVID-19 hospitalized at a children’s hospital and to compare these parameters between patients hospitalized with and without severe disease.
Design, Setting, and Participants This retrospective review of electronic medical records from a tertiary care academically affiliated children’s hospital in New York City, New York, included hospitalized children and adolescents (≤21 years) who were tested based on suspicion for COVID-19 between March 1 to April 15, 2020, and had positive results for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Exposures Detection of SARS-CoV-2 from a nasopharyngeal specimen using a reverse transcription–polymerase chain reaction assay.
Main Outcomes and Measures Severe disease as defined by the requirement for mechanical ventilation.
Results Among 50 patients, 27 (54%) were boys and 25 (50%) were Hispanic. The median days from onset of symptoms to admission was 2 days (interquartile range, 1-5 days). Most patients (40 [80%]) had fever or respiratory symptoms (32 [64%]), but 3 patients (6%) with only gastrointestinal tract presentations were identified. Obesity (11 [22%]) was the most prevalent comorbidity. Respiratory support was required for 16 patients (32%), including 9 patients (18%) who required mechanical ventilation. One patient (2%) died. None of 14 infants and 1 of 8 immunocompromised patients had severe disease. Obesity was significantly associated with mechanical ventilation in children 2 years or older (6 of 9 [67%] vs 5 of 25 [20%]; P = .03). Lymphopenia was commonly observed at admission (36 [72%]) but did not differ significantly between those with and without severe disease. Those with severe disease had significantly higher C-reactive protein (median, 8.978 mg/dL [to convert to milligrams per liter, multiply by 10] vs 0.64 mg/dL) and procalcitonin levels (median, 0.31 ng/mL vs 0.17 ng/mL) at admission ( P < .001), as well as elevated peak interleukin 6, ferritin, and D-dimer levels during hospitalization. Hydroxychloroquine was administered to 15 patients (30%) but could not be completed for 3. Prolonged test positivity (maximum of 27 days) was observed in 4 patients (8%).
Conclusions and Relevance In this case series study of children and adolescents hospitalized with COVID-19, the disease had diverse manifestations. Infants and immunocompromised patients were not at increased risk of severe disease. Obesity was significantly associated with disease severity. Elevated inflammatory markers were seen in those with severe disease.
Community transmission of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is now widespread in the US, with New York City (NYC), New York, continuing to be the epicenter. 1 Detailed reports of clinical features among hospitalized adults in the US are increasingly available. 2 , 3 International pediatric data suggest lower rates of severe coronavirus disease 2019 (COVID-19) in children 4 and higher rates of asymptomatic infection. 5 , 6 Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail. Being younger than 1 year has been suggested as a predisposing factor for hospitalization in initial reports, including from the US Centers for Disease Control and Prevention (CDC). 5 , 7 , 8 Detailed descriptions of the clinical course, laboratory parameters, and findings associated with severe disease in children and adolescents could help inform clinical practice and infection prevention and control (IPC) preparedness at children’s hospitals. In this article, we present the epidemiology, clinical characteristics, treatment, and outcomes of 50 pediatric patients admitted with COVID-19 to our children’s hospital from March 1 to April 15, 2020.
The study site was NewYork-Presbyterian Morgan Stanley Children’s Hospital, a tertiary care children’s hospital affiliated with Columbia University Irving Medical Center. Electronic medical records for all patients with SARS-CoV-2 detected in nasopharyngeal swabs between March 1 and April 15, 2020, were reviewed. The inclusion criteria for detailed medical record review included (1) inpatient hospitalization, (2) symptoms consistent with COVID-19 as described in the literature, 5 , 9 and (3) age 21 years or younger.
Since April 6, 2020, our hospital system has performed universal SARS-CoV-2 testing for all patients being newly hospitalized and for patients undergoing surgical procedures with the potential for aerosol generation. Asymptomatic patients who received positive test results as part of screening were excluded from further analysis.
All testing was conducted at the Columbia University Microbiology Laboratory using a real-time reverse transcriptase–polymerase chain reaction (PCR) assay (Roche Cobas SARS-CoV-2 Test). The Columbia University Irving Medical Center institutional review board approved this study, and a waiver of informed consent was provided because of the minimal risk.
For patients who met eligibility criteria, the following groups of variables were collected from the electronic medical record: presenting symptoms, duration of symptoms before presentation, comorbid conditions, hospital course, disease severity, laboratory parameters, radiologic findings, administered antiviral therapies, clinical course during hospitalization, and patterns of repeated test positivity when available. Demographic data collected included age, for which infants were defined as patients younger than 12 months and adolescents as patients ages 11 through 21 years. Race and ethnicity were as defined by documentation in the electronic medical record.
All symptoms reported at time of presentation were documented, including COVID-19 symptoms as outlined by the CDC 10 : fever (subjective or temperature ≥38 °C), cough, shortness of breath, chills, muscle pain, new loss of taste or smell, vomiting or diarrhea, and/or sore throat. Respiratory distress was defined by persistent tachypnea, use of accessory muscles documented in physical examination findings, or respiratory distress as noted in treating clinician’s documentation.
The epidemiology of admissions was assessed in association with the introduction of nonpharmaceutical interventions (NPIs) implemented within NYC. Health care–associated cases were defined as detection of SARS-CoV-2 more than 14 days after admission and/or associated with a confirmed exposure within the hospital. The presence of household contacts with illness was stratified based on compatible symptomatology or laboratory confirmation of SARS-CoV-2.
Specific comorbidities ascertained based on published work on COVID-19 included infancy (age younger than 1 year), obesity, asthma, and immunosuppression. Obesity and overweight status were defined based on the CDC’s child and teen body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) calculator for all patients 2 years and older (BMI at or above the 95th percentile for age/sex categorized as obesity; 85%-95% as overweight) and the weight for length percentiles for patients younger than 2 years (overweight above 95th percentile). 11 Immunosuppression was defined as the concurrent use of an immunosuppressive agent either for hematologic or solid malignancy, solid organ transplant, hematopoietic stem cell transplant, or ongoing severe cytopenia.
Severe disease was defined as requirement for mechanical ventilation during hospitalization. Our health care system recommended minimizing the use of noninvasive positive pressure ventilation (NIPPV) to limit aerosol generation. Time to intubation from symptom onset was collected for intubated patients. Other markers of disease severity (eg, length of stay, discharge status) were collected.
Suspected and confirmed bacterial and respiratory viral coinfections were reviewed. Our health care system restricted respiratory PCR testing starting on March 27, 2020, to conserve test supplies. Specific laboratory parameters collected included complete blood cell counts for which lymphopenia was defined as an absolute lymphocyte count (ALC) less than 4500/μL in infants younger than 8 months (to convert to ×10 9 per liter, multiply by 0.001) or an ALC of less than 1500/μL in patients 8 months or older, 12 kidney/hepatic function, and routine markers of inflammation (C-reactive protein, procalcitonin) for all patients. More comprehensive laboratory testing was performed for select patients, informed by adult protocols at our center, and included additional markers of inflammation: ferritin, D-dimer, and interleukin 6 (IL-6). Severely affected children without additional known comorbidities underwent a workup for primary immune deficiency. Radiology results were reviewed for the presence of bilateral patchy opacities, effusions, pneumothorax, and/or focal consolidation. Finally, we also reviewed readmissions and repeated testing data for included hospitalized patients.
A bivariate analysis was performed comparing comorbidities and laboratory parameters between patients with and without severe disease. This was conducted using nonparametric tests (Wilcoxon rank sum) or parametric tests ( t test) for continuous variables as appropriate. Fisher exact tests or χ 2 tests were used to compare categorical variables between patients with and without severe disease. An α of .05 was predetermined as the level of significance. All analyses were conducted using R, version 3.53 (R Foundation for Statistical Computing).
Between March 1 and April 15, 2020, 387 unique patients (484 tests total) 21 years and younger were tested for SARS-CoV-2 from the emergency department or an inpatient location, with a total of 73 positive results (15%). Among these patients with a positive SARS-CoV-2 result, 54 patients (74.0%) were hospitalized 1 day or longer. Four patients (5.5%) did not have symptoms consistent with COVID-19 and were tested before transfer to an inpatient psychiatry facility (n = 2), or after admission with another diagnosis (axillary abscess and incarcerated inguinal hernia; n = 2). The remaining 50 patients were eligible for the current study.
Forty-nine of these 50 patients (98%) acquired SARS-CoV-2 in the community; 1 infection (2%) was possibly health care associated. Close to half (27 [54%]) were male and Hispanic (25 [50%]) ( Table 1 ). The peak number of hospitalizations (6 [12%]) occurred on March 27, 2020. The number of daily hospitalizations in association with citywide school closures (March 16, 2020) and a social distancing measure enforcement called New York State on Pause (March 22, 2020) are shown in Figure 1 .
Most patients (26 [52%]) had a documented adult family member or household contact with symptoms compatible with COVID-19 (eg, congestion/rhinorrhea, sore throat, cough, fever, and/or myalgia), of whom 9 (18%) had an exposure to an individual with a confirmed case of COVID-19. No patient had a history of international travel within 14 days before symptom onset. Two parents developed symptoms consistent with COVID-19 while visiting their hospitalized children.
The median time to admission from development of symptoms was 2 days (interquartile range [IQR], 1-5 days) but was longer in adolescents (median, 4 days; IQR, 2-7 days) compared with younger children and infants (median, 1 day; IQR, 1-2 days) ( P < .001). Most patients had fever (40 [80%]) or upper/lower respiratory tract symptoms (eg, cough, congestion, sore throat, and/or shortness of breath) (32 [64%]). Infants were significantly less likely to present with respiratory distress compared with older children (1 of 14 [7%] vs 16 of 36 [44%]; P = .02). Atypical presentations included seizures or seizure-like activity (3 [6%]), severe odynophagia (1 [2%]), loss of smell (3 [6%]), recurrent pneumothorax (1 [2%]), and hepatitis in a patient who received a liver transplant for whom the donor was found to be SARS-CoV-2–positive posttransplant (1 [2%]). One infant had seizure-like activity and an abnormal electroencephalogram finding; the cerebrospinal fluid testing result for SARS-CoV-2 using a research PCR assay was negative. Gastrointestinal tract symptoms were observed for 7 patients (14%). Three of these patients only had gastrointestinal tract symptomatology (eg, abdominal pain, vomiting), triggering evaluations for appendicitis. Codetection of other respiratory viruses were found for 4 patients (rhinovirus/enterovirus [2 (4%)], rhinovirus/enterovirus/adenovirus [1 (2%)], and human metapneumovirus [1 (2%)]). Bacterial coinfections during hospitalization included bacteremia (3 [6%]), suspected bacterial pneumonia (9 [18%]), urinary tract infections (5 [10%]), skin and soft tissue infections (3 [6%]), and streptococcus pharyngitis (1 [2%]). Of the patients with bacteremia, 1 was admitted to receive a course of antibiotic therapy for Klebsiella pneumoniae bacteremia diagnosed at another hospital, 1 had methicillin-sensitive Staphylococcus aureus bacteremia on admission, and 1 developed methicillin-resistant S aureus and Enterococcus faecalis bacteremia during hospitalization.
Most patients were discharged (38 [76%]) with a median length of stay of 3 days (range, 1-30 days). Approximately one-third of the hospitalized patients (16 [32%]) required some form of respiratory support (eg, nasal cannula, NIPPV, or mechanical ventilation). The NIPPV was the maximum respiratory support used for 3 patients (6%) and mechanical ventilation was required for 9 patients (18%). The median time to intubation from symptom onset was 7 days (range, 3-11 days). Two patients had sudden cardiac arrest (pulseless electrical activity) on hospital days 3 and 5, respectively, 1 of whom died. Both cardiac arrests were preceded by a prolonged period of severe hypoxia. Mucus plugging and/or thromboembolism are being considered as potential etiologies.
The most prevalent comorbidity was obesity, seen for 11 patients (22%). An additional 8 patients (16%) had overweight. The distributions of comorbidities in children with severe disease (mechanically ventilated) vs nonsevere disease are summarized in Table 1 . Obesity was significantly higher in the severe disease group. Infants were less severely affected. Disease severity was not significantly higher in immunocompromised patients. One previously healthy child who required mechanical ventilation was found on whole-exome sequencing to be heterozygous for a variant of uncertain significance; further workup is ongoing.
On admission, the white blood cell counts were generally normal (median, 7.6 × 10 3 /μL; IQR, 4.6-11.4 × 10 3 /μL), with lymphopenia (median ALC, 1201/μL; IQR, 600-2084/μL) seen in 36 patients (72%). Absolute lymphocyte count at admission did not differ significantly in patients with and without severe disease (median 1201/μL vs 1199.5/μL). Thrombocytopenia was only seen in 7 patients (14%; median, 248 × 10 3 /μL; IQR, 18-733 × 10 3 /μL). Inflammatory markers (C-reactive protein: median, 8.978 mg/dL vs 0.64 mg/dL [to convert to milligrams per liter, multiply by 10]; procalcitonin: median, 0.31 ng/mL vs 0.17 ng/mL) were significantly elevated at admission for patients with severe disease ( P < .001 for both). Patients who required mechanical ventilation were characterized by high mean peak inflammatory markers (ferritin, C-reactive protein, procalcitonin, D-dimer, and IL-6) ( Table 2 ).
Chest radiographs were performed for 36 patients (72%). Findings included bilateral patchy or ground glass opacities (25 [69%]), pleural effusion (9 [25%]), focal consolidation (8 [22%]), and pneumothorax (2 [5%]). Five patients without respiratory symptoms had bilateral patchy infiltrates on imaging. Three immunocompromised patients received chest computerized tomography; 1 patient had unilateral multilobar pneumonia but did not develop lower respiratory tract symptoms or a supplemental oxygen requirement.
Hydroxychloroquine was administered to 15 patients (30%), typically at a dose of 6.5 mg/kg, twice daily, for 2 doses, then 6.5 mg/kg, once daily, for 4 doses. Therapy was reserved for patients with escalating oxygen requirements and respiratory distress. In 3 patients, hydroxychloroquine was used as a bridge to remdesivir therapy. Of the 15 patients prescribed hydroxychloroquine, 2 patients required drug discontinuation because of adverse events (blurry vision [1] and severe abdominal pain [1]); both resolved their symptoms with drug discontinuation. One patient had the drug discontinued because of a new diagnosis of Brugada syndrome associated with prolonged QTc of more than 500 milliseconds. One patient who received hydroxychloroquine died on hospital day 5. Remdesivir was administered to 4 patients (3 obtained through a compassionate use mechanism and 1 enrolled through a clinical trial). No adverse events were observed, with 1 patient discharged and 3 still hospitalized. Tocilizumab was administered to 1 patient with elevated IL-6 levels receiving extracorporeal membrane oxygenation who developed methicillin-resistant S aureus and E faecalis bacteremia 10 days after administration. Two patients receiving mechanical ventilation with elevated inflammatory markers received methylprednisolone, 1 mg/kg, once daily, for 5 to 7 days.
On readmission 15 and 27 days after their first SARS-CoV-2 tests, 2 immunocompetent patients were retested and had positive results. A test positivity sequence demonstrating potential false-negative results for 1 of these patients is illustrated in Figure 2 . Two immunocompromised patients were retested 14 and 23 days after their first detection and still had positive results. One patient with fever and fatigue at the time of admission initially had a negative test result but was retested 7 days later and had positive results for SARS-CoV-2. Nasopharyngeal viral load values as represented as the PCR cycle threshold values were available for 1 immunocompromised infant, and these values remained high and unchanged with sequential testing 7 days apart, although the patient had minimal lower respiratory tract disease.
In this article, we report the epidemiology, clinical manifestations, and outcomes of pediatric patients hospitalized with COVID-19 at a children’s hospital in New York City. Thus far, the small number of cases are consistent with data suggesting that children have less severe disease requiring hospitalization compared with adults. 5
Data from China suggested that children were infected early during the community transmission phase of the pandemic. 6 Thus, having a low threshold of suspicion for SARS-CoV-2 testing and adequate test supplies are crucial for mitigation. Consequently, our testing strategy, which is similar to many other centers, has rapidly evolved from using strict CDC person-under-investigation criteria to universal screening of admissions. Most of the patients were clustered within an incubation period starting from citywide NPI implementation, and decreasing numbers of cases could indicate efficacy of these measures. Many patients had household contacts with illness at the time of admission, suggesting household transmission. However, only a few of these contacts had laboratory confirmation of SARS-CoV-2. Expansion of ambulatory testing and easier access must be implemented before decreasing NPIs in communities with high rates of COVID-19. Two parents developed symptoms during their child’s admission, so vigilance for the emergence of symptoms in visitors remains crucial to minimize staff exposures.
Lower respiratory tract symptoms and fever were common manifestations in the study patients. However, we noted diverse COVID-19 presentations. Gastrointestinal symptoms were a feature in many patients, as described in adults. 13 The constellation of abdominal pain and vomiting was seen in 3 patients (6%), and whether gastrointestinal tract inflammation can trigger a clinical picture consistent with appendicitis in children should be further defined. Seizures or seizure-like activity also occurred. Neurologic manifestations have been documented in adults with COVID-19. 14 Whether these atypical presentations result from viral replication vs an immune phenomenon remains to be elucidated. The presence of viral and bacterial coinfections can complicate decisions for pediatric and infection control practitioners when labeling a detection of SARS-CoV-2 as COVID-19.
The significance of obesity as an independent risk factor for severity is now being increasingly described in adult studies of COVID-19, 15 so it was interesting that many of the hospitalized patients in this study had obesity and/or overweight. Obesity was the most significant factor associated with mechanical ventilation in children 2 years and older. Contrary to some previous reports, 8 infants seemed largely spared severe manifestations. Most patients had 1 or more comorbidities. An associated observation is the lack of disproportionate effect on immunosuppressed patients, most of whom remained stable throughout their illness.
As described previously, lymphopenia was the most consistent laboratory finding, 16 but it did not have prognostic value. However, significantly elevated inflammatory markers suggestive of a hyperinflammatory state were seen in patients with severe disease, as described in adults. 17 Radiographic findings were consistent with previous reports, 18 but in some cases, findings were observed without significant symptoms.
Therapy for COVID-19 remains experimental. We reserved antiviral therapy for patients who required escalating respiratory support, usually with NIPPV or higher. The safety of hydroxychloroquine is debated, 19 , 20 and in our limited experience, we encountered issues that halted course completion for 20% of patients receiving hydroxychloroquine. Remdesivir administration was not associated with any adverse events. However, the small sample size does not allow inference regarding efficacy. The role of immune modulators and steroids remains controversial and should be addressed through clinical trials.
The dynamics of viral shedding complicate IPC for SARS-CoV-2. The few retested patients showed prolonged positivity even when immunocompetent. Prolonged SARS-CoV-2 detection after symptom resolution has been described, 21 which complicates decision-making around discontinuing isolation or home quarantine. Even more concerning is repeated positivity after multiple interval negative results, as seen in 1 patient. Encouragingly, as rates of community transmission have decreased, our admission screening positivity rates remain low. Only 1 health care–associated case has been identified to date at our center, hopefully attributable to effective hospital IPC practices, including universal masking, universal symptom checks of staff and visitors, and expanded personal protective equipment access.
This study has limitations. Our hospital predominantly serves a Hispanic community, so findings may not be generalizable to other populations. The small sample size of this descriptive study may additionally limit generalizability. We may not have captured all comorbidities or signs and symptoms in this retrospective study. In the setting of widespread community transmission, SARS-CoV-2 detection could also be coincidental with other diagnoses and detection could represent previous illness with prolonged shedding, mild symptoms, and/or asymptomatic infection creating misclassification.
As community transmission of SARS-CoV-2 continues, hospitals must be alert to variable presentations of COVID-19, test liberally, attempt early risk stratification of patient populations, and have well-established clinical and IPC protocols. Therapeutic considerations need to consider the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation.
Accepted for Publication: May 13, 2020.
Corresponding Author: Philip Zachariah, MD, MSc, Department of Pediatrics, Columbia University Irving Medical Center, 622 W 168th St, PH 4 West Room 473, New York, NY 10032 ( [email protected] ).
Published Online: June 3, 2020. doi:10.1001/jamapediatrics.2020.2430
Correction: This article was corrected on June 21, 2021, to add a supplement that lists of all the nonauthor collaborators.
Author Contributions: Dr Zachariah had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Zachariah, Johnson, Camille Halabi, Giordano, Schweickert, Babineau, Fenster, Orange, Saiman.
Acquisition, analysis, or interpretation of data: Zachariah, Johnson, Camille Halabi, Ahn, Sen, Fischer, Banker, Giordano, Manice, Diamond, Sewell, Carter, Fenster, Orange, McCann, Kernie, Saiman.
Drafting of the manuscript: Zachariah, Camille Halabi, Ahn, Saiman.
Critical revision of the manuscript for important intellectual content: Zachariah, Johnson, Camille Halabi, Sen, Fischer, Banker, Giordano, Manice, Diamond, Sewell, Schweickert, Babineau, Carter, Fenster, Orange, McCann, Kernie, Saiman.
Statistical analysis: Zachariah, Giordano.
Administrative, technical, or material support: Zachariah, Johnson, Camille Halabi, Fischer, Giordano, Manice, Diamond, Schweickert, Carter, Fenster, Orange, McCann.
Supervision: Zachariah, Babineau, Fenster, Orange, Kernie, Saiman.
Conflict of Interest Disclosures: Dr Orange reported personal fees from Takeda and ADMA Biologics and being a member of the scientific advisory board for Gigagen outside the submitted work. Dr Saiman reported grants from Merck, the CF Foundation, the National Institute of Allergy and Infectious Diseases, and the Bill and Melinda Gates Foundation and serving on the scientific advisory boards of Merck and AstraZeneca outside the submitted work. No other disclosures were reported.
Group Information: The Columbia Pediatric COVID-19 Management Group members are listed in Supplement 1 .
Additional Contributions: We acknowledge the extraordinary work of physicians, nurses, respiratory therapists, and all staff at Columbia University Irving Medical Center, Weill Cornell Medicine, and NewYork-Presbyterian Hospital. Specifically, we would like to thank our nursing leadership: Tammy Compagnone, DNP, RN, Donna Johnson, MS, MBA, RN, Kenya Robinson, MSN, RN, Vepuka Kauari, MSN, RN, and Bernadette Khan, DNP, RN (NewYork-Presbyterian Hospital). We thank the families of the children included in this study. None of these individuals received compensation for their contributions.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Novel coronavirus 2019 (COVID-19)
A case report and review of treatments.
Editor(s): Saranathan., Maya
a Department of Medicine, Hackensack Meridian Jersey Shore University Medical Center Neptune
b Department of Medicine, Hackensack Meridian School of Medicine at Seton Hall University Nutley
c Department of Pulmonology and Critical Care, Hackensack Meridian Jersey Shore University Medical Center Neptune, NJ, USA.
∗Correspondence: Steven Douedi, Jersey Shore University Medical Center, Neptune, NJ 07753 (e-mail: [email protected] ).
Abbreviations: ARDS = acute respiratory distress syndrome, CoV = coronavirus, COVID-19 = novel coronavirus 2019, CVVHD = continuous veno-venous hemodialysis, ED = emergency department, FiO2 = fraction of inspired oxygen, ICU = intensive care unit, MERS-CoV = Middle East respiratory syndrome coronavirus, PCR = polymerase chain reaction, PEEP = positive end-expiratory pressure, RSV = Respiratory syncytial virus, SARS-CoV = severe acute respiratory syndrome coronavirus, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2.
How to cite this article: Douedi S, Miskoff J. Novel coronavirus 2019 (COVID-19): a case report and review of treatments. Medicine . 2020;99:19(e20207).
The authors have no conflicts of interests to disclose.
This manuscript is a unique submission and is not being considered for publication by any other source in any medium. Further, the manuscript has not been published, in part or in full, in any form.
The patient's next of kin provided consent for this manuscript to be published.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
This is an open access article distributed under the Creative Commons Attribution License 4.0 (CCBY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. http://creativecommons.org/licenses/by/4.0
Rationale:
Novel coronavirus 2019 (COVID-19) also known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an enveloped, non-segmented positive-sense RNA virus belonging to the beta-coronaviridae family. This virus is known to cause severe bilateral pneumonia and acute respiratory distress syndrome (ARDS) which can lead to difficulty breathing requiring mechanical ventilation and intensive care unit management.
Patient concerns:
A 77-year-old female with a history of hypertension and hyperlipidemia who presented as a transfer to our hospital facility with worsening fevers, cough, and respiratory distress.
Diagnosis:
Chest X-rays revealed bilateral infiltrates worse at the lung bases and CT scan of the chest showed bilateral ground-glass opacities consistent with COVID-19. While our testing revealed a negative COVID-19 result at our institution, the result at a previous hospital returned a positive result.
Interventions:
She was being treated aggressively in the intensive care unit with high dose intravenous ascorbic acid, hydroxychloroquine, and anti-interleukin-6 monoclonal antibody. She also received a loading dose of remdesivir however was unable to complete the course due to organ failure and requirement of vasopressors for hemodynamic stability.
Outcomes:
She remained critically ill and was eventually placed on comfort care as per the family's wishes and passed away.
Lessons:
With a rapidly growing death rate and more than 200,000 confirmed cases worldwide, COVID-19 has become a global pandemic and major hit to our healthcare systems. While several companies have already begun vaccine trials and healthcare facilities have been using a wide-range of medications to treat the virus and symptoms, there is not yet an approved medication regimen for COVID-19 infections. The alarming increase in cases per day adds additional pressure to find a cure and decrease the global health burden and mortality rate.
1 Introduction
The novel coronavirus 2019 (COVID-19) also known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an enveloped, non-segmented positive-sense RNA virus belonging to the beta-coronaviridae family. [1] COVID-19 has been found to be the cause of severe pneumonia and acute respiratory distress syndrome (ARDS) with a significantly high mortality rate. [2] According to the World Health Organization, there are 207,855 confirmed cases and 8648 deaths from COVID-19 as of March 19, 2020 and rapidly increasing. [3] Originating from bats like other virulent coronavirus (CoV) strains such as severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV), COVID-19 has become the focus of the medical world and the pandemic of 2020. [1,4] We present a case of elderly female presenting with fever, cough, and shortness of breath found to be positive for COVID-19 and started on high-dose IV ascorbic acid, anti-interleukin-6, hydroxychloroquine, and remdesivir requiring high ventilator settings and eventually requiring vasopressors and continuous veno-venous hemodialysis (CVVHD).
2 Case presentation
A 77-year-old Middle-Eastern female with a medical history of hypertension and hyperlipidemia presented to the emergency department (ED) from a day care facility apartment where 2 people at the facility have tested positive for COVID-19 but she did not have any direct contact with these individuals. About 5 days before admission the patient developed a fever with a temperature of 102°F at home, and went to her primary medical doctor who sent her to the ED. In the ED she was found to have bilateral opacities on chest X-ray and had continued intermittent fevers with generalized weakness, cough, lethargy, and dyspnea and was sent for testing for COVID-19 then transferred to our facility for further management. In our facility, her temperature was 101.7°F, blood pressure 148/76 mm Hg, heart rate of 99 beats per minute, respiratory rate of 18 per minute, and oxygen saturation of 93% on room air. Physical exam was significant for a dry cough and bilateral rales on auscultation of the lung fields bilaterally but was unremarkable otherwise. A chest X-ray ( Fig. 1 ) was performed showing bilateral opacities throughout the lung fields with predominance of the lower lung lobes she was admitted for possible pneumonia with isolation precautions for suspected COVID-19 and was started on oxygen via nasal cannula and on 1-gram ceftazidime intravenously every 8 hours and 500 mg azithromycin orally daily. CT scan of the chest ( Fig. 2 ) was performed showing bilateral ground glass appearance throughout the lung with predominance in the peripheral lower lobes. Respiratory viral panel was sent including a repeat COVID-19 test ( Table 1 ). All results came back negative however the patient's condition deteriorated 2 days after admission to our facility, and she became hypoxic to 85% oxygen saturation while on nasal cannula and remained spiking fevers up to 103.4°F. She was intubated and transferred to the intensive care unit (ICU) for further management and was switched to ceftriaxone 1 g intravenously daily and azithromycin 500 mg via orogastric tube daily and was started on hydroxychloroquine 400 mg loading dose followed by 200 mg twice daily for a 7-day course. She required 100% fraction of inspired oxygen (FiO2) and a positive end-expiratory pressure (PEEP) of 12 to maintain an oxygen saturation of >90%. 12 hours later, the COVID-19 test from the initial facility returned positive results. On day 3 of hospitalization she was started on 6 g of IV ascorbic acid twice daily and given one dose of 8 mg per kg (567 mg) of tocilizumab, an anti-interleukin-6 monoclonal antibody. Due to a shortage of vitamin C in the hospital, her dose was decreased to 1 g IV daily on the 6th day of hospitalization and she was given another dose of tocilizumab. On day 7, her PEEP increased from 12 to 16 due to worsening oxygen saturation and increased requirement despite 100% FiO2. Due to severe ARDS, the decision was made to prone the patient for 18 hours a day. She completed her course of antibiotics and hydroxychloroquine but remained on vitamin C and zinc. Approval for remdesivir was obtained from Gilead Sciences Inc and she was given a loading dose of 200 mg on day 10 and due to worsening oxygen saturation her PEEP was again increased to 18. On day 11, the patient was unable to tolerate being prone due to significant desaturation to 65% on pulse oximetry and remained supine. She eventually required levophed for maintenance of hemodynamic stability and her creatinine increased from her baseline of 0.5-0.6 since admission until day 10 to 2.65 on day 12. For this reason, remdesivir was discontinued and nephrology was consulted and recommended CVVHD on day 13. On day 14 her PEEP requirement again increased to 20 while on 100% FiO2 to maintain an oxygen saturation >90%. Her condition remained critical while being aggressively managed in the ICU and ultimately the patient's family decision was to pursue comfort measures and the patient passed away.

3 Discussion
COVID-19 is the cause of severe viral pneumonia rapidly leading to ARDS. In a case series of 135 patients, Wan et al reported 88.9% of patients presented with a fever and 76.5% had a cough. [5] Fatigue and myalgias (32.5%), headache (17.7%), and dyspnea (13.3%) were less commonly reported. [5] These symptoms were also found on presentation with our patient. While the COVID-19 tests were pending, the CT scan of the chest provided valuable information as it met the trend of findings in infected patients. Wan et al obtained CT scans on all patients in their study and found bilateral involvement and multiple patchy or ground glass appearance to be the primary finding. [5] Huang et al found similar findings where 98% of CT scans obtained had bilateral involvement and multilobular consolidations. [6] These findings on CT scans are not unusual for a viral pneumonia. Influenza A (H1N1) was first found to cause a pandemic in 2009, a retrospective review of 92 patients by Çörtük et al found 69.6% of patients with H1N1 had bilateral patchy pneumonic infiltrates and 41.3% had bilateral ground glass opacities. [7] While the lack of rapid testing for COVID-19 has caused a delay in diagnosis, perhaps the use of CT scans could provide an increased suspicion of COVID-19 infection leading to earlier treatment and management.
Our patient presented in this case received treatment with vitamin C and zinc, both of which are known to improve the human immune system and aid in shortening the duration of and improving outcomes in respiratory infections including pneumonia. [8,9] In addition to vitamin and mineral supplements, hydroxychloroquine and azithromycin have obtained a large amount of attention for the treatment of COVID-19. Hydroxychloroquine, a well-known anti-malarial and auto-immune medication, is relatively inexpensive and has been extensively studied in the treatment for COVID-19. Studies have suggested hydroxychloroquine can interfere with glycosylation of the coronavirus receptors and increase endosomal pH thus inhibiting viral fusion and decreasing viral load. [10,11] Gautret et al reported a synergistic effect using hydroxychloroquine and azithromycin in viral elimination and decreasing viral load. [12] Despite this evidence, the use of hydroxychloroquine for viral infections has been questioned. Roques et al reported a study using chloroquine in Chikungunya virus reporting cytokines were reduced causing the adaptive immune response to be delayed, exacerbating fever, and unchanged suppression of viral load. [13] While further studies are in need to provide concrete evidence on the use of hydroxychloroquine, clinical trials from China have already shown promising results for COVID-19 and several countries around the world have begun using these medications. Tocilizumab, a recombinant humanized anti-interleukin-6 receptor monoclonal antibody, has been extensively used in auto-immune conditions such as rheumatoid arthritis. [14] With this monoclonal antibody, interleukin-6 function is blocked and hence the differentiation of T helper cells and B cells into immunoglobulin-secreting cells are inhibited. [14] The cytokine storm observed in patients with COVID-19 has been difficult to control and manage leading to increased mortality, tocilizumab therefore helps decrease the immune response and the resulting damage caused by cytokines. [6,15] While still not approved in the United States, tocilizumab has thus far shown promising results in clinical trials. [15]
Other treatments for COVID-19 have also emerged and have thus far shown promising results in ongoing clinical trials. Of these, remdesivir (GS-5734) and favipiravir (T-705) have become the center of attention. Remdesivir is an adenosine analog that incorporates into viral RNA causing premature termination. [10,14] It has been found effective at inhibiting viral replication in Ebola, SARS-CoV, and MERS-CoV infections. [10,16,17] Favipiravir, an RNA-dependent RNA polymerase inhibitor, has already obtained approval for the treatment of COVID-19 in China on February 15th, 2020. [18] Studies have shown favipiravir inhibited RNA polymerase activity and thus prevented replication of RNA viruses like COVID-19 with minimal side effects. [18] Remdesivir (GS-5734, Gilead Sciences Inc.) is currently under several clinical trials and all of its side effects have not yet been defined. In our patient, within 2 days of starting remdesivir our patient had worsening renal function eventually requiring CVVHD and vasopressors thus preventing further treatment with the medication. While our patient was critically ill in the ICU, it is not known if this medication was the cause for further decompensation due to kidney injury. Further studies and clinical trials are required to fully understand the role of remdesivir and other medications in COVID-19 infected patients.
4 Conclusion
COVID-19 is a serious infection that has led to thousands of cases of severe pneumonia, ARDS, and even deaths across the globe. As of now there are no approved treatments for this viral pandemic. While several medications have shown to be effective in clinical trials, further studies are needed to establish dosing, treatment course, and side effects of these medications. As the number of cases and deaths continue to increase in the world, the race to develop faster testing modalities to rapidly diagnose and manage these patients earlier continues to be the focus of the global healthcare system.
Author contributions
Conceptualization: Steven Douedi, Jeffery Miskoff.
Writing – original draft: Steven Douedi.
Writing – review & editing: Steven Douedi, Jeffery Miskoff.
- Cited Here |
- Google Scholar
acute respiratory distress syndrome; coronavirus; novel coronavirus 2019; infection; respiratory; severe acute respiratory syndrome coronavirus 2
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Clinical remission of a critically ill covid-19 patient treated by human..., acquired reactive perforating collagenosis: a case report and review of the..., covid-19 with cystic features on computed tomography: a case report.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 25 April 2023
An interpretable hybrid predictive model of COVID-19 cases using autoregressive model and LSTM
- Yangyi Zhang 1 ,
- Sui Tang 1 &
Scientific Reports volume 13 , Article number: 6708 ( 2023 ) Cite this article
2868 Accesses
6 Citations
10 Altmetric
Metrics details
- Computer science
- Scientific data
The Coronavirus Disease 2019 (COVID-19) has had a profound impact on global health and economy, making it crucial to build accurate and interpretable data-driven predictive models for COVID-19 cases to improve public policy making. The extremely large scale of the pandemic and the intrinsically changing transmission characteristics pose a great challenge for effectively predicting COVID-19 cases. To address this challenge, we propose a novel hybrid model in which the interpretability of the Autoregressive model (AR) and the predictive power of the long short-term memory neural networks (LSTM) join forces. The proposed hybrid model is formalized as a neural network with an architecture that connects two composing model blocks, of which the relative contribution is decided data-adaptively in the training procedure. We demonstrate the favorable performance of the hybrid model over its two single composing models as well as other popular predictive models through comprehensive numerical studies on two data sources under multiple evaluation metrics. Specifically, in county-level data of 8 California counties, our hybrid model achieves 4.173% MAPE, outperforming the composing AR (5.629%) and LSTM (4.934%) alone on average. In country-level datasets, our hybrid model outperforms the widely-used predictive models such as AR, LSTM, Support Vector Machines, Gradient Boosting, and Random Forest, in predicting the COVID-19 cases in Japan, Canada, Brazil, Argentina, Singapore, Italy, and the United Kingdom. In addition to the predictive performance, we illustrate the interpretability of our proposed hybrid model using the estimated AR component, which is a key feature that is not shared by most black-box predictive models for COVID-19 cases. Our study provides a new and promising direction for building effective and interpretable data-driven models for COVID-19 cases, which could have significant implications for public health policy making and control of the current COVID-19 and potential future pandemics.
Similar content being viewed by others
A novel bidirectional LSTM deep learning approach for COVID-19 forecasting
Improving prediction of COVID-19 evolution by fusing epidemiological and mobility data
Spatio-temporal prediction of the COVID-19 pandemic in US counties: modeling with a deep LSTM neural network
Introduction.
The coronavirus disease 2019 (COVID-19) pandemic has posed a severe threat to global health and economy while producing some of the richest data we have ever seen in terms of infectious disease tracking. The quantity and quality of data placed epidemic modeling and forecasting at the forefront of worldwide public policy making. Compared to previous infectious diseases, COVID-19 shows special transmission characteristics, yielding significant fluctuations and non-stationarity in the new COVID-19 cases. This poses grand challenges in effective prediction, and, on the other hand, draws attention of the global community to epidemic tracking and prediction.
In the last three years, various models and methods have been developed to predict COVID-19 cases (see survey in 1 and references therein). These models can be roughly grouped into two categories: mechanistic models and data-driven models. The mechanistic models aim at directly characterizing the underlying mechanisms of COVID-19 transmission. Typical examples of mechanistic models are based on differential equations, such as the compartmental models SIR and SEIR 2 , 3 , 4 , 5 . The data-driven models formulate the prediction of the COVID-19 cases primarily as a regression problem and exploit fully data-adaptive approaches to understand the functional relationship between COVID-19 cases with a set of observable variables. Data-driven models include classical statistical models such as Autoregressive models (AR) 6 , 7 , 8 , Support Vector Machine (SVM) 9 , 10 , 11 , and the deep learning models 12 , 13 , 14 , 15 , 16 , 17 , 18 . In this paper, we will focus on data-driven models.
An Autoregressive model expresses the response variable as a linear function of its previous observations 19 . Its simple structure and strong interpretability are found to be powerful in capturing short-term changing trends in time series. AR models have been applied in various application fields, including infectious decease modeling 20 , 21 . However, they may fail to capture the highly nonlinear patterns and long-term effects in the data-generating dynamics. On the other extreme of the predictive model complexity spectrum, deep learning models, particularly LSTM 22 , have demonstrate impressive power in capturing complex dependence structures in sequential data. LSTM has been used to achieve the best-known results for many problems on sequential data. However, a well-known limitation of the deep learning models is the short of interpretability due to their black-box nature. This lack of interpretability prevents people from drawing useful conclusions from the model outputs, thus hinders effective policy making 23 , especially in crucial fields such as public health. This observation motivates us to consider a hybrid model in which the two seemingly distinct types of models join forces while maintaining both good predictive power and certain interpretability.
In this paper, we propose such a hybrid model that additively combines the LSTM and the AR model for the task of COVID-19 cases prediction. The proposed hybrid model is formalized as a neural network with an architecture that connects an AR model and a LSTM block, and the relative contribution of these two component models is decided in a totally data-adaptive way in the training procedure. To demonstrate the predictive power of the proposed hybrid model, we consider both county-level and country-level data. Specifically, in 8 counties in the state of California, USA, and 7 other different countries (results available in the Supplementary Material ), our method performs favorably compared with either AR or LSTM model alone, as well as other commonly-used predictive models under various evaluation metrics. All codes are accessible through links on the reference page 24 .
In addition to the predictive accuracy, the importance of predictive models’ interpretability has been discussed in plenty of previous works 23 , 24 , 25 , 26 , 27 . A higher model interpretability facilitates human’s ability to understand its predictions, and thus promotes bias detection and other factors that contribute to policy making. Specifically, we demonstrate how the coefficients from the AR part of the trained hybrid model shed light onto understanding the underlying disease transmission mechanism, and thus could help to predict its prevalence trends, and to inform public health policy makers to improve pandemic planning, resource allocation, and implementation of social distancing measures and other interventions. A long-term mission of this paper is to stretch the application of hybrid models beyond COVID-19 forecasting: toward other fast-moving epidemics and cases that require accurate prediction and interpretability.
Although in this paper we focus on confirmed cases prediction, we note that the proposed framework can be easily extended to tackle other COVID-19 or more general epidemiological tasks (e.g., hot spot prediction). Furthermore, the proposed method has its own research significance from a methodological perspective. For example, it raised the open questions on studying its theoretical guarantees, mathematical quantification of prediction, and interpretability.
Related work
Recently, numerous studies have employed machine learning techniques to investigate various tasks on COVID-19 and achieved impressive results. Examples include using deep learning to detect COVID-19 through CXR images and predicting death status based on food categories to recommend healthy foods during the pandemic 28 , 29 , 30 . In light of these advances, our research focuses on predicting confirmed cases of COVID-19.
In this section, we provide a more detailed review of data-driven models that formulate the prediction problem as a regression problem. Regression-based models, including simple AR models and more complex models such as Random Forest, Gradient Boosting, and CNN-LSTM, have been widely used for COVID-19 prediction. For example, Mumtaz et al. 31 used ARIMA to predict the daily confirmed cases in European countries, while Yesilkanat 32 used a Random Forest model to predict the number of cases and deaths. Muhammad et al. 33 used a CNN-LSTM model to predict the number of confirmed cases and deaths in Nigeria, South Africa, and Botswana. We summarize a list of recent work from year 2020 to 2022 in Table 1 .
One advantage of these models is that they do not require a priori knowledge of the disease dynamics and can capture rich relationships in the data. They have been shown to be effective in predicting COVID-19 cases in various regions around the world. However, COVID-19 data displays rich variability, and therefore a single predictive model may not be sufficient and has its own limitations. For example, one major disadvantage of ARIMA models is that they may not be able to capture non-linear patterns in the data, which can lead to inaccurate predictions. On the other hand, more complex models such as Random Forest and CNN-LSTM may suffer from overfitting, where the model becomes too specialized to the training data and cannot generalize well to new data. These complex models may also lack interpretability, making it difficult to understand the factors driving the predictions and thus provide little to none guidance to actual public health policy making.
Hybrid predictive models that combine different regression models may offer the best of both worlds by capturing both linear and non-linear patterns in the data while maintaining some degrees of interpretability. The idea is to decompose a model into different components that are designed to capture specific characteristics of the data. It has proven to be an effective way of improving empirical predictions in various applications, including those in COVID-19 prediction 34 , 35 , 36 , 37 , 38 .

Comparison to previous works on hybrid modeling
The idea of using an additive combination of AR models (or more generally, ARIMA models) with LSTMs has recently appeared in the literature for time series forecasting, with applications in gas and oil well production and sunspot monitoring 39 , 40 . However, there is a significant difference between our approach and previous methods: our approach trains the two components in the model jointly, while previous hybrid modeling techniques take a sequential approach to training. Specifically, Zhang 41 proposed a hybrid model of ARIMA and artificial neural networks, aiming to capture more patterns in the data and improve forecasting performance. The preprocessed data is used to fit an ARIMA model first, before the residual term is used as input to train a neural network model. Fan et al. 39 followed a similar procedure, using an ARIMA model and an LSTM model. The logistics of these methods is to use an ARIMA model to capture the linear pattern of the data first and rely on the neural networks capture the non-linear pattern in the residuals. The main goal of these previous works is to explore whether a hybrid model produces better performance than the single models.
In our study, we design a general network architecture that includes both an AR part and an LSTM part additively and trains the entire architecture jointly by minimizing the empirical risk. By doing so, we do not arbitrarily give preference to any of the two additive components. Instead, the relative weights of the interpretable AR part and the predictive LSTM part are determined fully by the data.
In summary, our contributions can be summarized as:
Development of a novel approach to hybrid modeling for COVID-19 cases prediction: we have designed a general network architecture that combines AR and LSTM models additively and trains the entire architecture jointly, allowing the relative weights of the interpretable AR part and the predictive LSTM part to be fully determined by the data. This approach is a departure from traditional sequential modeling approach and has the potential to contribute to the literature of sequential data prediction.
Extensive numerical studies on data sets from two sources that displays a rich variety of variability: we have shown that the proposed hybrid model demonstrates better forecasting performance than single models. This finding is important as it shows that the hybrid model is an effective way to combine the strengths of different modeling techniques and can be used as a framework for future research.
Exploration of interpretability: we have also explored the interpretability of the hybrid model, which is an important contribution as it allows for a better understanding of the model and can lead to improved decision-making based on the model’s output. This contribution enhances the practical applicability of our proposed hybrid model.
In this section, we first overview the two building blocks of our additive hybrid model, namely the AR and the LSTM model, and their relative advantages. Then we present our hybrid model which combines these two building blocks additively, and we intuitively elaborate why it is better than the two individual components.
Autoregressive (AR) models
In time series, we often observe associations between past and present values. For example, by knowing the price of a stock in the past few days, we can often make a rough prediction about its value tomorrow. AR is a simple model that utilized this empirical observation and can yield very accurate prediction in certain applications. It represents the time series values using linear combination of the past values. The number of past values used is called the lag number and often denoted by p . Let \(\epsilon _t\) denote the Gaussian noise at time t with mean 0 and variance \(\sigma ^2\) . The structure equation of AR(p) model can be represented as
where \(a_0\) is the intercept, and \(a_1,\cdots ,a_p\) represent the coefficients. AR model is often effective on stationary data. To ensure stationarity, a common trick is to apply the differencing operation on the time series. A time series value at time t that has been differenced once, \(Y^{(1)}\) , is defined as follows:
and higher order differencing operation can be defined recursively. However, an AR model is not sufficient to capture the non-linear dependence structure, which is found to be an important feature of the COVID-19 data, indicated by Fig. 1 . A purely AR based model is thus often insufficient for the task of COVID-19 cases prediction.
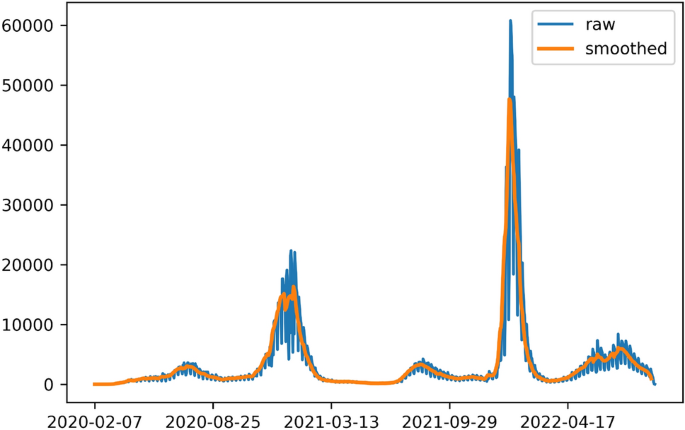
An example of visualizing daily observations, where blue line represents the data before smoothing, orange line represents data after smoothing. The data is collected from the Los Angeles county.
Long short term memory networks (LSTM)
RNN (Recurrent Neural Network) 52 is known to suffer from the long term dependency problem: as the network grows larger through time, the gradient decays quickly during back propagation, making it impossible to train RNN models with long unfolding in time. To solve this problem, Hochreiter and Schmidhuber (1997) introduced a special type of RNN called LSTM with a proper gradient-based learning algorithm 22 .
We employ a LSTM regression model, which is represented as
where we use \(Y_{t-1},...,Y_{t-p}\) as the sequential input data; G represents the neural network architecture shown in Supplementary Fig. 1 and \(\theta\) represents the weight parameters in neural networks.
The core concepts of a LSTM cell are the cell states and the associated gates, as illustrated in Supplementary Fig. 2 . The cell state \(C_{t-1}\) at time step \(t-1\) acts as a transport highway that transfers relative information all the way down the sequence chain, which intuitively characterizes the “memory” of the network. The cell states, in principle, carry relevant information throughout the processing of the sequence. So even information from the earlier time steps can make its way to later time steps, reducing the effects of short-term memory. The Forget Gate decides what information should be kept. The Input Gate decides what information is to be added from the current step and update the cell state \(C_t\) at time step t . The Output Gate determines what the next hidden state \(h_t\) should be. The four gates comprise a fully connected feed forward neural network.
To achieve optimal prediction results using LSTM model, it is crucial to have a careful hyperparameter tuning, including the choice of units (dimension of the hidden state), the number of cells (i.e. the number of time steps), and layers. This is usually a difficult task in practice. For example, few LSTM cells are unlikely to capture the structure of the sequence, while too many LSTM cells might lead to overfitting. However, just like other neural networks, a well-known limitation of LSTM is its lack of interpretability 23 .
The hybrid model
As discussed above, both AR and LSTM have their relative strength and limitations in their prospective domains. We propose to combine the two models additively into one single hybrid model, which is expressed as
where p is the lag number and \(\alpha\) weights the contribution of two components: by tuning the value of \(\alpha\) , one can strike a balance between the prediction given by AR and LSTM parts, and thus a prediction of linear and nonlinear signals.
We illustrate the structure of the hybrid model in Fig. 2 . The hybrid model is characterized as one neural network architecture where the two composing models are added through the last layer. The AR component captures the linear relationship in time series and the LSTM component would describe the nonlinear patterns. In section “Training” of the Supplementary Material , we show how to train the weights in each of the two components in a fully data-adaptive manner by minimizing the empirical risk. We will compare the contribution of the hybrid model’s AR component and LSTM component in section Results .
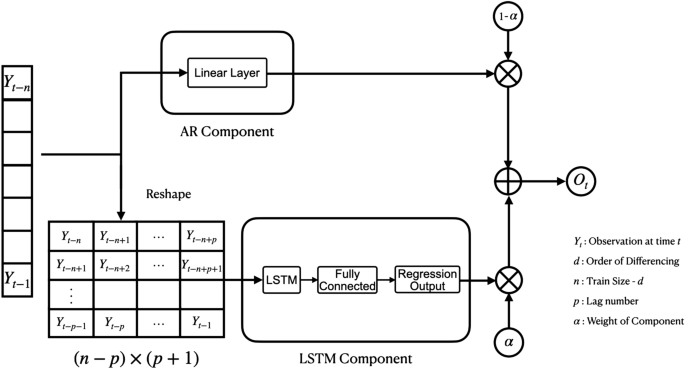
Visualization of the hybrid architecture.
The results include four sections: Model evaluations , Prediction , Interpretability , and Comparative study on the WHO datasets . In Model evaluations, we introduce the metrics we use to evaluate the models and on which we compare the models’ performances. In section Prediction , we exhibit the visualizations of several interesting trials and compare the numerical predictions and evaluations of the three models. In Interpretability , we compare the AR component of the hybrid model with the AR model. This is to examine how we may interpret the hybrid model. We leave other training details in Supplementary Material . In Comparative study on the WHO datasets , we further examine the performance of the proposed hybrid model by applying it to data of 7 different countries around the world and comparing its performance with that of its component models and 3 additional models.
Data description and statistical analysis
We utilize two primary data sources. The first data source is a dataset specific to California counties, which is available in the CHHS Open Data repository under the title COVID-19 Time-Series Metrics by County and State . This dataset includes information on populations, positive and total tests, number of deaths, and positive cases. We conducted a preliminary statistical analysis to examine correlations between these variables and the number of daily cases. The results of this analysis can be found in Supplementary Fig. 3 in Supplementary Material , and we anticipate that they will provide valuable insights for future research.
The second data source, used for comparative analysis, can be found in the WHO repository at the WHO Coronavirus (COVID-19) Dashboard . This resource presents official daily counts of COVID-19 cases, deaths, and vaccine utilization, as reported by countries, territories, and areas. In this study, we use 7 countries: Japan, Canada, Brazil, Argentina, Singapore, Italy, and the United Kingdom.
All datasets generated and analysed during the current study are also available in the author’s Github repository 24 .
Model evaluations
We use a quantitative measure to evaluate and compare the performance of models: the Mean Absolute Percentage Error (MAPE), defined as:
A model with small values of MAPE is preferred.
We examine the performance of the three models (hybrid, AR, and LSTM) on different time periods within the available range. This is essential in our research, since the performance of a model is not constant on different trends; by intuition, a model performs better on smooth curves than it does on steep curves. By repeating our evaluation process on different time periods thus different trends, we wish to understand what trends do the model give the best performance. Such understanding will help us decide to what degrees we may trust the performance of the models. We evaluate the models repeatedly to reduce the influence brought by the instability of model training. Specifically, we leave 7 days between the first date of any two consecutive training data points. Although a larger number of repetitions seems desirable, increasing the repetition number is at the cost of making neighboring training points closer to each other. However, the difference in performance between two neighboring training points, that are too close to each other, would be attributed more to the instability of model training than to the difference in trend. Such results give us little information about the model performance over trend. In the end, we let the step number be the same as our lag number. By doing so, we suppose the concept of a week is important in forecasting.
Additional evaluation metrics
In the Supplementary Material , we additionally evaluate and compare above models using Root Mean Square Error (RMSE) and Mean Absolute Error (MAE). The evaluation is done on the same dataset across different comparing methods.
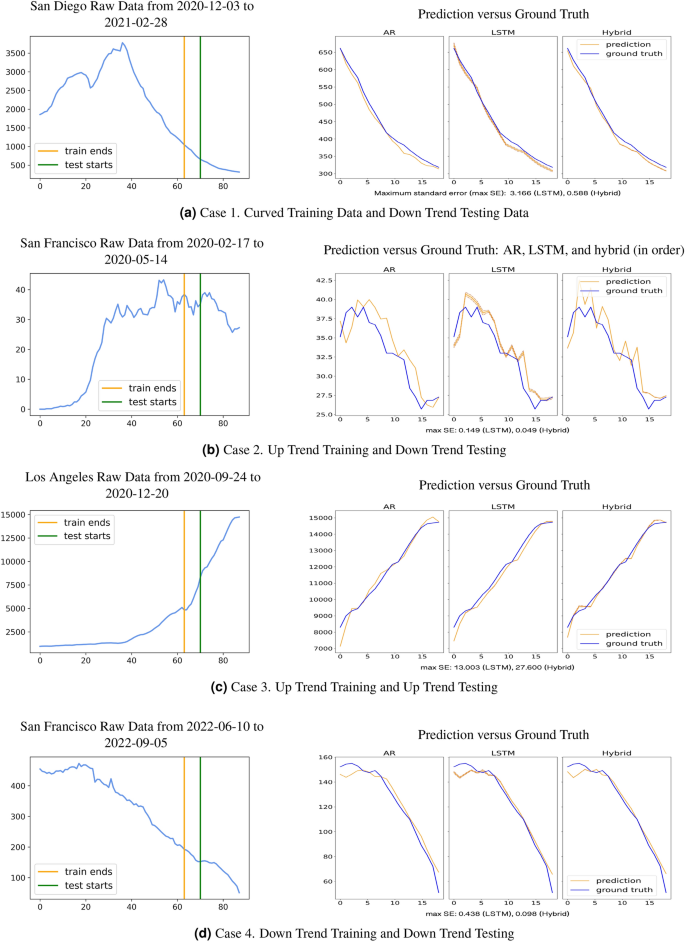
The left panels show the training and testing data. The right panels show the ground truth versus forecasts of the AR, LSTM, and hybrid model, respectively. We display the average prediction (solid line) with 2 times standard error (shaded region). The standard error across 100 runs are reported for LSTM and hybrid. The hybrid model is more stable than the LSTM.
In this section, we present the numerical results for all three models. We perform a comprehensive comparison of the performance for the three models in multiple counties, showing the advantage of the hybrid model. All predictions are transformed back to the original scale.
Visualization
We compare the three models’ performance on COVID-19 case prediction in California 8 counties. For each county, we test the models’ performance on several different situations: for example, when the training data has an up trend and the testing data has a down trend. From all trials we practiced, we choose the following trials, presented in Figs. 3 and 4 , as representatives of different combinations of training and testing data, since they reflect the general model performances well.
Figure 3 a shows models being trained on curved data and being tested on down trend data, as shown on the left and right panel, respectively. Figure 3 b shows models being trained on up trend data and being tested on down trend data. Figure 3 c shows models being trained on up trend data and being tested on up trend data. Figure 3 d shows models being trained on down trend data and being tested on down trend data. Figure 4 a,b show models being trained on down trend data and being tested on up trend data, while Fig. 4 a has gentle upward testing data and Fig. 4 b has sharp upward testing data. Figure 4 c show models being trained and tested on jagged data.
To ensure the results above are representative, we run each selected trial 100 times, visualize the mean and standard error of these trials, and present averaged MAPE. While AR outperforms LSTM on some cases, the hybrid model outperforms both in most cases, except that in Fig. 3 b and in Fig. 4 c. The MAPE, averaged on the 100 trials, shows that LSTM (4.469%) outperforms hybrid (4.993%) slightly in Fig. 3 b. However, as shown in the right panel of Fig. 3 b, the hybrid model captures the general trend of ground truth better than LSTM does. Similarly, in Fig. 4 c, AR (3.675%) outperforms hybrid (3.718%) slightly. Yet, as shown in the right panel of Fig. 4 c, the hybrid model captures the general trend of ground truth better than AR does.
Beside, interestingly enough, the hybrid model always seems to capture the ground truth’s trend. Actually, the shape of hybrid ’s forecasts resembles either that of the AR model or that of the LSTM model, or it resembles a combination of both. When AR model captures the trend better than the LSTM does, the hybrid model resembles the AR model in forecast shape: for example, in Fig. 3 b, San Francisco 2020-02-17 to 2020-05-14, and in Fig. 4 a, Santa Barbara 2022-01-17 to 2022-04-14. When LSTM model captures the trend better than the AR does, the hybrid model resembles the LSTM model in forecast shape: for example, in Fig. 3 d, San Francisco 2022-06-10 to 2022-09-05, and in Fig. 4 b, Riverside 2022-02-16 to 2022-12-20. On jagged testing data, where AR performs better on some part and LSTM better on the other, the hybrid model presents advantages of both models: for example, in Fig. 4 c, the hybrid model resembles AR on the two ends, where AR performs better, and it resembles LSTM in shape between day 5 to day 15, where LSTM seems to capture the trend better.
General performance
We evaluated the model performances numerically, in the 8 California counties across multiple trials. The results are given in Table 2 . We observe that the hybrid model outperforms the AR model and the LSTM models almost uniformly: it generally yields the smallest average MAPE. To be specific, the general MAPE of each model (AR, LSTM, LSTM with 2 layers, and hybrid), averaged on the results for all 8 counties, is 5.629%, 4.934%, 6.804%, and 4.173% in order. In general, the hybrid model has the best general performance, and it outperforms the AR model by approximately 1.5%. The LSTM model suffers from overfitting when a second LSTM layer is added. As seen in the Supplementary Material , the proposed hybrid model also yields the lowest RMSE and MAE values.
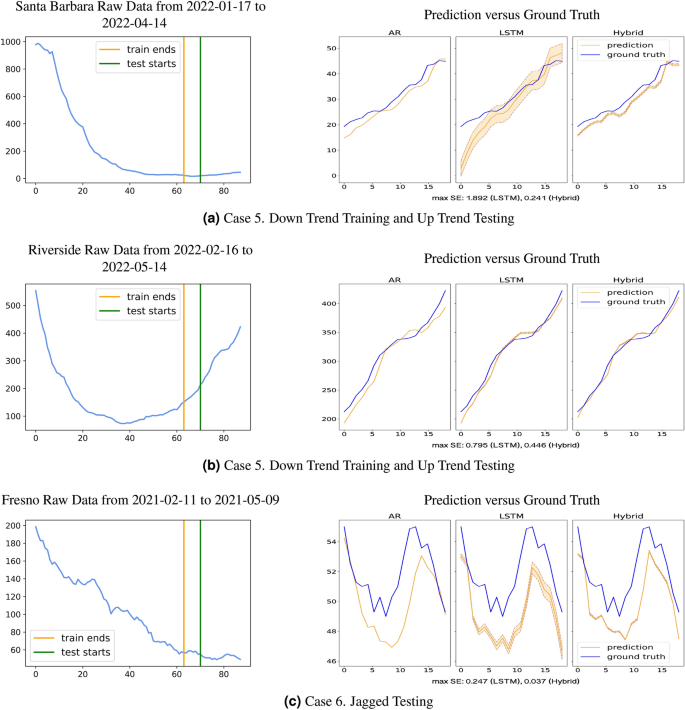
Interpretability
Interpretability of hybrid models can be defined as the ability to provide insight into the relationships they have learned, as introduced by Murdoch et al. 23 . The hybrid model proposed a decomposition approach to decipher the learned model underlying the data-generating mechanism, where the estimated AR model provides the easy-to-understand linear trend. On the other hand, the LSTM is able to capture the long-term and nonlinear trend in the time series data. Our hybrid model aims to strike a balance between interpretability and accuracy, enabling us to gain insights into the underlying data while still achieving high predictive performance.
In this section, we study how AR and LSTM components contribute to the hybrid model when fitting the data. Our purpose is to seek the insights into explaining why the hybrid model enjoys the better performance in general. And more importantly, we seek to use the interpretation from the fitted hybrid model to provide practical guidance to the public health policy making process.
Note that all models are trained on the normalized data as described in section “Training” ( Supplementary Material ). Consequently all figures below report predictions on the normalized scales.
In Fig. 5 , we present three settings with different signal strength ratio (represented by the value of \(\alpha\) ) of the AR components and LSTM components in the prediction of the hybrid model. Specifically, the larger value of \(\alpha\) indicates the AR component dominates the LSTM component in prediction, and the smaller value of \(\alpha\) indicates otherwise. We found that the component that has stronger signal characterizes the general trend in the data while the other helps to stabilize the variance. This observation sheds light into why the hybrid model provides better predictive performance in general than a single model.
Moreover, the fitted value of \(\alpha\) provides a characterization of the intrinsic nonlinearity of the data, and consequently the difficulty of exploiting interpretation in the linear components of the fitted hybrid model. The smaller the value of \(\alpha\) , the higher weight the nonlinear fit using LSTM has in the final prediction. In such a setting, coefficients in the AR components should be given less weight into generating interpretation for policy making. Equivalently, for larger value of \(\alpha\) , it is more trustworthy to derive coefficients interpretation from the important AR part. This observation is helpful for public policy maker to distinguish among different virus transmission stages.
Finally, we observe interesting patterns of the coefficients estimates in the AR components of the hybrid model compared with the coefficients in the pure AR model. As shown in Table 3 , across the three settings of different values of \(\alpha\) , the pure AR model tends to put heavier weight in coefficients of larger lags, say \(Y_{t-7}\) . In contrast, the AR component in the hybrid model tends to focus on capturing the short history, i.e., the coefficients associated with smaller lags (e.g., \(Y_{t-1}\) ) tend to have larger estimates. This indicates that the short history pattern in the data could be well approximated by a simple (say, linear) model, while the longer history in the data possesses more complicated nonlinear structure that requires a LSTM component to fit.
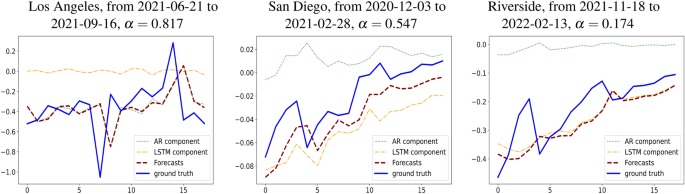
The forecasts of a hybrid model versus the ground truth, and the contribution of its AR and its LSTM component.
Comparative study on the WHO datasets
In this section, we compare our proposed hybrid model for COVID-19 prediction with its two component models, the ARIMA and LSTM models, as well as three other commonly used models: Support Vector Machines 53 (SVM), Random Forest 54 (RF), and eXtreme Gradient Boosting 55 (XGBoost). To ensure the effectiveness of our model in different application settings, we use a country-level data for this comparative study, focusing on datasets from seven different countries collected by the World Health Organization.
We provide a brief overview of the three additional comparing methods. Support Vector Machines (SVM) 42 , 47 is a machine learning model that identifies the optimal hyperplane in a high-dimensional space that maximally separates data points into different classes. An SVM applies to both classification and regression problems. SVM is know to not perform well on noisy or unbalanced data 56 , 57 .
Random Forest 43 , 44 , 45 is an ensemble learning method that constructs a multitude of decision trees. A Random Forest is very flexible and can handle complex data types. On the other hand, the Random Forests are known for their reduced interpretability, sensitivity to noise, the need for hyperparameter tuning, and potential issues with imbalanced data. These factors may impact their performance in the context of COVID-19 predictions 58 , 59 , 60 .
Extreme Gradient Boosting (XGBoost) 44 , 46 , 48 has shown exceptional performance in various tasks. XGBoost is an ensemble learning method based on gradient boosting trees. It is known for its efficiency, scalability, and accuracy. However, like other tree-based ensemble methods, it can be more challenging to interpret. This may make it difficult to understand the driving factors behind predictions. In addition, XGBoost can be prone to overfitting, especially with small datasets or when the hyperparameters are not tuned properly 61 , 62 .
We present the numerical results of the comparative study, which are visualized in Fig. 6 . The comparative study is done on data collected by the World Health Organization 63 in Japan (JPN), Canada (CAN), Brazil (BRA), Argentina (ARG), Singapore (SGP), Italy (ITA), and the United Kingdom (GBR).
Overall, the proposed hybrid model performs better than the other models in most cases, as evidenced by its lower MAPE. This suggests that our model is effective in various situations and outperforms other commonly used models for COVID-19 prediction.
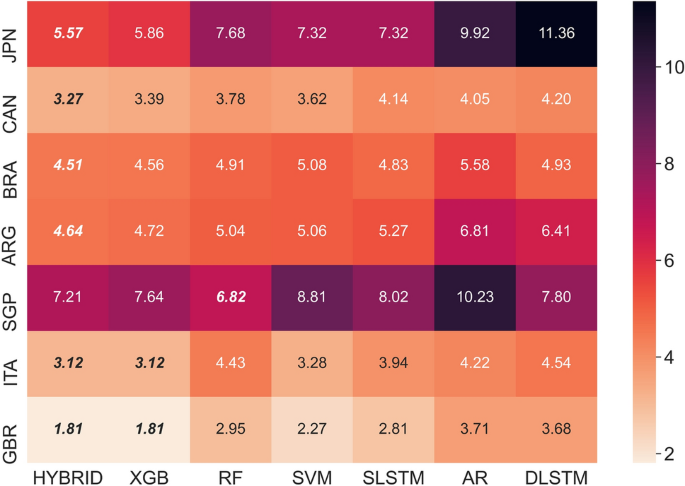
A heatmap exhibiting the performance, measured by MAPE in percentage, of the 7 models from this study and from previous work: AR, Single LSTM(LSTM), Double LSTM(DLSTM), hybrid, SVM, Random Forest(RF), XGBoost(XGB). The assessment has been done on data collected by World Health Organization, from 7 different countries around the world: Japan(JPN), Canada(CAN), Brazil(BRA), Argentina(ARG), Singapore(SGP), Italy(ITA), and The United Kingdom(GBR).
In this paper, we introduce a novel hybrid model that borrows strength from a highly structured Autoregressive model and a LSTM model for the task of COVID-19 cases prediction. Through intensive numerical experiments, we conclude that the hybrid model yields more desirable predictive performance than considering the AR or the LSTM counterpart alone. In principle, the hybrid model enjoy the advantages of each of its two building blocks: the expressive power of LSTM in representing nonlinear patterns in the data and the interpretability from the simple structures in AR. Consequently, the proposed hybrid model is useful in simultaneously providing accurate prediction and shedding light into understanding the transition of the virus transmission phases, and thus providing guidance to the public health policy making process.
It is also noteworthy that the predictive performance of the proposed hybrid model can be further improved by properly choosing the hyperparameters. Furthermore, while we considered LSTM as the nonlinear component in the hybrid model, it can be substituted by any other deep learning models.
Rahimi, I., Gandomi, A. H. & Chen, F. A review on covid-19 forecasting models. Neural Comput. Appl. https://doi.org/10.1007/s00521-020-05626-8 (2021).
Article PubMed PubMed Central Google Scholar
He, S., Peng, Y. & Sun, K. Seir modeling of the covid-19 and its dynamics. Nonlinear Dyn. 101 , 1667–1680 (2020).
Bertozzi, A. L., Franco, E., Mohler, G., Short, M. B. & Sledge, D. The challenges of modeling and forecasting the spread of covid-19. Proc. Natl. Acad. Sci. USA 117 , 16732–16738 (2020).
Article ADS MathSciNet CAS PubMed PubMed Central Google Scholar
Ndaïrou, F., Area, I., Nieto, J. J. & Torres, D. F. Mathematical modeling of covid-19 transmission dynamics with a case study of Wuhan. Chaos Solitons Fractals 135 , 109846 (2020).
Article MathSciNet PubMed PubMed Central MATH Google Scholar
O’Dea, E. B. & Drake, J. M. A semi-parametric, state-space compartmental model with time-dependent parameters for forecasting covid-19 cases, hospitalizations and deaths. J. R. Soc. Interface 19 , 20210702 (2022).
McDonald, D. J. et al. Can auxiliary indicators improve covid-19 forecasting and hotspot prediction?. Proc. Natl. Acad. Sci. USA 118 , e2111453118 (2021).
Article CAS PubMed PubMed Central Google Scholar
Maleki, M., Mahmoudi, M. R., Wraith, D. & Pho, K.-H. Time series modelling to forecast the confirmed and recovered cases of covid-19. Travel Med. Infect. Dis. 37 , 101742. https://doi.org/10.1016/j.tmaid.2020.101742 (2020).
Sioofy Khoojine, A., Shadabfar, M., Hosseini, V. R. & Kordestani, H. Network autoregressive model for the prediction of covid-19 considering the disease interaction in neighboring countries. Entropy 23 , 1267 (2021).
Article ADS CAS PubMed PubMed Central Google Scholar
Guhathakurata, S., Kundu, S., Chakraborty, A. & Banerjee, J. S. 18: A novel approach to predict covid-19 using support vector machine. In Data Science for COVID-19 (eds Kose, U. et al. ) 351–364 (Academic Press, 2021).
Yadav, M., Perumal, M. & Srinivas, M. Analysis on novel coronavirus (covid-19) using machine learning methods. Chaos Solitons Fractals 139 , 110050. https://doi.org/10.1016/j.chaos.2020.110050 (2020).
Article MathSciNet PubMed PubMed Central Google Scholar
Tiwari, D., Bhati, B. S., Al-Turjman, F. & Nagpal, B. Pandemic coronavirus disease (covid-19): World effects analysis and prediction using machine-learning techniques. Expert Syst. 39 , e12714 (2022).
Article PubMed Google Scholar
Shahid, F., Zameer, A. & Muneeb, M. Predictions for covid-19 with deep learning models of lstm, gru and bi-lstm. Chaos Solitons Fractals 140 , 110212. https://doi.org/10.1016/j.chaos.2020.110212 (2020).
Zeroual, A., Harrou, F., Dairi, A. & Sun, Y. Deep learning methods for forecasting covid-19 time-series data: A comparative study. Chaos Solitons Fractals 140 , 110121 (2020).
Davahli, M. R., Fiok, K., Karwowski, W., Aljuaid, A. M. & Taiar, R. Predicting the dynamics of the covid-19 pandemic in the United States using graph theory-based neural networks. Int. J. Environ. Res. Public Health 18 , 3834 (2021).
Alassafi, M. O., Jarrah, M. & Alotaibi, R. Time series predicting of covid-19 based on deep learning. Neurocomputing 468 , 335–344. https://doi.org/10.1016/j.neucom.2021.10.035 (2022).
Chimmula, V. K. R. & Zhang, L. Time series forecasting of covid-19 transmission in Canada using lstm networks. Chaos Solitons Fractals 135 , 109864 (2020).
Article PubMed PubMed Central MATH Google Scholar
Hawas, M. Generated time-series prediction data of covid-19’ s daily infections in Brazil by using recurrent neural networks. Data Brief 32 , 106175 (2020).
Long, J., Khaliq, A. & Furati, K. M. Identification and prediction of time-varying parameters of covid-19 model: A data-driven deep learning approach. Int. J. Comput. Math. 98 , 1617–1632 (2021).
Article MathSciNet MATH Google Scholar
Box, G. E., Jenkins, G. M., Reinsel, G. C & Ljung, G. M. Time Series Analysis: Forecasting and Control (Wiley, 2015).
Allard, R. Use of time-series analysis in infectious disease surveillance. Bull. World Health Organ. 76 (4), 327–333 (1998).
CAS PubMed PubMed Central Google Scholar
Michael A., Johansson, N. G. R., Aditi Hota, J. S. B., Santillana, M. (2016) Evaluating the performance of infectious disease forecasts: A comparison of climate-driven and seasonal dengue forecasts for Mexico. Sci. Rep. https://doi.org/10.1038/srep33707 (2016).
Sepp Hochreiter, J. S. Long short-term memory. Neural Comput. 9 , 1735–1780 (1997).
Article Google Scholar
Murdoch, W. J., Singh, C., Kumbier, K., Abbasi-Asl, R. & Yu, B. Definitions, methods, and applications in interpretable machine learning. Proc. Natl. Acad. Sci. USA 116 , 22071–22080. https://doi.org/10.1073/pnas.1900654116 (2019).
Article ADS MathSciNet CAS PubMed PubMed Central MATH Google Scholar
Zhang, Y. https://github.com/yangyi-zhang/covid-forecasting (2022).
Xuhong Li, H. X. et al. Interpretable deep learning: Interpretation, interpretability, trustworthiness, and beyond. Knowl. Inf. Syst. 64 , 3197–3234 (2022).
Vellido, A. The importance of interpretability and visualization in machine learning for applications in medicine and health care. Neural Comput. Appl. 32 , 18069–18083 (2020).
Forough Poursabzi-Sangdeh, D. G. G., Hofman, J. M., Vaughan, J. W. & Wallach, H. M. Manipulating and measuring model interpretability. CoRR abs/1802.07810 . arXiv:1802.07810 (2018).
ElAraby, M. E., Elzeki, O. M., Shams, M. Y., Mahmoud, A. & Salem, H. A novel gray-scale spatial exploitation learning net for covid-19 by crawling internet resources. Biomed. Signal Process. Control 73 , 103441 (2022).
Shams, M. Y. et al. Hana: A healthy artificial nutrition analysis model during covid-19 pandemic. Comput. Biol. Med. 135 , 104606. https://doi.org/10.1016/j.compbiomed.2021.104606 (2021).
Harleen Kaur, B. A., Ahsaan, S. U. & Chang, V. A proposed sentiment analysis deep learning algorithm for analyzing covid-19 tweets. Inf. Syst. Front. 23 , 1417–1429 (2021).
Awan, T. M. & Aslam, F. Prediction of daily covid-19 cases in European countries using automatic arima model. J. Public Health Res. 9 , 1765 (2020).
Yeşilkanat, C. M. Spatio-temporal estimation of the daily cases of covid-19 in worldwide using random forest machine learning algorithm. Chaos Solitons Fractals 140 , 110210 (2020).
Muhammad, L., Haruna, A. A., Sharif, U. S. & Mohammed, M. B. Cnn-lstm deep learning based forecasting model for covid-19 infection cases in Nigeria, South Africa and Botswana. Health Technol. 23 , 1259–1276 (2022).
Azeez, A., Obaromi, D., Odeyemi, A., Ndege, J. & Muntabayi, R. Seasonality and trend forecasting of tuberculosis prevalence data in Eastern Cape, South Africa, using a hybrid model. Int. J. Environ. Res. Public Health 13 , 757. https://doi.org/10.3390/ijerph13080757 (2016).
Yan, W., Xu, Y., Yang, X. & Zhou, Y. A hybrid model for short-term bacillary dysentery prediction in Yichang City, China. Jpn. J. Infect. Dis. 63 , 264–270. https://doi.org/10.7883/yoken.63.264 (2010).
Zhao, W., Chen, Y., Li, Y. & Guan, W. Prediction of covid-19 data using hybrid modelling approaches. Front. Public Health 10 , 923978 (2022).
Ala’raj, M., Majdalawieh, M. & Nizamuddin, N. Modeling and forecasting of covid-19 using a hybrid dynamic model based on seird with arima corrections. Infect. Dis. Model. 6 , 98–111 (2021).
PubMed Google Scholar
Zheng, N. et al. Predicting covid-19 in China using hybrid AI model. IEEE Trans. Cybern. 50 , 2891–2904 (2020).
Fan, D. et al. Well production forecasting based on arima-lstm model considering manual operations. Energy 220 , 119708 (2021).
Fathi, O. Time series forecasting using a hybrid arima and lstm model. Velvet Consult. 2019 , 1–7 (2019).
Google Scholar
Zhang, G. Time series forecasting using a hybrid arima and neural network model. Neurocomputing 50 , 159–175. https://doi.org/10.1016/S0925-2312(01)00702-0 (2003).
Article MATH Google Scholar
Atik, I. Performance comparison of regression learning methods: Covid-19 case prediction for turkey. Int. J. Mech. Eng. 7 , 6297–6308 (2022).
Galasso, J., Cao, D. M. & Hochberg, R. A random forest model for forecasting regional covid-19 cases utilizing reproduction number estimates and demographic data. Chaos Solitons Fractals 156 , 111779. https://doi.org/10.1016/j.chaos.2021.111779 (2022).
Ali, A. A., Usmani, A. & Sher, R. Covid-19 cases prediction in Saudi Arabia using tree-based ensemble models. Intell. Autom. Soft Comput. 32 , 298–400 (2022).
Chumachenko, D., Meniailov, I., Bazilevych, K., Chumachenko, T. & Yakovlev, S. Investigation of statistical machine learning models for covid-19 epidemic process simulation: Random forest, k-nearest neighbors, gradient boosting. Computation 10 , 86. https://doi.org/10.3390/computation10060086 (2022).
Article CAS Google Scholar
Fang, Z.-G., Yang, S.-Q., Lv, C.-X., An, S.-Y. & Wu, W. Application of a data-driven xgboost model for the prediction of covid-19 in the USA: A time-series study. BMJ Open 12 , e056685. https://doi.org/10.1136/bmjopen-2021-056685 (2022).
Muhammad, L. J., Alghehyne, E. A. & Usman, S. S. Supervised machine learning models for prediction of covid-19 infection using epidemiology dataset. SN Compu. Sci. https://doi.org/10.1007/s42979-020-00394-7 (2020).
Luo, J., Zhang, Z., Fu, Y. & Rao, F. Time series prediction of covid-19 transmission in America using lstm and xgboost algorithms. Results Phys. 27 , 104462. https://doi.org/10.1016/j.rinp.2021.104462 (2021).
Vadyala, S. R., Betgeri, S. N., Sherer, E. A. & Amritphale, A. Prediction of the number of covid-19 confirmed cases based on k-means-lstm. Array 11 , 100085. https://doi.org/10.1016/j.array.2021.100085 (2021).
Tomar, A. & Gupta, N. Prediction for the spread of covid-19 in India and effectiveness of preventive measures. Sci. Total Environ. 728 , 138762. https://doi.org/10.1016/j.scitotenv.2020.138762 (2020).
Bhandari, S. et al. Evolving trajectories of covid-19 curves in India: Prediction using autoregressive integrated moving average modeling. Mol. Biol. 2020 , 1–15. https://doi.org/10.21203/rs.3.rs-40385/v1 (2020).
Lipton, Z. C. A critical review of recurrent neural networks for sequence learning. CoRR. arXiv:1506.00019 (2015).
Cortes, C. & Vapnik, V. Support-vector networks. Mach. Learn. 20 , 273–297 (1995).
Breiman, L. Random forests. Mach. Learn. 45 , 5–32 (2001).
Chen, T. & Guestrin, C. Xgboost: A scalable tree boosting system. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining https://doi.org/10.1145/2939672.2939785 (ACM, 2016).
Akbani, R., Kwek, S. & Japkowicz, N. Applying support vector machines to imbalanced datasets. In Machine Learning: ECML 2004: 15th European Conference on Machine Learning. Proceedings 15 39–50 (Springer, 2004).
Fung, G. & Mangasarian, O. L. Proximal support vector machine classifiers. In Proceedings of the Seventh ACM SIGKDD International Conference on Knowledge Discovery and Data Mining 77–86 (2001).
Antoniadis, A., Lambert-Lacroix, S. & Poggi, J.-M. Random forests for global sensitivity analysis: A selective review. Reliabil. Eng. Syst. Saf. 206 , 107312 (2021).
Aria, M., Cuccurullo, C. & Gnasso, A. A comparison among interpretative proposals for random forests. Mach. Learn. Appl. 6 , 100094 (2021).
Biau, G. & Scornet, E. A random forest guided tour. Test 25 , 197–227 (2016).
Pesantez-Narvaez, J., Guillen, M. & Alcañiz, M. Predicting motor insurance claims using telematics data-xgboost versus logistic regression. Risks 7 , 70. https://doi.org/10.3390/risks7020070 (2019).
Li, W., Yin, Y., Quan, X. & Zhang, H. Gene expression value prediction based on xgboost algorithm. Front. Genet. 10 , 1077 (2019).
World Health Organization. WHO-COVID-19-Global-Data (2023).
Download references
Y. Zhang was partially supported by Raymond L Wilder Award sponsored by University of California Santa Barbara and Hellman Family Faculty Fellowship. S.T. was partially supported by Regents Junior Faculty fellowship, Faculty Early Career Acceleration grant sponsored by University of California Santa Barbara, Hellman Family Faculty Fellowship and the NSF DMS-2111303. G.Y. was partially supported by Regents Junior Faculty fellowship, Faculty Early Career Acceleration grant sponsored by University of California Santa Barbara.
Author information
Authors and affiliations.
Department of Mathematics, University of California Santa Barbara, Santa Barbara, CA, 93106, USA
Yangyi Zhang & Sui Tang
Department of Statistics and Applied Probability, University of California Santa Barbara, Santa Barbara, CA, 93106, USA
You can also search for this author in PubMed Google Scholar
Contributions
S.T. and Y.G. provided the initial idea and research plan, Y.Z. collected data, implement algorithms and performed simulations. All authors participated in the analysis and discussion of the results, and participated in the writing of the manuscript.
Corresponding authors
Correspondence to Sui Tang or Guo Yu .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhang, Y., Tang, S. & Yu, G. An interpretable hybrid predictive model of COVID-19 cases using autoregressive model and LSTM. Sci Rep 13 , 6708 (2023). https://doi.org/10.1038/s41598-023-33685-z
Download citation
Received : 11 November 2022
Accepted : 17 April 2023
Published : 25 April 2023
DOI : https://doi.org/10.1038/s41598-023-33685-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: AI and Robotics newsletter — what matters in AI and robotics research, free to your inbox weekly.
Volume 26, Number 11—November 2020
Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand
Cite This Article
We evaluated effectiveness of personal protective measures against severe acute respiratory disease coronavirus 2 (SARS-CoV-2) infection. Our case-control study included 211 cases of coronavirus disease (COVID-19) and 839 controls in Thailand. Cases were defined as asymptomatic contacts of COVID-19 patients who later tested positive for SARS-CoV-2; controls were asymptomatic contacts who never tested positive. Wearing masks all the time during contact was independently associated with lower risk for SARS-CoV-2 infection compared with not wearing masks; wearing a mask sometimes during contact did not lower infection risk. We found the type of mask worn was not independently associated with infection and that contacts who always wore masks were more likely to practice social distancing. Maintaining > 1 m distance from a person with COVID-19, having close contact for < 15 minutes, and frequent handwashing were independently associated with lower risk for infection. Our findings support consistent wearing of masks, handwashing, and social distancing to protect against COVID-19.
Evaluation of the effectiveness of mask-wearing to protect healthy persons in the general public from infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease (COVID-19), is urgently needed ( 1 , 2 ). On February 27, 2020, during the early stages of the COVID-19 outbreak, the World Health Organization (WHO) announced that wearing a mask of any type was not recommended for asymptomatic persons ( 3 ). The rationale at that time was to avoid unnecessary cost, procurement burden, and a false sense of security ( 3 ). Several systematic reviews found no conclusive evidence to support widespread use of masks in public settings to protect against respiratory infectious diseases, such as influenza and severe acute respiratory syndrome (SARS) ( 4 – 6 ). However, China, South Korea, Japan, Thailand, and other countries in Asia have recommended the use of face masks among the general public since early in the COVID-19 pandemic ( 7 ). Evidence suggests that persons with COVID-19 can have a presymptomatic period, during which they can be contagious and transmit SARS-CoV-2 to others before symptoms develop ( 8 ). These findings led to a change in recommendations from the US Centers for Disease Control and Prevention on April 4, 2020, that advised all persons wear a cloth face covering when in public ( 9 ). On April 6 and June 5, 2020, WHO updated its advice on the use of masks for the general public and encouraged countries that issue the recommendations to conduct research on this topic ( 8 ).
Thailand has been implementing multiple measures against transmission of SARS-CoV-2 since the beginning of the outbreak ( 10 , 11 ). The country established thermal screening at airports on January 3, 2020, and detected an early case of COVID-19 outside China in a traveler from Wuhan, China, arriving at Bangkok Suvarnabhumi airport on January 8, 2020 ( 10 ). Thailand uses Surveillance and Rapid Response Teams (SRRTs), together with village health volunteers, to conduct contact tracing, educate the public about COVID-19, and monitor close contacts of persons with COVID-19 in quarantine ( 11 ). SRRTs are epidemiologic teams trained to conduct surveillance, investigations, and initial control of communicable diseases, such as SARS and influenza ( 12 , 13 ). More than 1,000 district-, provincial-, and regional-level SRRTs are working on COVID-19 contact tracing in Thailand.
By February 2020, public pressure to wear masks in Thailand was high. However, medical masks became difficult for the public to procure, and the government categorized medical masks as price-controlled goods. When the Ministry of Public Health (MoPH) designated COVID-19 a dangerous communicable disease, according to the Communicable Disease Act of 2015, government officials were empowered to quarantine case-contacts and close venues ( 14 , 15 ). On March 3, MoPH recommended public use of cloth face masks ( 16 ). On March 18, schools, universities, bars, nightclubs, and entertainment venues were closed ( 17 ). On March 26, when the country was reporting »100–150 new COVID-19 cases per day, the government declared a national state of emergency, prohibited public gatherings, and enforced wearing of face masks by all persons on public transport ( 18 ). On April 21, MoPH announced 19 new PCR-confirmed COVID-19 cases, bringing the total number of cases to 2,811 ( 18 ). Given the lack of evidence, we sought to evaluate the effectiveness of mask-wearing, handwashing, social distancing, and other personal protective measures against SARS-CoV-2 infection in public in Thailand.
Study Design
We conducted a retrospective case-control study by drawing persons with COVID-19 cases and noninfected controls from a cohort of contact tracing records of the central SRRT team at the Department of Disease Control (DDC), MoPH, Thailand. We included contact investigations of 3 large COVID-19 clusters in nightclubs, boxing stadiums, and a state enterprise office in Thailand.
Contacts were defined by DDC as persons who had activities with or were in the same location as a person with confirmed COVID-19 ( 19 , 20 ). The main aim of contact tracing was to identify and evaluate contacts, perform reverse transcription PCR (RT-PCR) diagnostic tests, and quarantine high-risk contacts, as defined by the MoPH ( Appendix ). RT-PCR was performed at laboratories certified for COVID-19 testing by the National Institute of Health of Thailand ( 19 , 20 ). Data on risk factors associated with SARS-CoV-2 infection, such as type of contact and use of mask, were recorded during contact investigations, but data sometimes were incomplete.
The central SRRT performed contact investigations for clusters of > 5 PCR-confirmed COVID-19 cases from the same location within a 1-week period ( 19 , 20 ). We used these data to identify contacts who were asymptomatic during March 1–31, 2020. We used all available contact tracing records of the central SRRT in the study.
We telephoned contacts during April 30–May 27, 2020, and asked details about their contact with a COVID-19 index patient, such as dates, locations, duration, and distance of contact. We asked whether contacts wore a mask during the contact with the index patient, the type of mask, and the frequency of wearing a mask, which we defined as compliance with mask-wearing. We asked whether and how frequently contacts washed their hands while with the index patient. We asked whether contacts performed social distancing and whether they had physical contact with the COVID-19 index patient. If they did not know, or could not remember, contact with the index patient, we asked whether they had contact with other persons at the location. We asked whether the contact shared a cup or a cigarette with other persons in the place they had contact or had highest risk for contact with the index patient and whether the COVID-19 index patient, if known to the respondent, had worn a mask ( Appendix , Additional Methods). We also asked, and verified by using DDC records, whether and when the contacts had symptoms and when COVID-19 was diagnosed.
For our study, we defined cases as asymptomatic contacts who later tested positive for SARS-CoV-2, on the basis of RT-PCR results available by April 21, 2020. We defined controls as asymptomatic contacts who did not have positive test results for SARS-CoV-2 by April 21, including those who tested negative and those who were not tested. We defined asymptomatic contacts as persons who had contact with or were in the same location as a symptomatic COVID-19 patient and had no symptoms of COVID-19 on the first day of contact. We defined index patients as persons identified from contact tracing data as the potential source of SARS-CoV-2 infection; cases (as defined above) also could be index patients. We defined primary index patients as persons whose probable sources of infection were before the study period, March 1–31; for whom we were not able to identify the source of infection; or whose probable sources of infection were outside the contact tracing data included in the study. We defined high-risk exposure as that which occurred when persons lived in the same household as a COVID-19 patient; had a direct physical contact with a COVID-19 patient; were < 1 m from a COVID-19 patient for >15 minutes; or were in the same closed environment, such as a room, nightclub, stadium, or vehicle, < 1 m from a COVID-19 patient for >15 minutes.
We used 21 days after March 31 as a cutoff date based on evidence that most persons with COVID-19 likely would develop symptoms within 14 days ( 21 ) and that it could take < 7 additional days for symptomatic persons under contact investigation to go to a healthcare facility and be tested for COVID-19. Our study follows the STROBE guidelines ( 22 ).
Statistical Analysis
To include only initially asymptomatic contacts in the study, we excluded persons who reported having symptoms of COVID-19 at the time of initial contact with an index patient. Because our study focused on the risk for infection in the community, we excluded contacts whose contact locations were healthcare facilities. We also excluded primary index patients if they were the first to have symptoms at the contact investigation location, had symptoms since the first day of visiting the location, or were the origin of infection based on the contact investigation.
We estimated secondary attack rates by using the percentage of new cases among asymptomatic contacts with high-risk exposure to enable comparison with other studies. We estimated odds ratios (ORs) and 95% CIs for associations between developing COVID-19 and factors evaluated. We used logistic regression with random effects for location and for index patients nested in the same location. If an asymptomatic contact had contact with > 1 symptomatic COVID-19 index patient, the interviewer identified the index patient as the symptomatic COVID-19 patient with the closest contact. The percentage of missing values for the variable indicating whether the index patients wore a mask was 27%; thus, we did not include this variable in our analyses. For other variables, we assumed that missing values were missing at random and used imputation by chained equations ( 23 , 24 ). We created 10 imputed datasets and the imputation model included the case-control indicator and variables used in the multivariable models, including sex, age group, contact place, shortest distance of contact, duration of contact at < 1 m, sharing dishes or cups, sharing cigarettes, handwashing, mask-wearing, and compliance with mask-wearing. We developed the final multilevel mixed-effect logistic regression models on the basis of previous knowledge and a purposeful selection method ( 25 ; Appendix , Additional Analyses). Because of collinearity between mask use and mask type, we conducted a separate analysis including mask type in the multilevel mixed-effects logistic regression model for SARS-CoV-2 infection. We also tested a predefined interaction between mask type and compliance with mask-wearing ( Appendix , Additional Analyses).
To clarify patterns of behavior and factors related to compliance with mask-wearing, we used multinomial logistic regression models and the imputed dataset to estimated OR and 95% CI for associations between 3 mask-wearing compliance categories, never, sometimes, or all the time; and for other practices, including handwashing and social distancing during the contact period. We used logistic regression to estimate p values for pairwise comparisons.
To estimate the proportional reduction in cases that would occur if exposure to risk factors was reduced, we estimated the population attributable fraction by using the imputed dataset and a direct method based on logistic regression, as described previously ( 26 , 27 ; Appendix , Additional Analyses). We performed all analyses by using Stata version 14.2 (StataCorp, https://www.stata.com ) and R version 4.0.0 (R Foundation for Statistical Computing, https://www.r-project.org ).
Characteristics of the Cohort Data
Figure 1 . Flow diagram in case-control study of severe acute respiratory syndrome coronavirus 2 infections and contacts, Thailand, March–April 2020. COVID-19, coronavirus disease; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SRRT, Surveillance...
The contact tracing records of the central SRRT included 1,716 persons who had contact with or were in the same location as a person with diagnosed COVID-19 in an investigation of 3 large clusters ( Figure 1 ). Overall, 18 primary index patients were identified: 11 from the nightclub cluster, 5 from the boxing stadiums cluster, and 2 from the state enterprise office cluster. Timelines of primary index patients from the 3 clusters varied ( Appendix Figures 1–3); we excluded the 18 primary index patients from our analyses.
Characteristics of Cases and Controls
After interviewing each contact by phone and applying the exclusion criteria ( Figure 1 ), our analysis included 1,050 asymptomatic persons who had contact with or were in the same location as a symptomatic COVID-19 index patient during March 1–31, 2020. The median age of persons included was 38 years (IQR 28–51 years); 55% were male, and 45% were female ( Table 1 ). Most (61%; n = 645) asymptomatic contacts included in the study were associated with the boxing stadiums cluster, 36% (n = 374) were related to the nightclub cluster, and 3% (n = 31) were related to the state enterprise office cluster. Overall, 890 (84.8%) contacts were considered to have high-risk exposure.
Among 1,050 asymptomatic contacts included in our analysis, 211 (20.1%) tested positive for SARS-CoV-2 by April 21, 2020, and were classified as cases; 839 (79.9%) never tested positive and were controls. Of the 211 cases, 195 (92.4%) had high-risk exposures and 150 (71.1%) had symptoms before COVID-19 diagnosis by RT-PCR ( Appendix ). The last date that a COVID-19 case was detected was April 9, 2020. Among the 839 controls, 695 (82.8%) had high-risk exposures and 719 (85.7%) were tested by PCR at least once.

Figure 2 . Development and transmission of severe acute respiratory syndrome coronavirus 2 among asymptomatic contacts, Thailand, March–April 2020. Clusters indicate coronavirus disease (COVID-19) contacts from nightclubs (A); boxing stadiums (B), and the...
Among asymptomatic contacts included in the study, 228 had contact with a COVID-19 index patient at nightclubs, 144 at boxing stadiums, and 20 at the state enterprise office ( Figure 2 ). The others had contacts with a COVID-19 index patient at workplaces (n = 277), households (n = 230), and other places (n = 151). Among 890 asymptomatic contacts with high-risk exposures included in the study, the secondary attack rate from boxing stadiums was 86% (111/129), the secondary attack rate for nightclubs was 18.2% (34/187), the household secondary attack rate was 16.5% (38/230), the workplace secondary attack rate was 4.9% (10/205), and the secondary attack rate at other places was 1.4% (2/139).
Bivariate Analyses
Our analysis showed risk for SARS-CoV-2 infection was negatively associated with personal protective measures ( Table 1 ). Crude odds ratio (OR) for infection was 0.08 (95% CI 0.02–0.31) for those maintaining a distance of > 1 m from a COVID-19 patient; 0.13 (95% CI 0.04–0.46) for those whose duration of contact was ≤15 minutes; 0.41 (95% CI 0.18–0.91) for those who performed handwashing sometimes; 0.19 (95% CI 0.08–0.46) for those who washed hands often; and 0.16 (95% CI 0.07–0.36) for those wearing a mask all the time during contact with a COVID-19 patient. We noted a higher risk for SARS-CoV-2 infection among persons sharing dishes or cups (OR 2.71; 95% CI 1.48–4.94) and sharing cigarettes (OR 6.12; 95% CI 2.12–17.72) with other persons in general, not necessarily including a COVID-19 patient. In the bivariate model, type of mask was associated with risk for infection (p = 0.003).
Multivariable Analyses
We found a negative association between risk for SARS-CoV-2 infection and maintaining a distance of > 1 m from a COVID-19 patient (adjusted odds ratio [aOR] 0.15; 95% CI 0.04–0.63); duration of contact < 15 minutes (aOR 0.24; 95% CI 0.07–0.90); handwashing often (aOR 0.33; 95% CI 0.13–0.87); and wearing a mask all the time during contact with a COVID-19 patient (aOR 0.23; 95% CI 0.09–0.60) ( Table 1 ). Wearing masks sometimes during contact with a COVID-19 patient was not statistically significantly associated with lower risk for infection (aOR 0.87; 95% CI 0.41–1.84). Sharing cigarettes with other persons was associated with higher risk for infection (aOR 3.47; 95% CI 1.09–11.02).
Compliance with mask-wearing during contact with a COVID-19 patient was strongly associated with lower risk for infection in the multivariable model. Because of collinearity with mask-wearing compliance, we did not include mask type in the final model. We included mask type in a separate multivariable model and found type of mask was not independently associated with infection (p = 0.54) ( Appendix Table 1 ). We found no evidence of effect modification between mask type and mask-wearing compliance.
Association Between Mask-Wearing Compliance and Other Social Distancing Practices
Because mask-wearing throughout the contact period was negatively associated with COVID-19, we further explored characteristics of participants to ascertain whether wearing a mask produced a potential false sense of security. We found that during the contact period, 25% of persons who wore masks all the time reported maintaining > 1 m distance from contacts compared with 18% of persons who did not wear a mask (pairwise p = 0.03). In addition, persons who wore masks all the time were more likely to report duration of contact < 15 minutes (26% vs. 13% for those who did not wear a mask; pairwise p<0.001) and washing hands often (79% vs. 26% for those who did not wear a mask; pairwise p<0.001) ( Table 2 ). We found that 43% of persons who wore masks sometimes were likely to wash their hands often compared with those who did not wear masks (26%; pairwise p<0.001), but they were more likely to have physical contact (50% vs. 42%; pairwise p = 0.03) and report duration of contact >60 minutes (75% vs. 67%; pairwise p = 0.04) compared with those who did not wear masks.
Our findings provide evidence that mask-wearing, handwashing, and social distancing are independently associated with lower risk for SARS-CoV-2 infection in the general public in community settings in Thailand. We observed that wearing masks throughout the period of exposure to someone infected with SARS-CoV-2 was associated with lower risk for infection, but wearing masks only sometimes during the period was not. This evidence supports recommendations to wear masks consistently and correctly at all times in public ( 2 , 7 – 9 ).
The effectiveness of mask-wearing we observed is consistent with previous studies, including a randomized-controlled trial showing that consistent face mask use reduced risk for influenza-like illness ( 28 ), 2 case-control studies that found that mask-wearing was associated with lower risk for SARS infection ( 29 , 30 ), and a retrospective cohort study that found that mask-wearing by index patients or family members at home was associated with lower risk for SARS-CoV-2 infection ( 31 ). Previous studies found use of surgical masks or similar 12–16-layer cotton reusable masks demonstrated protection against coronavirus infection in the community ( 32 ), but we did not observe a difference between wearing nonmedical and medical masks in the general population. Our results suggest that wearing nonmedical masks in public can potentially reduce transmission of SARS-CoV-2. Another study found perception of risk of developing COVID-19 can increase a person’s likelihood of wearing a medical mask in nonmedical settings (T.D. Huynh, unpub. data, https://www.medrxiv.org/content/10.1101/2020.03.26.20044388v1 ). However, given supply shortages, medical masks should be reserved for use by healthcare workers.
We found a negative association between risk for SARS-CoV-2 infection and social distancing, consistent with previous studies that found that > 1 m physical distancing was associated with a large protective effect and distances of >2 m could be more effective ( 32 ). Our findings on effectiveness of hand hygiene also were consistent with reports in previous studies ( 33 ).
In this study, secondary attack rates at different venues varied widely. The household secondary attack rate in our study (16.5%) is comparable with ranges reported previously (11%–23%) ( 34 , 35 ), and relatively high compared with workplaces (4.9%) and other settings (1.4%). Although quarantine measures can be challenging and sometimes impractical, household members should immediately separate a person who develops symptoms of COVID-19; the sick person should stay in a specific room; use a separate bathroom, if possible; and not share dishes, cups, and other utensils ( 36 ). All household members should wear masks, frequently wash their hands, and perform social distancing to the extent possible ( 37 ).
The high number of COVID-19 cases associated with nightclub exposures in Bangkok is comparable to a COVID-19 outbreak associated with the Itaewon nightclub cluster in Seoul, South Korea, during May 2020 ( 38 ), in which persons visited several nightclubs in the same area during a short period of time. The secondary attack rate in boxing stadiums was high (86%) but similar to a cluster of COVID-19 cases associated with a football match in Italy during February 2020 ( 39 ). The secondary attack rate of COVID-19 at a choir practice in the United States was reported to be 53.3%–86.7% ( 40 ). Secondary attack rates in public gathering places with high densities of persons shouting and cheering, such as football and boxing stadiums, are still uncertain but appear to be high.
Clear and consistent public messaging from policy makers likely can prevent a false sense of security and promote compliance with social distancing in Thailand. We found that those who wore masks throughout the time they were exposed to a COVID-19 patient also were more likely to wash their hands and perform social distancing. Traditional and social media outlets can support public health responses by working with governments to provide consistent, simple, and clear messages ( 41 ). In Thailand, daily briefings from the Centre for COVID-19 Situation Administration provided clear, consistent messages on social distancing, how to put on a mask, and how to wash hands, which might have improved public confidence with the recommendations. Consistent public messages on how to wear masks correctly also are needed, particularly for those who wear masks sometimes or incorrectly, such as not covering both nose and mouth. We found that persons who only intermittently wore masks during exposure also did not practice social distancing adequately.
Our study has several limitations. First, because our findings were based on contacts related to 3 major COVID-19 clusters in Thailand during March 2020, they might not be generalizable to all settings. Second, estimated ORs were conditioned on reported contact with index patients; our study did not evaluate or consider the probability of having contact with other infected persons in the community, which could have occurred. Third, because only 89% of controls were tested, those not tested could have been infected; therefore, cases might have been missed in persons with mild or no symptoms or who did not report symptoms or seek care or testing. Nonetheless, we believe that misclassification likely was minimal because those who were not tested with RT-PCR were low-risk contacts; the small number likely would not change our main findings and recommendations on personal protective measures. Fourth, identifying every potential contact can be nearly impossible because some persons might have had contact with >1 COVID-19 patient. Hence, our estimated secondary attack rates among contacts with high-risk exposure could be overestimated or underestimated. Fifth, population attributable fraction is based on several assumptions, including causality, and should be interpreted with caution ( 42 , 43 ). Finally, findings were subject to common biases of retrospective case-control studies, including memory bias, observer bias, and information bias ( 44 ). To reduce potential biases, we used structured interviews in which each participant was asked the same set of defined questions.
As many countries begin to relax social distancing measures, our findings provide evidence supporting consistent mask-wearing, handwashing, and adhering to social distancing recommendations to reduce SARS-CoV-2 transmission in public gatherings. Wearing nonmedical masks in public could help slow the spread of COVID-19. Complying with all measures could be highly effective; however, in places with a high population density, additional measures might be required.
Clear and consistent public messaging on personal protective recommendations is essential, particularly for targeting those who wear masks intermittently or incorrectly. Our data showed that no single protective measure was associated with complete protection from COVID-19. All measures, including mask-wearing, handwashing, and social distancing, can increase protection against COVID-19 in public settings.
Dr. Pawinee Doung-ngern is the head of Communicable Disease Unit, Bureau of Epidemiology, Department of Disease Control, Ministry of Public Health, Thailand. Her primary research interests include the public health and epidemiology of communicable diseases.
Acknowledgment
This article was preprinted at https://www.medrxiv.org/content/10.1101/2020.06.11.20128900 .
- Greenhalgh T , Schmid MB , Czypionka T , Bassler D , Gruer L . Face masks for the public during the covid-19 crisis. BMJ . 2020 ; 369 : m1435 . DOI PubMed Google Scholar
- Cheng KK , Lam TH , Leung CC . Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity. Lancet . 2020 ; S0140-6736(20)30918-1 ; [ Epub ahead of print ]. PubMed Google Scholar
- World Health Organization . Rational use of personal protective equipment for coronavirus disease (COVID-19): interim guidance, 27 February 2020 [cited 2020 Jun 23]. https://apps.who.int/iris/handle/10665/331215
- Long Y , Hu T , Liu L , Chen R , Guo Q , Yang L , et al. Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis. J Evid Based Med . 2020 ; 13 : 93 – 101 . DOI PubMed Google Scholar
- Cowling BJ , Zhou Y , Ip DK , Leung GM , Aiello AE . Face masks to prevent transmission of influenza virus: a systematic review. Epidemiol Infect . 2010 ; 138 : 449 – 56 . DOI PubMed Google Scholar
- Jefferson T , Del Mar CB , Dooley L , Ferroni E , Al-Ansary LA , Bawazeer GA , et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev . 2011 ; ( 7 ): CD006207 . DOI PubMed Google Scholar
- Feng S , Shen C , Xia N , Song W , Fan M , Cowling BJ . Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med . 2020 ; 8 : 434 – 6 . DOI PubMed Google Scholar
- World Health Organization . Advice on the use of masks in the context of COVID-19: interim guidance, 5 June 2020 [cited 2020 Jun 23]. https://apps.who.int/iris/handle/10665/332293
- US Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID-19): how to protect yourself and others [cited 2020 Jun 23]. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
- Okada P , Buathong R , Phuygun S , Thanadachakul T , Parnmen S , Wongboot W , et al. Early transmission patterns of coronavirus disease 2019 (COVID-19) in travellers from Wuhan to Thailand, January 2020. Euro Surveill . 2020 ; 25 : 25 . DOI PubMed Google Scholar
- Department of Disease Control, Ministry of Public Health, Thailand . Coronavirus disease (COVID-19): situation reports 2020 [cited 2020 Jun 23]. https://ddc.moph.go.th/viralpneumonia/eng/situation.php
- Chunsuttiwat S . Response to avian influenza and preparedness for pandemic influenza: Thailand’s experience. Respirology . 2008 ; 13 ( Suppl 1 ): S36 – 40 . DOI PubMed Google Scholar
- Putthasri W , Lertiendumrong J , Chompook P , Tangcharoensathien V , Coker R . Capacity of Thailand to contain an emerging influenza pandemic. Emerg Infect Dis . 2009 ; 15 : 423 – 32 . DOI PubMed Google Scholar
- Bangkok Post. Tougher Covid-19 measures take effect Sunday. 2020 Feb 29 [cited 2020 Jun 23]. https://www.bangkokpost.com/thailand/general/1868439/tougher-covid-19-measures-take-effect-sunday
- World Health Organization . Thailand. Coronavirus disease 2019 (COVID-19) WHO Thailand situation report–11: 29 Feb 2020 [cited 2020 Jun 23]. https://www.who.int/docs/default-source/searo/thailand/20200229-tha-sitrep-11-covid-19-final.pdf
- Channel News Asia . ‘Better than nothing’: Thailand encourages cloth masks amid surgical mask shortage. 12 Mar 2020 [cited 2020 Jun 23]. https://www.channelnewsasia.com/news/asia/coronavirus-thailand-cloth-masks-surgical-shortage-covid-19-12530896
- Bangkok Post. Cabinet approves plans to close schools, postpone Songkran. 2020 Mar 17 [cited 2020 Jun 23]. https://www.bangkokpost.com/thailand/general/1880635/cabinet-approves-plans-to-close-schools-postpone-songkran
- World Health Organization . Thailand. Coronavirus disease 2019 (COVID-19) WHO Thailand situation report–59: 21 April 2020 [cited 2020 Jun 23]. https://www.who.int/docs/default-source/searo/thailand/2020-04-21-tha-sitrep-59-covid19-new-template-final.pdf
- Department of Disease Control, Ministry of Public Health, Thailand . Coronavirus disease 2019 : COVID-19, updated on 3 March 2020 [cited 2020 Jun 23]. https://ddc.moph.go.th/viralpneumonia/file/guidelines/G_Invest_03_2.pdf
- Department of Disease Control, Ministry of Public Health, Thailand . Coronavirus disease 2019 : COVID-19, updated on 23 March 2020 [cited 2020 Jun 23]. https://ddc.moph.go.th/viralpneumonia/file/g_srrt/g_srrt_250363.pdf
- Lauer SA , Grantz KH , Bi Q , Jones FK , Zheng Q , Meredith HR , et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med . 2020 ; 172 : 577 – 82 . DOI PubMed Google Scholar
- Vandenbroucke JP , von Elm E , Altman DG , Gøtzsche PC , Mulrow CD , Pocock SJ , et al. ; STROBE Initiative . STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med . 2007 ; 4 : e297 . DOI PubMed Google Scholar
- van Buuren S , Boshuizen HC , Knook DL . Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med . 1999 ; 18 : 681 – 94 . DOI PubMed Google Scholar
- Raghunathan T , Lepkowski J , Hoewyk J , Solenberger P . A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol . 2001 ; 27 : 85 – 95 .
- Bursac Z , Gauss CH , Williams DK , Hosmer DW . Purposeful selection of variables in logistic regression. Source Code Biol Med . 2008 ; 3 : 17 . DOI PubMed Google Scholar
- Azimi SS , Khalili D , Hadaegh F , Yavari P , Mehrabi Y , Azizi F . Calculating population attributable fraction for cardiovascular risk factors using different methods in a population based cohort study. J Res Health Sci . 2015 ; 15 : 22 – 7 . PubMed Google Scholar
- Rückinger S , von Kries R , Toschke AM . An illustration of and programs estimating attributable fractions in large scale surveys considering multiple risk factors. BMC Med Res Methodol . 2009 ; 9 : 7 . DOI PubMed Google Scholar
- MacIntyre CR , Cauchemez S , Dwyer DE , Seale H , Cheung P , Browne G , et al. Face mask use and control of respiratory virus transmission in households. Emerg Infect Dis . 2009 ; 15 : 233 – 41 . DOI PubMed Google Scholar
- Wu J , Xu F , Zhou W , Feikin DR , Lin CY , He X , et al. Risk factors for SARS among persons without known contact with SARS patients, Beijing, China. Emerg Infect Dis . 2004 ; 10 : 210 – 6 . DOI PubMed Google Scholar
- Lau JT , Tsui H , Lau M , Yang X . SARS transmission, risk factors, and prevention in Hong Kong. Emerg Infect Dis . 2004 ; 10 : 587 – 92 . DOI PubMed Google Scholar
- Wang Y , Tian H , Zhang L , Zhang M , Guo D , Wu W , et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Health . 2020 ; 5 : e002794 . DOI PubMed Google Scholar
- Chu DK , Akl EA , Duda S , Solo K , Yaacoub S , Schünemann HJ , et al. ; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors . Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet . 2020 ; 395 : 1973 – 87 . DOI PubMed Google Scholar
- Jefferson T , Del Mar C , Dooley L , Ferroni E , Al-Ansary LA , Bawazeer GA , et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ . 2009 ; 339 ( sep21 1 ): b3675 . DOI PubMed Google Scholar
- Bi Q , Wu Y , Mei S , Ye C , Zou X , Zhang Z , et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis . 2020 ; 20 : 911 – 9 . DOI PubMed Google Scholar
- Jing Q-L , Liu M-J , Yuan J , Zhang Z-B , Zhang A-R , Dean NE , et al. Household secondary attack rate of COVID-19 and associated determinants. Lancet Infect Dis. 2020 Jun 17 [Epub ahead of print]. PubMed Google Scholar
- US Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID-19): what to do if you are sick [cited 2020 Jun 23]. https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html
- US Centers for Disease Control and Prevention . Coronavirus disease 2019 (COVID-19): households living in close quarters [cited 2020 Jun 23]. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/living-in-close-quarters.html
- Kang CR , Lee JY , Park Y , Huh IS , Ham HJ , Han JK , et al. Seoul Metropolitan Government COVID-19; Rapid Response Team (SCoRR Team). Coronavirus disease exposure and spread from nightclubs, South Korea. Emerg Infect Dis . 2020 ; ••• : 26 .
- Boccia S , Ricciardi W , Ioannidis JPA . What other countries can learn from Italy during the COVID-19 pandemic. JAMA Intern Med . 2020 ; 180 : 927 – 8 . DOI PubMed Google Scholar
- Hamner L , Dubbel P , Capron I , Ross A , Jordan A , Lee J , et al. High SARS-CoV-2 attack rate following exposure at a choir practice—Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep . 2020 ; 69 : 606 – 10 . DOI PubMed Google Scholar
- Hopman J , Allegranzi B , Mehtar S . Managing COVID-19 in low- and middle-income countries. JAMA . 2020 ; 323 : 1549 – 50 . DOI PubMed Google Scholar
- Levine B . What does the population attributable fraction mean? Prev Chronic Dis . 2007 ; 4 : A14 . PubMed Google Scholar
- Mansournia MA , Altman DG . Population attributable fraction. BMJ . 2018 ; 360 : k757 . DOI PubMed Google Scholar
- Kopec JA , Esdaile JM . Bias in case-control studies. A review. J Epidemiol Community Health . 1990 ; 44 : 179 – 86 . DOI PubMed Google Scholar
- Figure 1 . Flow diagram in case-control study of severe acute respiratory syndrome coronavirus 2 infections and contacts, Thailand, March–April 2020. COVID-19, coronavirus disease; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SRRT,...
- Figure 2 . Development and transmission of severe acute respiratory syndrome coronavirus 2 among asymptomatic contacts, Thailand, March–April 2020. Clusters indicate coronavirus disease (COVID-19) contacts from nightclubs (A); boxing stadiums (B), and...
- Table 1 . Factors associated with coronavirus disease among persons followed through contract tracing, Thailand, March–April 2020
- Table 2 . Factors associated with compliance of mask wearing among coronavirus disease cases and controls, Thailand, March–April 2020
DOI: 10.3201/eid2611.203003
Original Publication Date: September 14, 2020
Table of Contents – Volume 26, Number 11—November 2020
| EID Search Options |
|---|
| – Search articles by author and/or keyword. |
| – Search articles by the topic country. |
| – Search articles by article type and issue. |
Please use the form below to submit correspondence to the authors or contact them at the following address:
Direk Limmathurotsakul, 420/6 Mahidol-Oxford Tropical Medicine Research Unit, Faculty of Tropical Medicine, Rajvithi Road, Bangkok 10400, Thailand
Comment submitted successfully, thank you for your feedback.
There was an unexpected error. Message not sent.
Article Citations
Highlight and copy the desired format.
| EID | Doung-ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand. Emerg Infect Dis. 2020;26(11):2607-2616. https://doi.org/10.3201/eid2611.203003 |
|---|---|
| AMA | Doung-ngern P, Suphanchaimat R, Panjangampatthana A, et al. Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand. . 2020;26(11):2607-2616. doi:10.3201/eid2611.203003. |
| APA | Doung-ngern, P., Suphanchaimat, R., Panjangampatthana, A., Janekrongtham, C., Ruampoom, D., Daochaeng, N....Limmathurotsakul, D. (2020). Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand. , (11), 2607-2616. https://doi.org/10.3201/eid2611.203003. |
Metric Details
Article views: 48530.
Data is collected weekly and does not include downloads and attachments. View data is from .
What is the Altmetric Attention Score?
The Altmetric Attention Score for a research output provides an indicator of the amount of attention that it has received. The score is derived from an automated algorithm, and represents a weighted count of the amount of attention Altmetric picked up for a research output.
- Research article
- Open access
- Published: 04 June 2021
Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews
- Israel Júnior Borges do Nascimento 1 , 2 ,
- Dónal P. O’Mathúna 3 , 4 ,
- Thilo Caspar von Groote 5 ,
- Hebatullah Mohamed Abdulazeem 6 ,
- Ishanka Weerasekara 7 , 8 ,
- Ana Marusic 9 ,
- Livia Puljak ORCID: orcid.org/0000-0002-8467-6061 10 ,
- Vinicius Tassoni Civile 11 ,
- Irena Zakarija-Grkovic 9 ,
- Tina Poklepovic Pericic 9 ,
- Alvaro Nagib Atallah 11 ,
- Santino Filoso 12 ,
- Nicola Luigi Bragazzi 13 &
- Milena Soriano Marcolino 1
On behalf of the International Network of Coronavirus Disease 2019 (InterNetCOVID-19)
BMC Infectious Diseases volume 21 , Article number: 525 ( 2021 ) Cite this article
17k Accesses
35 Citations
14 Altmetric
Metrics details
Navigating the rapidly growing body of scientific literature on the SARS-CoV-2 pandemic is challenging, and ongoing critical appraisal of this output is essential. We aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Nine databases (Medline, EMBASE, Cochrane Library, CINAHL, Web of Sciences, PDQ-Evidence, WHO’s Global Research, LILACS, and Epistemonikos) were searched from December 1, 2019, to March 24, 2020. Systematic reviews analyzing primary studies of COVID-19 were included. Two authors independently undertook screening, selection, extraction (data on clinical symptoms, prevalence, pharmacological and non-pharmacological interventions, diagnostic test assessment, laboratory, and radiological findings), and quality assessment (AMSTAR 2). A meta-analysis was performed of the prevalence of clinical outcomes.
Eighteen systematic reviews were included; one was empty (did not identify any relevant study). Using AMSTAR 2, confidence in the results of all 18 reviews was rated as “critically low”. Identified symptoms of COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%) and gastrointestinal complaints (5–9%). Severe symptoms were more common in men. Elevated C-reactive protein and lactate dehydrogenase, and slightly elevated aspartate and alanine aminotransferase, were commonly described. Thrombocytopenia and elevated levels of procalcitonin and cardiac troponin I were associated with severe disease. A frequent finding on chest imaging was uni- or bilateral multilobar ground-glass opacity. A single review investigated the impact of medication (chloroquine) but found no verifiable clinical data. All-cause mortality ranged from 0.3 to 13.9%.
Conclusions
In this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic were of questionable usefulness. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards.
Peer Review reports
The spread of the “Severe Acute Respiratory Coronavirus 2” (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [ 1 ]. The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [ 2 ], causing massive economic strain, and escalating healthcare and public health expenses [ 3 , 4 ].
The research community has responded by publishing an impressive number of scientific reports related to COVID-19. The world was alerted to the new disease at the beginning of 2020 [ 1 ], and by mid-March 2020, more than 2000 articles had been published on COVID-19 in scholarly journals, with 25% of them containing original data [ 5 ]. The living map of COVID-19 evidence, curated by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), contained more than 40,000 records by February 2021 [ 6 ]. More than 100,000 records on PubMed were labeled as “SARS-CoV-2 literature, sequence, and clinical content” by February 2021 [ 7 ].
Due to publication speed, the research community has voiced concerns regarding the quality and reproducibility of evidence produced during the COVID-19 pandemic, warning of the potential damaging approach of “publish first, retract later” [ 8 ]. It appears that these concerns are not unfounded, as it has been reported that COVID-19 articles were overrepresented in the pool of retracted articles in 2020 [ 9 ]. These concerns about inadequate evidence are of major importance because they can lead to poor clinical practice and inappropriate policies [ 10 ].
Systematic reviews are a cornerstone of today’s evidence-informed decision-making. By synthesizing all relevant evidence regarding a particular topic, systematic reviews reflect the current scientific knowledge. Systematic reviews are considered to be at the highest level in the hierarchy of evidence and should be used to make informed decisions. However, with high numbers of systematic reviews of different scope and methodological quality being published, overviews of multiple systematic reviews that assess their methodological quality are essential [ 11 , 12 , 13 ]. An overview of systematic reviews helps identify and organize the literature and highlights areas of priority in decision-making.
In this overview of systematic reviews, we aimed to summarize and critically appraise systematic reviews of coronavirus disease (COVID-19) in humans that were available at the beginning of the pandemic.
Methodology
Research question.
This overview’s primary objective was to summarize and critically appraise systematic reviews that assessed any type of primary clinical data from patients infected with SARS-CoV-2. Our research question was purposefully broad because we wanted to analyze as many systematic reviews as possible that were available early following the COVID-19 outbreak.
Study design
We conducted an overview of systematic reviews. The idea for this overview originated in a protocol for a systematic review submitted to PROSPERO (CRD42020170623), which indicated a plan to conduct an overview.
Overviews of systematic reviews use explicit and systematic methods for searching and identifying multiple systematic reviews addressing related research questions in the same field to extract and analyze evidence across important outcomes. Overviews of systematic reviews are in principle similar to systematic reviews of interventions, but the unit of analysis is a systematic review [ 14 , 15 , 16 ].
We used the overview methodology instead of other evidence synthesis methods to allow us to collate and appraise multiple systematic reviews on this topic, and to extract and analyze their results across relevant topics [ 17 ]. The overview and meta-analysis of systematic reviews allowed us to investigate the methodological quality of included studies, summarize results, and identify specific areas of available or limited evidence, thereby strengthening the current understanding of this novel disease and guiding future research [ 13 ].
A reporting guideline for overviews of reviews is currently under development, i.e., Preferred Reporting Items for Overviews of Reviews (PRIOR) [ 18 ]. As the PRIOR checklist is still not published, this study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement [ 19 ]. The methodology used in this review was adapted from the Cochrane Handbook for Systematic Reviews of Interventions and also followed established methodological considerations for analyzing existing systematic reviews [ 14 ].
Approval of a research ethics committee was not necessary as the study analyzed only publicly available articles.
Eligibility criteria
Systematic reviews were included if they analyzed primary data from patients infected with SARS-CoV-2 as confirmed by RT-PCR or another pre-specified diagnostic technique. Eligible reviews covered all topics related to COVID-19 including, but not limited to, those that reported clinical symptoms, diagnostic methods, therapeutic interventions, laboratory findings, or radiological results. Both full manuscripts and abbreviated versions, such as letters, were eligible.
No restrictions were imposed on the design of the primary studies included within the systematic reviews, the last search date, whether the review included meta-analyses or language. Reviews related to SARS-CoV-2 and other coronaviruses were eligible, but from those reviews, we analyzed only data related to SARS-CoV-2.
No consensus definition exists for a systematic review [ 20 ], and debates continue about the defining characteristics of a systematic review [ 21 ]. Cochrane’s guidance for overviews of reviews recommends setting pre-established criteria for making decisions around inclusion [ 14 ]. That is supported by a recent scoping review about guidance for overviews of systematic reviews [ 22 ].
Thus, for this study, we defined a systematic review as a research report which searched for primary research studies on a specific topic using an explicit search strategy, had a detailed description of the methods with explicit inclusion criteria provided, and provided a summary of the included studies either in narrative or quantitative format (such as a meta-analysis). Cochrane and non-Cochrane systematic reviews were considered eligible for inclusion, with or without meta-analysis, and regardless of the study design, language restriction and methodology of the included primary studies. To be eligible for inclusion, reviews had to be clearly analyzing data related to SARS-CoV-2 (associated or not with other viruses). We excluded narrative reviews without those characteristics as these are less likely to be replicable and are more prone to bias.
Scoping reviews and rapid reviews were eligible for inclusion in this overview if they met our pre-defined inclusion criteria noted above. We included reviews that addressed SARS-CoV-2 and other coronaviruses if they reported separate data regarding SARS-CoV-2.
Information sources
Nine databases were searched for eligible records published between December 1, 2019, and March 24, 2020: Cochrane Database of Systematic Reviews via Cochrane Library, PubMed, EMBASE, CINAHL (Cumulative Index to Nursing and Allied Health Literature), Web of Sciences, LILACS (Latin American and Caribbean Health Sciences Literature), PDQ-Evidence, WHO’s Global Research on Coronavirus Disease (COVID-19), and Epistemonikos.
The comprehensive search strategy for each database is provided in Additional file 1 and was designed and conducted in collaboration with an information specialist. All retrieved records were primarily processed in EndNote, where duplicates were removed, and records were then imported into the Covidence platform [ 23 ]. In addition to database searches, we screened reference lists of reviews included after screening records retrieved via databases.
Study selection
All searches, screening of titles and abstracts, and record selection, were performed independently by two investigators using the Covidence platform [ 23 ]. Articles deemed potentially eligible were retrieved for full-text screening carried out independently by two investigators. Discrepancies at all stages were resolved by consensus. During the screening, records published in languages other than English were translated by a native/fluent speaker.
Data collection process
We custom designed a data extraction table for this study, which was piloted by two authors independently. Data extraction was performed independently by two authors. Conflicts were resolved by consensus or by consulting a third researcher.
We extracted the following data: article identification data (authors’ name and journal of publication), search period, number of databases searched, population or settings considered, main results and outcomes observed, and number of participants. From Web of Science (Clarivate Analytics, Philadelphia, PA, USA), we extracted journal rank (quartile) and Journal Impact Factor (JIF).
We categorized the following as primary outcomes: all-cause mortality, need for and length of mechanical ventilation, length of hospitalization (in days), admission to intensive care unit (yes/no), and length of stay in the intensive care unit.
The following outcomes were categorized as exploratory: diagnostic methods used for detection of the virus, male to female ratio, clinical symptoms, pharmacological and non-pharmacological interventions, laboratory findings (full blood count, liver enzymes, C-reactive protein, d-dimer, albumin, lipid profile, serum electrolytes, blood vitamin levels, glucose levels, and any other important biomarkers), and radiological findings (using radiography, computed tomography, magnetic resonance imaging or ultrasound).
We also collected data on reporting guidelines and requirements for the publication of systematic reviews and meta-analyses from journal websites where included reviews were published.
Quality assessment in individual reviews
Two researchers independently assessed the reviews’ quality using the “A MeaSurement Tool to Assess Systematic Reviews 2 (AMSTAR 2)”. We acknowledge that the AMSTAR 2 was created as “a critical appraisal tool for systematic reviews that include randomized or non-randomized studies of healthcare interventions, or both” [ 24 ]. However, since AMSTAR 2 was designed for systematic reviews of intervention trials, and we included additional types of systematic reviews, we adjusted some AMSTAR 2 ratings and reported these in Additional file 2 .
Adherence to each item was rated as follows: yes, partial yes, no, or not applicable (such as when a meta-analysis was not conducted). The overall confidence in the results of the review is rated as “critically low”, “low”, “moderate” or “high”, according to the AMSTAR 2 guidance based on seven critical domains, which are items 2, 4, 7, 9, 11, 13, 15 as defined by AMSTAR 2 authors [ 24 ]. We reported our adherence ratings for transparency of our decision with accompanying explanations, for each item, in each included review.
One of the included systematic reviews was conducted by some members of this author team [ 25 ]. This review was initially assessed independently by two authors who were not co-authors of that review to prevent the risk of bias in assessing this study.
Synthesis of results
For data synthesis, we prepared a table summarizing each systematic review. Graphs illustrating the mortality rate and clinical symptoms were created. We then prepared a narrative summary of the methods, findings, study strengths, and limitations.
For analysis of the prevalence of clinical outcomes, we extracted data on the number of events and the total number of patients to perform proportional meta-analysis using RStudio© software, with the “meta” package (version 4.9–6), using the “metaprop” function for reviews that did not perform a meta-analysis, excluding case studies because of the absence of variance. For reviews that did not perform a meta-analysis, we presented pooled results of proportions with their respective confidence intervals (95%) by the inverse variance method with a random-effects model, using the DerSimonian-Laird estimator for τ 2 . We adjusted data using Freeman-Tukey double arcosen transformation. Confidence intervals were calculated using the Clopper-Pearson method for individual studies. We created forest plots using the RStudio© software, with the “metafor” package (version 2.1–0) and “forest” function.
Managing overlapping systematic reviews
Some of the included systematic reviews that address the same or similar research questions may include the same primary studies in overviews. Including such overlapping reviews may introduce bias when outcome data from the same primary study are included in the analyses of an overview multiple times. Thus, in summaries of evidence, multiple-counting of the same outcome data will give data from some primary studies too much influence [ 14 ]. In this overview, we did not exclude overlapping systematic reviews because, according to Cochrane’s guidance, it may be appropriate to include all relevant reviews’ results if the purpose of the overview is to present and describe the current body of evidence on a topic [ 14 ]. To avoid any bias in summary estimates associated with overlapping reviews, we generated forest plots showing data from individual systematic reviews, but the results were not pooled because some primary studies were included in multiple reviews.
Our search retrieved 1063 publications, of which 175 were duplicates. Most publications were excluded after the title and abstract analysis ( n = 860). Among the 28 studies selected for full-text screening, 10 were excluded for the reasons described in Additional file 3 , and 18 were included in the final analysis (Fig. 1 ) [ 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Reference list screening did not retrieve any additional systematic reviews.

PRISMA flow diagram
Characteristics of included reviews
Summary features of 18 systematic reviews are presented in Table 1 . They were published in 14 different journals. Only four of these journals had specific requirements for systematic reviews (with or without meta-analysis): European Journal of Internal Medicine, Journal of Clinical Medicine, Ultrasound in Obstetrics and Gynecology, and Clinical Research in Cardiology . Two journals reported that they published only invited reviews ( Journal of Medical Virology and Clinica Chimica Acta ). Three systematic reviews in our study were published as letters; one was labeled as a scoping review and another as a rapid review (Table 2 ).
All reviews were published in English, in first quartile (Q1) journals, with JIF ranging from 1.692 to 6.062. One review was empty, meaning that its search did not identify any relevant studies; i.e., no primary studies were included [ 36 ]. The remaining 17 reviews included 269 unique studies; the majority ( N = 211; 78%) were included in only a single review included in our study (range: 1 to 12). Primary studies included in the reviews were published between December 2019 and March 18, 2020, and comprised case reports, case series, cohorts, and other observational studies. We found only one review that included randomized clinical trials [ 38 ]. In the included reviews, systematic literature searches were performed from 2019 (entire year) up to March 9, 2020. Ten systematic reviews included meta-analyses. The list of primary studies found in the included systematic reviews is shown in Additional file 4 , as well as the number of reviews in which each primary study was included.
Population and study designs
Most of the reviews analyzed data from patients with COVID-19 who developed pneumonia, acute respiratory distress syndrome (ARDS), or any other correlated complication. One review aimed to evaluate the effectiveness of using surgical masks on preventing transmission of the virus [ 36 ], one review was focused on pediatric patients [ 34 ], and one review investigated COVID-19 in pregnant women [ 37 ]. Most reviews assessed clinical symptoms, laboratory findings, or radiological results.
Systematic review findings
The summary of findings from individual reviews is shown in Table 2 . Overall, all-cause mortality ranged from 0.3 to 13.9% (Fig. 2 ).

A meta-analysis of the prevalence of mortality
Clinical symptoms
Seven reviews described the main clinical manifestations of COVID-19 [ 26 , 28 , 29 , 34 , 35 , 39 , 41 ]. Three of them provided only a narrative discussion of symptoms [ 26 , 34 , 35 ]. In the reviews that performed a statistical analysis of the incidence of different clinical symptoms, symptoms in patients with COVID-19 were (range values of point estimates): fever (82–95%), cough with or without sputum (58–72%), dyspnea (26–59%), myalgia or muscle fatigue (29–51%), sore throat (10–13%), headache (8–12%), gastrointestinal disorders, such as diarrhea, nausea or vomiting (5.0–9.0%), and others (including, in one study only: dizziness 12.1%) (Figs. 3 , 4 , 5 , 6 , 7 , 8 and 9 ). Three reviews assessed cough with and without sputum together; only one review assessed sputum production itself (28.5%).

A meta-analysis of the prevalence of fever

A meta-analysis of the prevalence of cough

A meta-analysis of the prevalence of dyspnea

A meta-analysis of the prevalence of fatigue or myalgia

A meta-analysis of the prevalence of headache

A meta-analysis of the prevalence of gastrointestinal disorders

A meta-analysis of the prevalence of sore throat
Diagnostic aspects
Three reviews described methodologies, protocols, and tools used for establishing the diagnosis of COVID-19 [ 26 , 34 , 38 ]. The use of respiratory swabs (nasal or pharyngeal) or blood specimens to assess the presence of SARS-CoV-2 nucleic acid using RT-PCR assays was the most commonly used diagnostic method mentioned in the included studies. These diagnostic tests have been widely used, but their precise sensitivity and specificity remain unknown. One review included a Chinese study with clinical diagnosis with no confirmation of SARS-CoV-2 infection (patients were diagnosed with COVID-19 if they presented with at least two symptoms suggestive of COVID-19, together with laboratory and chest radiography abnormalities) [ 34 ].
Therapeutic possibilities
Pharmacological and non-pharmacological interventions (supportive therapies) used in treating patients with COVID-19 were reported in five reviews [ 25 , 27 , 34 , 35 , 38 ]. Antivirals used empirically for COVID-19 treatment were reported in seven reviews [ 25 , 27 , 34 , 35 , 37 , 38 , 41 ]; most commonly used were protease inhibitors (lopinavir, ritonavir, darunavir), nucleoside reverse transcriptase inhibitor (tenofovir), nucleotide analogs (remdesivir, galidesivir, ganciclovir), and neuraminidase inhibitors (oseltamivir). Umifenovir, a membrane fusion inhibitor, was investigated in two studies [ 25 , 35 ]. Possible supportive interventions analyzed were different types of oxygen supplementation and breathing support (invasive or non-invasive ventilation) [ 25 ]. The use of antibiotics, both empirically and to treat secondary pneumonia, was reported in six studies [ 25 , 26 , 27 , 34 , 35 , 38 ]. One review specifically assessed evidence on the efficacy and safety of the anti-malaria drug chloroquine [ 27 ]. It identified 23 ongoing trials investigating the potential of chloroquine as a therapeutic option for COVID-19, but no verifiable clinical outcomes data. The use of mesenchymal stem cells, antifungals, and glucocorticoids were described in four reviews [ 25 , 34 , 35 , 38 ].
Laboratory and radiological findings
Of the 18 reviews included in this overview, eight analyzed laboratory parameters in patients with COVID-19 [ 25 , 29 , 30 , 32 , 33 , 34 , 35 , 39 ]; elevated C-reactive protein levels, associated with lymphocytopenia, elevated lactate dehydrogenase, as well as slightly elevated aspartate and alanine aminotransferase (AST, ALT) were commonly described in those eight reviews. Lippi et al. assessed cardiac troponin I (cTnI) [ 25 ], procalcitonin [ 32 ], and platelet count [ 33 ] in COVID-19 patients. Elevated levels of procalcitonin [ 32 ] and cTnI [ 30 ] were more likely to be associated with a severe disease course (requiring intensive care unit admission and intubation). Furthermore, thrombocytopenia was frequently observed in patients with complicated COVID-19 infections [ 33 ].
Chest imaging (chest radiography and/or computed tomography) features were assessed in six reviews, all of which described a frequent pattern of local or bilateral multilobar ground-glass opacity [ 25 , 34 , 35 , 39 , 40 , 41 ]. Those six reviews showed that septal thickening, bronchiectasis, pleural and cardiac effusions, halo signs, and pneumothorax were observed in patients suffering from COVID-19.
Quality of evidence in individual systematic reviews
Table 3 shows the detailed results of the quality assessment of 18 systematic reviews, including the assessment of individual items and summary assessment. A detailed explanation for each decision in each review is available in Additional file 5 .
Using AMSTAR 2 criteria, confidence in the results of all 18 reviews was rated as “critically low” (Table 3 ). Common methodological drawbacks were: omission of prospective protocol submission or publication; use of inappropriate search strategy: lack of independent and dual literature screening and data-extraction (or methodology unclear); absence of an explanation for heterogeneity among the studies included; lack of reasons for study exclusion (or rationale unclear).
Risk of bias assessment, based on a reported methodological tool, and quality of evidence appraisal, in line with the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, were reported only in one review [ 25 ]. Five reviews presented a table summarizing bias, using various risk of bias tools [ 25 , 29 , 39 , 40 , 41 ]. One review analyzed “study quality” [ 37 ]. One review mentioned the risk of bias assessment in the methodology but did not provide any related analysis [ 28 ].
This overview of systematic reviews analyzed the first 18 systematic reviews published after the onset of the COVID-19 pandemic, up to March 24, 2020, with primary studies involving more than 60,000 patients. Using AMSTAR-2, we judged that our confidence in all those reviews was “critically low”. Ten reviews included meta-analyses. The reviews presented data on clinical manifestations, laboratory and radiological findings, and interventions. We found no systematic reviews on the utility of diagnostic tests.
Symptoms were reported in seven reviews; most of the patients had a fever, cough, dyspnea, myalgia or muscle fatigue, and gastrointestinal disorders such as diarrhea, nausea, or vomiting. Olfactory dysfunction (anosmia or dysosmia) has been described in patients infected with COVID-19 [ 43 ]; however, this was not reported in any of the reviews included in this overview. During the SARS outbreak in 2002, there were reports of impairment of the sense of smell associated with the disease [ 44 , 45 ].
The reported mortality rates ranged from 0.3 to 14% in the included reviews. Mortality estimates are influenced by the transmissibility rate (basic reproduction number), availability of diagnostic tools, notification policies, asymptomatic presentations of the disease, resources for disease prevention and control, and treatment facilities; variability in the mortality rate fits the pattern of emerging infectious diseases [ 46 ]. Furthermore, the reported cases did not consider asymptomatic cases, mild cases where individuals have not sought medical treatment, and the fact that many countries had limited access to diagnostic tests or have implemented testing policies later than the others. Considering the lack of reviews assessing diagnostic testing (sensitivity, specificity, and predictive values of RT-PCT or immunoglobulin tests), and the preponderance of studies that assessed only symptomatic individuals, considerable imprecision around the calculated mortality rates existed in the early stage of the COVID-19 pandemic.
Few reviews included treatment data. Those reviews described studies considered to be at a very low level of evidence: usually small, retrospective studies with very heterogeneous populations. Seven reviews analyzed laboratory parameters; those reviews could have been useful for clinicians who attend patients suspected of COVID-19 in emergency services worldwide, such as assessing which patients need to be reassessed more frequently.
All systematic reviews scored poorly on the AMSTAR 2 critical appraisal tool for systematic reviews. Most of the original studies included in the reviews were case series and case reports, impacting the quality of evidence. Such evidence has major implications for clinical practice and the use of these reviews in evidence-based practice and policy. Clinicians, patients, and policymakers can only have the highest confidence in systematic review findings if high-quality systematic review methodologies are employed. The urgent need for information during a pandemic does not justify poor quality reporting.
We acknowledge that there are numerous challenges associated with analyzing COVID-19 data during a pandemic [ 47 ]. High-quality evidence syntheses are needed for decision-making, but each type of evidence syntheses is associated with its inherent challenges.
The creation of classic systematic reviews requires considerable time and effort; with massive research output, they quickly become outdated, and preparing updated versions also requires considerable time. A recent study showed that updates of non-Cochrane systematic reviews are published a median of 5 years after the publication of the previous version [ 48 ].
Authors may register a review and then abandon it [ 49 ], but the existence of a public record that is not updated may lead other authors to believe that the review is still ongoing. A quarter of Cochrane review protocols remains unpublished as completed systematic reviews 8 years after protocol publication [ 50 ].
Rapid reviews can be used to summarize the evidence, but they involve methodological sacrifices and simplifications to produce information promptly, with inconsistent methodological approaches [ 51 ]. However, rapid reviews are justified in times of public health emergencies, and even Cochrane has resorted to publishing rapid reviews in response to the COVID-19 crisis [ 52 ]. Rapid reviews were eligible for inclusion in this overview, but only one of the 18 reviews included in this study was labeled as a rapid review.
Ideally, COVID-19 evidence would be continually summarized in a series of high-quality living systematic reviews, types of evidence synthesis defined as “ a systematic review which is continually updated, incorporating relevant new evidence as it becomes available ” [ 53 ]. However, conducting living systematic reviews requires considerable resources, calling into question the sustainability of such evidence synthesis over long periods [ 54 ].
Research reports about COVID-19 will contribute to research waste if they are poorly designed, poorly reported, or simply not necessary. In principle, systematic reviews should help reduce research waste as they usually provide recommendations for further research that is needed or may advise that sufficient evidence exists on a particular topic [ 55 ]. However, systematic reviews can also contribute to growing research waste when they are not needed, or poorly conducted and reported. Our present study clearly shows that most of the systematic reviews that were published early on in the COVID-19 pandemic could be categorized as research waste, as our confidence in their results is critically low.
Our study has some limitations. One is that for AMSTAR 2 assessment we relied on information available in publications; we did not attempt to contact study authors for clarifications or additional data. In three reviews, the methodological quality appraisal was challenging because they were published as letters, or labeled as rapid communications. As a result, various details about their review process were not included, leading to AMSTAR 2 questions being answered as “not reported”, resulting in low confidence scores. Full manuscripts might have provided additional information that could have led to higher confidence in the results. In other words, low scores could reflect incomplete reporting, not necessarily low-quality review methods. To make their review available more rapidly and more concisely, the authors may have omitted methodological details. A general issue during a crisis is that speed and completeness must be balanced. However, maintaining high standards requires proper resourcing and commitment to ensure that the users of systematic reviews can have high confidence in the results.
Furthermore, we used adjusted AMSTAR 2 scoring, as the tool was designed for critical appraisal of reviews of interventions. Some reviews may have received lower scores than actually warranted in spite of these adjustments.
Another limitation of our study may be the inclusion of multiple overlapping reviews, as some included reviews included the same primary studies. According to the Cochrane Handbook, including overlapping reviews may be appropriate when the review’s aim is “ to present and describe the current body of systematic review evidence on a topic ” [ 12 ], which was our aim. To avoid bias with summarizing evidence from overlapping reviews, we presented the forest plots without summary estimates. The forest plots serve to inform readers about the effect sizes for outcomes that were reported in each review.
Several authors from this study have contributed to one of the reviews identified [ 25 ]. To reduce the risk of any bias, two authors who did not co-author the review in question initially assessed its quality and limitations.
Finally, we note that the systematic reviews included in our overview may have had issues that our analysis did not identify because we did not analyze their primary studies to verify the accuracy of the data and information they presented. We give two examples to substantiate this possibility. Lovato et al. wrote a commentary on the review of Sun et al. [ 41 ], in which they criticized the authors’ conclusion that sore throat is rare in COVID-19 patients [ 56 ]. Lovato et al. highlighted that multiple studies included in Sun et al. did not accurately describe participants’ clinical presentations, warning that only three studies clearly reported data on sore throat [ 56 ].
In another example, Leung [ 57 ] warned about the review of Li, L.Q. et al. [ 29 ]: “ it is possible that this statistic was computed using overlapped samples, therefore some patients were double counted ”. Li et al. responded to Leung that it is uncertain whether the data overlapped, as they used data from published articles and did not have access to the original data; they also reported that they requested original data and that they plan to re-do their analyses once they receive them; they also urged readers to treat the data with caution [ 58 ]. This points to the evolving nature of evidence during a crisis.
Our study’s strength is that this overview adds to the current knowledge by providing a comprehensive summary of all the evidence synthesis about COVID-19 available early after the onset of the pandemic. This overview followed strict methodological criteria, including a comprehensive and sensitive search strategy and a standard tool for methodological appraisal of systematic reviews.
In conclusion, in this overview of systematic reviews, we analyzed evidence from the first 18 systematic reviews that were published after the emergence of COVID-19. However, confidence in the results of all the reviews was “critically low”. Thus, systematic reviews that were published early on in the pandemic could be categorized as research waste. Even during public health emergencies, studies and systematic reviews should adhere to established methodological standards to provide patients, clinicians, and decision-makers trustworthy evidence.
Availability of data and materials
All data collected and analyzed within this study are available from the corresponding author on reasonable request.
World Health Organization. Timeline - COVID-19: Available at: https://www.who.int/news/item/29-06-2020-covidtimeline . Accessed 1 June 2021.
COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html . Accessed 1 June 2021.
Anzai A, Kobayashi T, Linton NM, Kinoshita R, Hayashi K, Suzuki A, et al. Assessing the Impact of Reduced Travel on Exportation Dynamics of Novel Coronavirus Infection (COVID-19). J Clin Med. 2020;9(2):601.
Chinazzi M, Davis JT, Ajelli M, Gioannini C, Litvinova M, Merler S, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. https://doi.org/10.1126/science.aba9757 .
Article CAS PubMed PubMed Central Google Scholar
Fidahic M, Nujic D, Runjic R, Civljak M, Markotic F, Lovric Makaric Z, et al. Research methodology and characteristics of journal articles with original data, preprint articles and registered clinical trial protocols about COVID-19. BMC Med Res Methodol. 2020;20(1):161. https://doi.org/10.1186/s12874-020-01047-2 .
EPPI Centre . COVID-19: a living systematic map of the evidence. Available at: http://eppi.ioe.ac.uk/cms/Projects/DepartmentofHealthandSocialCare/Publishedreviews/COVID-19Livingsystematicmapoftheevidence/tabid/3765/Default.aspx . Accessed 1 June 2021.
NCBI SARS-CoV-2 Resources. Available at: https://www.ncbi.nlm.nih.gov/sars-cov-2/ . Accessed 1 June 2021.
Gustot T. Quality and reproducibility during the COVID-19 pandemic. JHEP Rep. 2020;2(4):100141. https://doi.org/10.1016/j.jhepr.2020.100141 .
Article PubMed PubMed Central Google Scholar
Kodvanj, I., et al., Publishing of COVID-19 Preprints in Peer-reviewed Journals, Preprinting Trends, Public Discussion and Quality Issues. Preprint article. bioRxiv 2020.11.23.394577; doi: https://doi.org/10.1101/2020.11.23.394577 .
Dobler CC. Poor quality research and clinical practice during COVID-19. Breathe (Sheff). 2020;16(2):200112. https://doi.org/10.1183/20734735.0112-2020 .
Article Google Scholar
Bastian H, Glasziou P, Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLoS Med. 2010;7(9):e1000326. https://doi.org/10.1371/journal.pmed.1000326 .
Lunny C, Brennan SE, McDonald S, McKenzie JE. Toward a comprehensive evidence map of overview of systematic review methods: paper 1-purpose, eligibility, search and data extraction. Syst Rev. 2017;6(1):231. https://doi.org/10.1186/s13643-017-0617-1 .
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane. 2020. Available from www.training.cochrane.org/handbook .
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.1 (updated September 2020). Cochrane. 2020; Available from www.training.cochrane.org/handbook .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):18. https://doi.org/10.1186/s13643-018-0914-3 .
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):29. https://doi.org/10.1186/s13643-018-0768-8 .
Hunt H, Pollock A, Campbell P, Estcourt L, Brunton G. An introduction to overviews of reviews: planning a relevant research question and objective for an overview. Syst Rev. 2018;7(1):39. https://doi.org/10.1186/s13643-018-0695-8 .
Pollock M, Fernandes RM, Pieper D, Tricco AC, Gates M, Gates A, et al. Preferred reporting items for overviews of reviews (PRIOR): a protocol for development of a reporting guideline for overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):335. https://doi.org/10.1186/s13643-019-1252-9 .
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Open Med. 2009;3(3):e123–30.
Krnic Martinic M, Pieper D, Glatt A, Puljak L. Definition of a systematic review used in overviews of systematic reviews, meta-epidemiological studies and textbooks. BMC Med Res Methodol. 2019;19(1):203. https://doi.org/10.1186/s12874-019-0855-0 .
Puljak L. If there is only one author or only one database was searched, a study should not be called a systematic review. J Clin Epidemiol. 2017;91:4–5. https://doi.org/10.1016/j.jclinepi.2017.08.002 .
Article PubMed Google Scholar
Gates M, Gates A, Guitard S, Pollock M, Hartling L. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev. 2020;9(1):254. https://doi.org/10.1186/s13643-020-01509-0 .
Covidence - systematic review software. Available at: https://www.covidence.org/ . Accessed 1 June 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Borges do Nascimento IJ, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med. 2020;9(4):941.
Article PubMed Central Google Scholar
Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. https://doi.org/10.1186/s40249-020-00646-x .
Cortegiani A, Ingoglia G, Ippolito M, Giarratano A, Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–83. https://doi.org/10.1016/j.jcrc.2020.03.005 .
Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531–8. https://doi.org/10.1007/s00392-020-01626-9 .
Article CAS PubMed Google Scholar
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577–83. https://doi.org/10.1002/jmv.25757 .
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001 .
Lippi G, Henry BM. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med. 2020;75:107–8. https://doi.org/10.1016/j.ejim.2020.03.014 .
Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chim Acta. 2020;505:190–1. https://doi.org/10.1016/j.cca.2020.03.004 .
Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta. 2020;506:145–8. https://doi.org/10.1016/j.cca.2020.03.022 .
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95. https://doi.org/10.1111/apa.15270 .
Lupia T, Scabini S, Mornese Pinna S, di Perri G, de Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: a new challenge. J Glob Antimicrob Resist. 2020;21:22–7. https://doi.org/10.1016/j.jgar.2020.02.021 .
Marasinghe, K.M., A systematic review investigating the effectiveness of face mask use in limiting the spread of COVID-19 among medically not diagnosed individuals: shedding light on current recommendations provided to individuals not medically diagnosed with COVID-19. Research Square. Preprint article. doi : https://doi.org/10.21203/rs.3.rs-16701/v1 . 2020 .
Mullins E, Evans D, Viner RM, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review. Ultrasound Obstet Gynecol. 2020;55(5):586–92. https://doi.org/10.1002/uog.22014 .
Pang J, Wang MX, Ang IYH, Tan SHX, Lewis RF, Chen JIP, et al. Potential Rapid Diagnostics, Vaccine and Therapeutics for 2019 Novel coronavirus (2019-nCoV): a systematic review. J Clin Med. 2020;9(3):623.
Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 .
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;215(1):87–93. https://doi.org/10.2214/AJR.20.23034 .
Sun P, Qie S, Liu Z, Ren J, Li K, Xi J. Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis. J Med Virol. 2020;92(6):612–7. https://doi.org/10.1002/jmv.25735 .
Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. https://doi.org/10.1016/j.ijid.2020.03.017 .
Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Investig. 2020;50(3):e13209. https://doi.org/10.1111/eci.13209 .
Article CAS Google Scholar
Hwang CS. Olfactory neuropathy in severe acute respiratory syndrome: report of a case. Acta Neurol Taiwanica. 2006;15(1):26–8.
Google Scholar
Suzuki M, Saito K, Min WP, Vladau C, Toida K, Itoh H, et al. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117(2):272–7. https://doi.org/10.1097/01.mlg.0000249922.37381.1e .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7. https://doi.org/10.1016/S1473-3099(20)30244-9 .
Wolkewitz M, Puljak L. Methodological challenges of analysing COVID-19 data during the pandemic. BMC Med Res Methodol. 2020;20(1):81. https://doi.org/10.1186/s12874-020-00972-6 .
Rombey T, Lochner V, Puljak L, Könsgen N, Mathes T, Pieper D. Epidemiology and reporting characteristics of non-Cochrane updates of systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(3):471–83. https://doi.org/10.1002/jrsm.1409 .
Runjic E, Rombey T, Pieper D, Puljak L. Half of systematic reviews about pain registered in PROSPERO were not published and the majority had inaccurate status. J Clin Epidemiol. 2019;116:114–21. https://doi.org/10.1016/j.jclinepi.2019.08.010 .
Runjic E, Behmen D, Pieper D, Mathes T, Tricco AC, Moher D, et al. Following Cochrane review protocols to completion 10 years later: a retrospective cohort study and author survey. J Clin Epidemiol. 2019;111:41–8. https://doi.org/10.1016/j.jclinepi.2019.03.006 .
Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. 2015;13(1):224. https://doi.org/10.1186/s12916-015-0465-6 .
COVID-19 Rapid Reviews: Cochrane’s response so far. Available at: https://training.cochrane.org/resource/covid-19-rapid-reviews-cochrane-response-so-far . Accessed 1 June 2021.
Cochrane. Living systematic reviews. Available at: https://community.cochrane.org/review-production/production-resources/living-systematic-reviews . Accessed 1 June 2021.
Millard T, Synnot A, Elliott J, Green S, McDonald S, Turner T. Feasibility and acceptability of living systematic reviews: results from a mixed-methods evaluation. Syst Rev. 2019;8(1):325. https://doi.org/10.1186/s13643-019-1248-5 .
Babic A, Poklepovic Pericic T, Pieper D, Puljak L. How to decide whether a systematic review is stable and not in need of updating: analysis of Cochrane reviews. Res Synth Methods. 2020;11(6):884–90. https://doi.org/10.1002/jrsm.1451 .
Lovato A, Rossettini G, de Filippis C. Sore throat in COVID-19: comment on “clinical characteristics of hospitalized patients with SARS-CoV-2 infection: a single arm meta-analysis”. J Med Virol. 2020;92(7):714–5. https://doi.org/10.1002/jmv.25815 .
Leung C. Comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1431–2. https://doi.org/10.1002/jmv.25912 .
Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. Response to Char’s comment: comment on Li et al: COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(9):1433. https://doi.org/10.1002/jmv.25924 .
Download references
Acknowledgments
We thank Catherine Henderson DPhil from Swanscoe Communications for pro bono medical writing and editing support. We acknowledge support from the Covidence Team, specifically Anneliese Arno. We thank the whole International Network of Coronavirus Disease 2019 (InterNetCOVID-19) for their commitment and involvement. Members of the InterNetCOVID-19 are listed in Additional file 6 . We thank Pavel Cerny and Roger Crosthwaite for guiding the team supervisor (IJBN) on human resources management.
This research received no external funding.
Author information
Authors and affiliations.
University Hospital and School of Medicine, Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil
Israel Júnior Borges do Nascimento & Milena Soriano Marcolino
Medical College of Wisconsin, Milwaukee, WI, USA
Israel Júnior Borges do Nascimento
Helene Fuld Health Trust National Institute for Evidence-based Practice in Nursing and Healthcare, College of Nursing, The Ohio State University, Columbus, OH, USA
Dónal P. O’Mathúna
School of Nursing, Psychotherapy and Community Health, Dublin City University, Dublin, Ireland
Department of Anesthesiology, Intensive Care and Pain Medicine, University of Münster, Münster, Germany
Thilo Caspar von Groote
Department of Sport and Health Science, Technische Universität München, Munich, Germany
Hebatullah Mohamed Abdulazeem
School of Health Sciences, Faculty of Health and Medicine, The University of Newcastle, Callaghan, Australia
Ishanka Weerasekara
Department of Physiotherapy, Faculty of Allied Health Sciences, University of Peradeniya, Peradeniya, Sri Lanka
Cochrane Croatia, University of Split, School of Medicine, Split, Croatia
Ana Marusic, Irena Zakarija-Grkovic & Tina Poklepovic Pericic
Center for Evidence-Based Medicine and Health Care, Catholic University of Croatia, Ilica 242, 10000, Zagreb, Croatia
Livia Puljak
Cochrane Brazil, Evidence-Based Health Program, Universidade Federal de São Paulo, São Paulo, Brazil
Vinicius Tassoni Civile & Alvaro Nagib Atallah
Yorkville University, Fredericton, New Brunswick, Canada
Santino Filoso
Laboratory for Industrial and Applied Mathematics (LIAM), Department of Mathematics and Statistics, York University, Toronto, Ontario, Canada
Nicola Luigi Bragazzi
You can also search for this author in PubMed Google Scholar
Contributions
IJBN conceived the research idea and worked as a project coordinator. DPOM, TCVG, HMA, IW, AM, LP, VTC, IZG, TPP, ANA, SF, NLB and MSM were involved in data curation, formal analysis, investigation, methodology, and initial draft writing. All authors revised the manuscript critically for the content. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Livia Puljak .
Ethics declarations
Ethics approval and consent to participate.
Not required as data was based on published studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1..
Search strategies used in the study.
Additional file 2: Appendix 2.
Adjusted scoring of AMSTAR 2 used in this study for systematic reviews of studies that did not analyze interventions.
Additional file 3: Appendix 3.
List of excluded studies, with reasons.
Additional file 4: Appendix 4.
Table of overlapping studies, containing the list of primary studies included, their visual overlap in individual systematic reviews, and the number in how many reviews each primary study was included.
Additional file 5: Appendix 5.
A detailed explanation of AMSTAR scoring for each item in each review.
Additional file 6: Appendix 6.
List of members and affiliates of International Network of Coronavirus Disease 2019 (InterNetCOVID-19).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Borges do Nascimento, I.J., O’Mathúna, D.P., von Groote, T.C. et al. Coronavirus disease (COVID-19) pandemic: an overview of systematic reviews. BMC Infect Dis 21 , 525 (2021). https://doi.org/10.1186/s12879-021-06214-4
Download citation
Received : 12 April 2020
Accepted : 19 May 2021
Published : 04 June 2021
DOI : https://doi.org/10.1186/s12879-021-06214-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronavirus
- Evidence-based medicine
- Infectious diseases
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Features, evaluation, and treatment of coronavirus (covid-19).
Marco Cascella ; Michael Rajnik ; Abdul Aleem ; Scott C. Dulebohn ; Raffaela Di Napoli .
Affiliations
Last Update: August 18, 2023 .
- Continuing Education Activity
Coronavirus disease 2019 (COVID-19) is a highly contagious infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 has had a catastrophic effect on the world, resulting in more than 6 million deaths worldwide. It has emerged as the most consequential global health crisis since the era of the influenza pandemic of 1918. As the virus mutates, treatment guidelines are altered to reflect the most efficacious therapies. This activity is a comprehensive review of the disease presentation, complications, and current guideline-recommended treatment options for managing this disease.
- Screen individuals based on exposure and symptom criteria to identify potential COVID-19 cases.
- Identify the clinical features and radiological findings expected in patients with COVID-19.
- Apply the recommended treatment options for patients with COVID-19.
- Create strategies with the interprofessional team for improving care coordination to care for patients with COVID-19 to help improve clinical outcomes.
- Introduction
Coronavirus disease 2019 (COVID-19) is a highly contagious viral illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 has had a catastrophic effect on the world, resulting in more than 6 million deaths worldwide. After the first cases of this predominantly respiratory viral illness were reported in Wuhan, Hubei Province, China, in late December 2019, SARS-CoV-2 rapidly disseminated worldwide. This compelled the World Health Organization (WHO) to declare it a global pandemic on March 11, 2020. [1]
Even though substantial progress in clinical research has led to a better understanding of SARS-CoV-2, many countries continue to have outbreaks of this viral illness. These outbreaks are primarily attributed to the emergence of mutant variants of the virus. Like other RNA viruses, SARS-CoV-2 adapts with genetic evolution and developing mutations. This results in mutant variants that may have different characteristics than their ancestral strains. Several variants of SARS-CoV-2 have been described during the course of this pandemic, among which only a few are considered variants of concern (VOCs). Based on the epidemiological update by the WHO, 5 SARS-CoV-2 VOCs have been identified since the beginning of the pandemic:
- Alpha (B.1.1.7): First variant of concern, which was described in the United Kingdom (UK) in late December 2020 [2]
- Beta (B.1.351) : First reported in South Africa in December 2020 [2]
- Gamma (P.1) : First reported in Brazil in early January 2021 [2]
- Delta (B.1.617.2): First reported in India in December 2020 [2]
- Omicron (B.1.1.529): First reported in South Africa in November 2021 [3]
Despite the unprecedented speed of vaccine development against the prevention of COVID-19 and robust global mass vaccination efforts, the emergence of new SARS-CoV-2 variants threatens to overturn the progress made in limiting the spread of this disease. This review aims to comprehensively describe the etiology, epidemiology, pathophysiology, and clinical features of COVID-19. This review also provides an overview of the different variants of SARS-CoV-2 and the guideline-recommended treatment (as of January 2023) for managing this disease.
Coronaviruses (CoVs) are positive-sense single-stranded RNA (+ssRNA) viruses with a crown-like appearance under an electron microscope ( coronam is the Latin term for crown) due to the presence of spike glycoproteins on the envelope. [1] The subfamily Orthocoronavirinae of the Coronaviridae family (order Nidovirales ) classifies into 4 genera of CoVs:
- Alphacoronavirus (alphaCoV)
- Betacoronavirus (betaCoV)
- Deltacoronavirus (deltaCoV)
- Gammacoronavirus (gammaCoV)
BetaCoV genus is further divided into 5 sub-genera or lineages. [4] Genomic characterization has shown that bats and rodents are the probable gene sources of alphaCoVs and betaCoVs. Avian species seem to be the source of deltaCoVs and gammaCoVs. CoVs have become significant pathogens of emerging respiratory disease outbreaks. Members of this large family of viruses can cause respiratory, enteric, hepatic, and neurological diseases in different animal species, including camels, cattle, cats, and bats.
These viruses can cross species barriers and infect humans as well. Seven human CoVs (HCoVs) capable of infecting humans have been identified. Some HCoVs were identified in the mid-1960s, while others were only detected in the new millennium. In general, estimates suggest that 2% of the population are healthy carriers of CoVs and that these viruses are responsible for about 5% to 10% of acute respiratory infections. [5]
- Common human CoVs : HCoV-OC43 and HCoV-HKU1 (betaCoVs of the A lineage), HCoV-229E, and HCoV-NL63 (alphaCoVs). These viruses can cause common colds and self-limiting upper respiratory tract infections in immunocompetent individuals. However, in immunocompromised and older patients, lower respiratory tract infections can occur due to these viruses.
- Other human CoVs : SARS-CoV and MERS-CoV (betaCoVs of the B and C lineage, respectively). These viruses are considered more virulent and capable of causing epidemics with respiratory and extra-respiratory manifestations of variable clinical severity. [1]
SARS-CoV-2 is a novel betaCoV belonging to the same subgenus as the severe acute respiratory syndrome coronavirus (SARS-CoV) and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV), which have been previously implicated in SARS-CoV and MERS-CoV epidemics with mortality rates up to 10% and 35%, respectively. [6] It has a round or elliptic and often pleomorphic form and a diameter of approximately 60 to 140 nm. Like other CoVs, it is sensitive to ultraviolet rays and heat. [6]
The inactivation temperature of SARS-CoV-2 is being researched. A stainless steel surface held at an air temperature of 54.5°C (130 °F) results in the inactivation of 90% of SARS-CoV-2 in approximately 36 minutes. [7] It resists lower temperatures, even those below 0°C. However, lipid solvents can effectively inactivate these viruses, including ether (75%), ethanol, chlorine-containing disinfectant, peroxyacetic acid, and chloroform (except for chlorhexidine).
Although the origin of SARS-CoV-2 is currently unknown, it is widely postulated to have a zoonotic transmission. [1] Genomic analyses suggest that SARS-CoV-2 probably evolved from a strain found in bats. The genomic comparison between the human SARS-CoV-2 sequence and known animal coronaviruses revealed high homology (96%) between the SARS-CoV-2 and the betaCoV RaTG13 of bats ( Rhinolophus affinis ). [8] Similar to SARS and MERS, it has been hypothesized that SARS-CoV-2 advanced from bats to intermediate hosts, such as pangolins and minks, and then to humans. [9] [10]
SARS-CoV-2 Variants
A globally dominant D614G variant was eventually identified and associated with increased transmissibility but without the ability to cause severe illness. [11] Another variant was attributed to transmission from infected farmed mink in Denmark but was not associated with increased transmissibility. [10] Since then, multiple variants of SARS-CoV-2 have been described, of which a few are considered variants of concern (VOCs) due to their potential to cause enhanced transmissibility or virulence. The United States Centers for Disease Control and Prevention (CDC) and the WHO have independently established a classification system for distinguishing the emerging variants of SARS-CoV-2 into variants of concern(VOCs) and variants of interest(VOIs).
SARS-CoV-2 Variants of Concern (VOCs)
- Alpha (B.1.1.7 lineage)
- In late December 2020, the Alpha variant, or GRY (formerly GR/501Y.V1), was reported in the UK based on whole-genome sequencing of samples from patients who tested positive for SARS-CoV-2. [12] [13]
- The variant was also identified using a commercial assay characterized by the absence of the S gene (S-gene target failure, SGTF) in PCR samples. The B.1.1.7 variant includes 17 mutations in the viral genome. Of these, 8 mutations (Δ69-70 deletion, Δ144 deletion, N501Y, A570D, P681H, T716I, S982A, D1118H) are in the spike (S) protein. N501Y shows an increased affinity of the spike protein to ACE 2 receptors, enhancing the viral attachment and subsequent entry into host cells. [14] [15] [16]
- This alpha variant was reportedly 43% to 82% more transmissible, surpassing preexisting variants of SARS-CoV-2 to emerge as the dominant SARS-CoV-2 variant in the UK. [15]
- An initial matched case-control study reported no significant difference in the risk of hospitalization or associated mortality with the B.1.1.7 lineage variant compared to other existing variants. However, subsequent studies have reported that people infected with B.1.1.7 lineage variant had increased disease severity compared to those infected with other circulating variants. [17] [13]
- A large matched cohort study in the UK reported that the mortality hazard ratio of patients infected with the B.1.1.7 lineage variant was 1.64 (95% confidence interval 1.32 to 2.04, P<0.0001) compared to patients with previously circulating strains. [18]
- Another study reported that the B 1.1.7 variant was associated with increased mortality compared to other SARS-CoV-2 variants (HR= 1.61, 95% CI 1.42-1.82). [19] The risk of death was reportedly greater (adjusted hazard ratio 1.67, 95% CI 1.34-2.09) among individuals with confirmed B.1.1.7 infection compared to individuals with non-B.1.1.7 SARS-CoV-2. [20]
- Beta (B.1.351 lineage)
- The Beta variant, or GH501Y.V2 with multiple spike mutations, resulted in the second wave of COVID-19 infections and was first detected in South Africa in October 2020. [21]
- The B.1.351 variant includes 9 mutations (L18F, D80A, D215G, R246I, K417N, E484K, N501Y, D614G, and A701V) in the spike protein, of which 3 mutations (K417N, E484K, and N501Y) are located in the receptor binding domain (RBD) and increase its binding affinity for the ACE receptors. [22] [14] [23]
- SARS-CoV-2 501Y.V2 (B.1.351 lineage) was reported in the US at the end of January 2021.
- This variant had an increased risk of transmission and reduced neutralization by monoclonal antibody therapy, convalescent sera, and post-vaccination sera. [24]
- Gamma (P.1 lineage)
- The Gamma variant, or GR/501Y.V3 , was identified in December 2020 in Brazil and was first detected in the US in January 2021. [25]
- This B.1.1.28 variant harbors ten mutations in the spike protein (L18F, T20N, P26S, D138Y, R190S, H655Y, T1027I V1176, K417T, E484K, and N501Y). Three mutations (L18F, K417N, E484K) are located in the RBD, similar to the B.1.351 variant. [25]
- The Delta variant was initially identified in December 2020 in India and was responsible for the deadly second wave of COVID-19 infections in April 2021 in India. In the United States, this variant was first detected in March 2021. [2]
- The B.1.617.2 variant harbors ten mutations ( T19R, (G142D*), 156del, 157del, R158G, L452R, T478K, D614G, P681R, D950N) in the spike protein.
- The Omicron variant was first identified in South Africa on 23 November 2021 after an uptick in the number of cases of COVID-19. [26]
- Omicron was quickly recognized as a VOC due to more than 30 changes to the spike protein of the virus and the sharp rise in the number of cases observed in South Africa. [27] The reported mutations include T91 in the envelope, P13L, E31del, R32del, S33del, R203K, G204R in the nucleocapsid protein, D3G, Q19E, A63T in the matrix, N211del/L212I, Y145del, Y144del, Y143del, G142D, T95I, V70del, H69del, A67V in the N-terminal domain of the spike, Y505H, N501Y, Q498R, G496S, Q493R, E484A, T478K, S477N, G446S, N440K, K417N, S375F, S373P, S371L, G339D in the receptor-binding domain of the spike, D796Y in the fusion peptide of the spike, L981F, N969K, Q954H in the heptad repeat 1 of the spike as well as multiple other mutations in the non-structural proteins and spike protein. [28]
- Many subvariants of Omicron, such as BA.1, BA.2, BA.3, BA.4, and BA.5, have been identified. [3]
Transmission of SARS-CoV-2
- The primary mode of transmission of SARS-CoV-2 is via exposure to respiratory droplets carrying the infectious virus from close contact or direct transmission from presymptomatic, asymptomatic, or symptomatic individuals harboring the virus. [1]
- Airborne transmission with aerosol-generating procedures has also been implicated in the spread of COVID-19. Data implicating airborne transmission of SARS-CoV-2 in the absence of aerosol-generating procedures is present; however, this mode of transmission has not been universally acknowledged.
- Fomite transmission from contamination of inanimate surfaces with SARS-CoV-2 has been well characterized based on many studies reporting the viability of SARS-CoV-2 on various porous and nonporous surfaces. Under experimental conditions, SARS-CoV-2 was stable on stainless steel and plastic surfaces compared to copper and cardboard surfaces, with the viable virus being detected up to 72 hours after inoculating the surfaces with the virus. [29] The viable virus was isolated for up to 28 days at 20°C from nonporous surfaces such as glass and stainless steel. Conversely, recovery of SARS-CoV-2 on porous materials was reduced compared with nonporous surfaces. [30] In hospital settings, the SARS-CoV-2 has been detected on floors, computer mice, trash cans, sickbed handrails, and in the air (up to 4 meters from patients). [31] The Centers for Disease Control and Prevention (CDC) has stated that individuals can be infected with SARS-CoV-2 via contact with surfaces contaminated by the virus, but the risk is low and is not the main route of transmission of this virus.
- Epidemiologic data from several case studies have reported that patients with SARS-CoV-2 infection have the live virus in feces implying possible fecal-oral transmission. [32]
- A meta-analysis that included 936 neonates from mothers with COVID-19 showed vertical transmission is possible but occurs in a minority of cases. [33]
- Epidemiology
COVID-19 was the third leading cause of death in the United States (USA) in 2020 after heart disease and cancer, with approximately 375,000 deaths. [34]
Individuals of all ages are at risk of contracting this infection. However, patients aged ≥60 and patients with underlying medical comorbidities (obesity, cardiovascular disease, chronic kidney disease, diabetes, chronic lung disease, smoking, cancer, solid organ or hematopoietic stem cell transplant patients) have an increased risk of developing severe COVID-19 infection.
According to the CDC, age remains the strongest predictor of poor outcomes and severe illness in patients with COVID-19. Data from the National Vital Statistics System (NVSS) at CDC states that patients with COVID-19 aged 50 to 64 years have a 25 times higher risk of death when compared to adults infected with this illness and aged less than 30 years. In patients 65 to 74 years old, this risk increases to 60 times. In patients older than 85, the risk of death increases to 340 times. According to the CDC, these data include all deaths in the United States throughout the pandemic, from February 2020 to July 1, 2022, including deaths among unvaccinated individuals.
The percentage of COVID-19 patients requiring hospitalization was 6 times higher in those with preexisting medical conditions than those without medical conditions (45.4% vs. 7.6%) based on an analysis by Stokes et al. of confirmed cases reported to the CDC from January 22 to May 30, 2020. [35] The study also reported that the percentage of patients who succumbed to this illness was 12 times higher in those with preexisting medical conditions than those without (19.5% vs 1.6%). [35]
Data regarding the gender-based differences in COVID-19 suggests that male patients have a higher risk of severe illness and increased mortality due to COVID-19 compared to female patients. [36] [37] Results from a retrospective cohort study from March 1 to November 21, 2020, evaluating the mortality rate in 209 United States of America (USA) acute care hospitals that included 42604 patients with confirmed SARS-CoV-2 infection, reported a higher mortality rate in male patients (12.5%) compared to female patients (9.6%). [38]
Racial and ethnic minority groups have been reported to have a higher percentage of COVID-19-related hospitalizations than White patients based on a recent CDC analysis of hospitalizations from an extensive administrative database that included approximately 300,000 COVID-19 patients hospitalized from March 2020 to December 2020. This high percentage of COVID-19-related hospitalizations among racial and ethnic groups was driven by a higher risk of exposure to SARS-CoV-2 and an increased risk of developing severe COVID-19 disease. [39] A meta-analysis of 50 studies from USA and UK researchers noted that people of Black, Hispanic, and Asian ethnic minority groups are at increased risk of contracting and dying from COVID-19 infection. [40]
COVID-19-related death rates were the highest among Hispanic persons. [34] Another analysis by the CDC evaluating the risk of COVID-19 among sexual minority adults reported that underlying medical comorbidities which increase the risk of developing severe COVID-19 were more prevalent in sexual minority individuals than heterosexual individuals within the general population and within specific racial/ethnic groups. [41]
- Pathophysiology
Structurally and phylogenetically, SARS-CoV-2 is similar to SARS-CoV and MERS-CoV and is composed of 4 main structural proteins: spike (S), envelope (E) glycoprotein, nucleocapsid (N), and membrane (M) protein. It also contains 16 nonstructural proteins and 5-8 accessory proteins. [42]
The surface spike (S) glycoprotein, which resembles a crown, is located on the outer surface of the virion. It undergoes cleavage into an amino (N)-terminal S1 subunit, which facilitates the incorporation of the virus into the host cell. The carboxyl (C)-terminal S2 subunit contains a fusion peptide, a transmembrane domain, and a cytoplasmic domain responsible for virus-cell membrane fusion. [43] [44] The S1 subunit is further divided into a receptor-binding domain (RBD) and an N-terminal domain (NTD), which facilitates viral entry into the host cell and serves as a potential target for neutralization in response to antisera or vaccines . [45]
The RBD is a fundamental peptide in the pathogenesis of infection as it represents a binding site for the human angiotensin-converting enzyme 2 (ACE2) receptors. Inhibition of the renin-angiotensin-aldosterone system (RAAS) does not increase the risk of hospitalization for COVID-19 and severe disease. [46]
SARS-CoV-2 gains entry into the host cells by binding the SARS-CoV-2 spike or S protein (S1) to the ACE2 receptors in the respiratory epithelium. ACE2 receptors are also expressed by other organs such as the upper esophagus, enterocytes from the ileum, myocardial cells, proximal tubular cells of the kidney, and urothelial cells of the bladder. [47] The viral attachment process is followed by priming the spike protein S2 subunit by the host transmembrane serine protease 2 (TMPRSS2) that facilitates cell entry and subsequent viral replication. [48]
In the early phase of the infection, viral replication results in direct virus-mediated tissue damage. In the late phase, the infected host cells trigger an immune response by recruiting T lymphocytes, monocytes, and neutrophils. Cytokines such as tumor necrosis factor-α (TNF α), granulocyte-macrophage colony-stimulating factor (GM-CSF), interleukin-1 (IL-1), interleukin-6 (IL-6), ), IL-1β, IL-8, IL-12 and interferon (IFN)-γ are released. In severe COVID-19 illness, a 'cytokine storm' is seen. This is due to the over-activation of the immune system and high levels of cytokines in circulation. This results in a local and systemic inflammatory response. [49] [50]
Effect of SARS-CoV-2 on the Respiratory System
Increased vascular permeability and subsequent development of pulmonary edema in patients with severe COVID-19 are explained by multiple mechanisms. [51] [52] [53] These mechanisms include:
- Endotheliitis as a result of direct viral injury and perivascular inflammation leading to microvascular and microthrombi deposition
- Dysregulation of RAAS due to increased binding of the virus to the ACE2 receptors
- Activation of the kallikrein-bradykinin pathway, the activation of which enhances vascular permeability
- Enhanced epithelial cell contraction causes swelling of cells and disturbance of intercellular junctions
- The binding of SARS-CoV-2 to the Toll-Like Receptor (TLR) induces the release of pro-IL-1β, which mediates lung inflammation until fibrosis . [54]
Effect of SARS-CoV-2 on Extrapulmonary Organ Systems
Although the respiratory system is the principal target for SARS-CoV-2, other major organ systems such as the gastrointestinal tract (GI), hepatobiliary, cardiovascular, renal, and central nervous systems may also be affected. SARS-CoV-2–induced organ dysfunction is likely due to a combination of mechanisms, such as direct viral toxicity, ischemic injury caused by vasculitis, thrombosis, immune dysregulation, and renin-angiotensin-aldosterone system (RAAS) dysregulation. [55]
Cardiac involvement in COVID-19 is common and likely multifactorial. ACE2 receptors exhibited by myocardial cells may cause direct cytotoxicity to the myocardium leading to myocarditis. Proinflammatory cytokines such as IL-6 can also lead to vascular inflammation, myocarditis, and cardiac arrhythmias. [56]
Acute coronary syndrome (ACS) is a well-recognized cardiac manifestation of COVID-19. It is likely due to multiple factors, including proinflammatory cytokines, worsening of preexisting severe coronary artery disease, coronary plaque destabilization, microthrombogenesis, and reduced coronary blood flow. [57]
SARS-CoV-2 has a significant effect on the hematological and hemostatic systems as well. The mechanism of leukopenia, one of the most common laboratory abnormalities encountered in COVID-19, is unknown. Several hypotheses have been postulated that include ACE 2 mediated lymphocyte destruction by direct invasion by the virus, lymphocyte apoptosis due to proinflammatory cytokines, and possible invasion of the virus in the lymphatic organs. [58]
Thrombocytopenia is common in COVID-19 and is likely due to multiple factors, including virus-mediated suppression of platelets, autoantibodies formation, and coagulation cascade activation, resulting in platelet consumption. [59]
Thrombocytopenia and neutrophilia are considered a hallmark of severe illness. [55] Although it is well known that COVID-19 is associated with a state of hypercoagulability, the exact mechanisms that lead to the activation of the coagulation system are unknown and likely attributed to the cytokine-induced inflammatory response. The pathogenesis of this associated hypercoagulability is multifactorial. The hypercoagulability is probably induced by direct viral-mediated damage or cytokine-induced injury of the vascular endothelium leading to the activation of platelets, monocytes, and macrophages, with increased expression of von Willebrand factor and Factor VIII that results in the generation of thrombin and formation of a fibrin clot. [59] [60]
Other mechanisms that have been proposed include possible mononuclear phagocyte-induced prothrombotic sequelae, derangements in the renin-angiotensin system (RAS) pathways, and complement-mediated microangiopathy. [59]
- History and Physical
Clinical Manifestations of COVID-19
- The median incubation period for SARS-CoV-2 is estimated to be 5.1 days, and most patients will develop symptoms within 11.5 days of infection. [61]
- The clinical spectrum of COVID-19 varies from asymptomatic or paucisymptomatic forms to clinical illness characterized by acute respiratory failure requiring mechanical ventilation, septic shock, and multiple organ failure.
- It is estimated that 17.9% to 33.3% of infected patients will remain asymptomatic. [62] [63]
- Most symptomatic patients present with fever, cough, and shortness of breath. Less common symptoms include sore throat, anosmia, dysgeusia, anorexia, nausea, malaise, myalgias, and diarrhea. Stokes et al. reported that among 373,883 confirmed symptomatic COVID-19 cases in the USA, 70% experienced fever, cough, and shortness of breath, 36% reported myalgia, and 34% reported headache. [35]
- A large meta-analysis evaluating clinicopathological characteristics of 8697 patients with COVID-19 in China reported laboratory abnormalities that included lymphopenia (47.6%), elevated C-reactive protein levels (65.9%), elevated cardiac enzymes (49.4%), and abnormal liver function tests (26.4%). Other laboratory abnormalities included leukopenia (23.5%), elevated D-dimer (20.4%), elevated erythrocyte sedimentation rate (20.4%), leukocytosis (9.9%), elevated procalcitonin (16.7%), and abnormal renal function (10.9%). [64]
- A meta-analysis of 212 published studies with 281,461 individuals from 11 countries/regions reported that severe disease course was noted in about 23% of the patients, with a mortality rate of about 6% in patients infected with COVID-19. [65]
- An elevated neutrophil-to-lymphocyte ratio (NLR), an elevated derived NLR ratio (d-NLR), and an elevated platelet-to-lymphocyte ratio indicate a cytokine-induced inflammatory storm. [66]
Based on the severity of the presenting illness, which includes clinical symptoms, laboratory and radiographic abnormalities, hemodynamics, and organ function, the National Institutes of Health (NIH) issued guidelines that classify COVID-19 into 5 distinct types.[ NIH COVID-19 Treatment Guidelines ]
- Asymptomatic or Presymptomatic Infection : Individuals with positive SARS-CoV-2 test without any clinical symptoms consistent with COVID-19.
- Mild illness : Individuals who have symptoms of COVID-19, such as fever, cough, sore throat, malaise, headache, muscle pain, nausea, vomiting, diarrhea, anosmia, or dysgeusia but without shortness of breath or abnormal chest imaging.
- Moderate illness : Individuals with clinical symptoms or radiologic evidence of lower respiratory tract disease and oxygen saturation (SpO 2 ) ≥94% on room air.
- Severe illness : Individuals who have SpO 2 less than 94% on room air, a ratio of partial pressure of arterial oxygen to fraction of inspired oxygen (PaO 2 /FiO 2 ) of less than 300, marked tachypnea with a respiratory frequency of greater than 30 breaths/min, or lung infiltrates that are greater than 50% of total lung volume.
- Critical illness : Individuals with acute respiratory failure, septic shock, or multiple organ dysfunction. Patients with severe COVID-19 illness may become critically ill with the development of acute respiratory distress syndrome (ARDS). This tends to occur approximately one week after the onset of symptoms.
ARDS is characterized by a severe new-onset respiratory failure or worsening of an already identified respiratory picture. The diagnosis requires bilateral opacities (lung infiltrates >50%), not fully explained by effusions or atelectasis. The Berlin definition classifies ARDS into 3 types based on the degree of hypoxia, with the reference parameter being PaO 2 /FiO 2 or P/F ratio: [67]
- Mild ARDS : 200 mm Hg <PaO 2 /FiO 2 ≤300 mm Hg in patients not receiving mechanical ventilation or in those managed through noninvasive ventilation (NIV) by using positive end-expiratory pressure (PEEP) or a continuous positive airway pressure (CPAP) ≥5 cm H2O.
- Moderate ARDS : 100 mm Hg <PaO 2 /FiO 2 ≤200 mm Hg
- Severe ARDS : PaO 2 /FiO 2 ≤100 mm Hg
When PaO 2 is unavailable, a ratio of SpO 2 /FiO 2 ≤315 suggests ARDS. A multicenter prospective observational study that analyzed 28-day mortality in mechanically ventilated patients with ARDS concluded that COVID-19 patients with ARDS had features similar to other ARDS cohorts, and the risk of 28-day mortality increased with ARDS severity. [68]
Extrapulmonary Manifestations
- Acute kidney injury (AKI) is the most frequently encountered extrapulmonary manifestation of COVID-19 and is associated with an increased mortality risk. [69] A large multicenter cohort study of hospitalized patients with COVID-19 that involved 5,449 patients admitted with COVID-19 reported that 1993 (36.6%) patients developed AKI during their hospitalization, of which 14.3% of patients required renal replacement therapy (RRT). [70]
- Myocardial injury manifesting as myocardial ischemia/infarction (MI) and myocarditis are well-recognized cardiac manifestations in patients with COVID-19. Single-center retrospective study analysis of 187 patients with confirmed COVID-19 reported that 27.8% of patients exhibited myocardial injury indicated by elevated troponin levels. The study also noted that patients with elevated troponin levels had more frequent malignant arrhythmias and a higher mechanical ventilation frequency than patients with normal troponin levels. [71] A meta-analysis of 198 published studies involving 159698 COVID-19 patients reported that acute myocardial injury and a high burden of pre-existing cardiovascular disease were significantly associated with higher mortality and ICU admission. [72]
- Lymphopenia is a common laboratory abnormality in most patients with COVID-19. Other laboratory abnormalities include thrombocytopenia, leukopenia, elevated ESR levels, C-reactive protein (CRP), lactate dehydrogenase (LDH), and leukocytosis.
- COVID-19 is also associated with a hypercoagulable state, evidenced by the high prevalence of venous thromboembolic events. COVID-19 is associated with markedly elevated D-dimer and fibrinogen levels and prolonged prothrombin time (PT) and partial thromboplastin time (aPTT). [71] [55]
- GI symptoms (such as diarrhea, nausea, vomiting), anorexia, and abdominal pain are common. A meta-analysis reported that the weighted pool prevalence of diarrhea was 12.4% (95% CI, 8.2% to 17.1%), nausea or vomiting was 9% (95% CI, 5.5% to 12.9%), loss of appetite was 22.3% (95% CI, 11.2% to 34.6%) and abdominal pain was 6.2% (95% CI, 2.6% to 10.3%). The study also reported that the mortality rate among patients with GI symptoms was similar to the overall mortality rate. [73] Cases of acute mesenteric ischemia and portal vein thrombosis have also been described. [74]
- An acute increase in aspartate transaminase (AST) and alanine transaminase (ALT) is noted in 14% to 53% of patients with COVID-19 infection. [75]
- Guillain-Barré syndrome (GBS) cases from Northern Italy have also been reported. [76] [77]
- Acral lesions resembling pseudo chilblains (40.4%) are the most common cutaneous manifestation noted in patients with COVID-19. [78]
- Other cutaneous manifestations include erythematous maculopapular rash (21.3%), vesicular rashes (13%), urticarial rashes (10.9%), vascular rashes (4%) resembling livedo or purpura, and erythema multiforme-like eruptions (3.7%). [78]
Diagnostic Testing in COVID-19
A nasopharyngeal swab for SARS-CoV-2 nucleic acid using a real-time PCR assay is the standard diagnostic test.[ NIH COVID-19 Treatment Guidelines ] Commercial PCR assays have been authorized by the USA Food and Drug Administration (FDA) for the qualitative detection of SARS-CoV-2 virus using specimens obtained from nasopharyngeal swabs as well as other sites such as oropharyngeal, anterior/mid-turbinate nasal swabs, nasopharyngeal aspirates, bronchoalveolar lavage (BAL) and saliva.
The sensitivity of PCR testing depends on multiple factors, including the specimen's adequacy, time from exposure, and specimen source. [79] However, the specificity of most commercial FDA-authorized SARS-CoV-2 PCR assays is nearly 100%, provided there is no cross-contamination during specimen processing. SARS-CoV-2 antigen tests are less sensitive but have a faster turnaround time than molecular PCR testing. [80]
Despite the numerous antibody tests designed to date, serologic testing has limitations in specificity and sensitivity, and results from different tests vary. According to the NIH guidelines, diagnosing acute SARS-CoV-2 infection based on serologic testing is not recommended. They also stated that there is insufficient evidence to recommend for or against using serologic testing to assess immunity, even if it is used to guide clinical decisions about COVID-19 vaccines/monoclonal antibodies.[ NIH COVID-19 Treatment Guidelines ]
Other Laboratory Assessment
- Complete blood count (CBC), a comprehensive metabolic panel (CMP) that includes renal and liver function testing, and a coagulation panel should be performed in all hospitalized patients.
- Additional tests, such as ESR, C-reactive protein (CRP), ferritin, lactate dehydrogenase, and procalcitonin, can be considered in hospitalized patients. However, their prognostic significance in COVID-19 is not clear.
- A D-dimer level is required as it guides the use of therapeutic versus prophylactic doses of anticoagulation.
Imaging ModalitiesThis s viral illness commonly manifests as pneumonia, so radiological imaging such as chest x-rays, lung ultrasounds, and chest computed tomography (CT) are often obtained. However, there are no guidelines regarding the timing and choice of pulmonary imaging in patients with COVID-19.
When obtained, the chest X-ray usually shows bilateral multifocal alveolar opacities. Pleural effusions can also be demonstrated. The most common CT chest findings in COVID-19 are multifocal bilateral ground glass opacities with consolidation changes, usually in a patchy peripheral distribution. [81]
Radiologic imaging is not a sensitive method for detecting this disease. A retrospective study of 64 patients with documented COVID-19 reported that 20% had no abnormalities on chest radiographs during the illness. [82] A chest CT is more sensitive than a radiograph but is not specific. No finding on radiographic imaging can completely rule in or rule out COVID-19 illness. Therefore the American College of Radiology (ACR) advises against the routine use of chest CT for screening or diagnosis of COVID-19.[ ACR Position Statement for Diagnosis of COVID-19 ]
- Treatment / Management
According to the National Institutes of Health (NIH), the 2 main processes driving the pathogenesis of COVID-19 include replication of the virus in the early phase of the illness and dysregulated immune/inflammatory response to SARS-CoV-2 that leads to systemic tissue damage in the later phase of the disease.[ NIH COVID-19 Treatment Guidelines ] The guidelines, therefore, advise antiviral medications to halt viral replication in the early phase of the illness and immunomodulators in the later phase.
Remdesivir is the only antiviral drug approved by the USA Food and Drug Administration (FDA) to treat COVID-19. Ritonavir-boosted nirmatrelvir, molnupiravir, and high-titer COVID-19 convalescent plasma have Emergency Use Authorizations (EUAs) for treating COVID-19. Tixagevimab 300 mg plus cilgavimab 300 mg monoclonal antibodies have received EUAs that allow them to be used as SARS-CoV-2 preexposure prophylaxis (PrEP) in certain patients.
Many other monoclonal antibodies had EUAs; however, as Omicron subvariants emerged, their EUAs were revoked as they were no longer effective.
The most recent NIH treatment guidelines for the management of COVID-19 illness (accessed on January 3rd, 2023) are outlined below:[ NIH COVID-19 Treatment Guidelines ]
Nonhospitalized Adults With Mild-to-Moderate COVID-19 Illness Who Do Not Require Supplemental Oxygen
- The NIH recommends against using dexamethasone or any other systemic corticosteroids in patients who are not hypoxic. [83]
- Ritonavir-boosted nirmatrelvir is a combination of oral protease inhibitors. It has been shown to reduce hospitalization and death when given to high-risk, unvaccinated, nonhospitalized patients. It must be given within 5 days of symptoms onset. [84]
- It is a strong cytochrome P450 inhibitor with many drug-drug interactions that must be carefully assessed.
- Some interactions can be managed by temporarily holding the medication, some may be managed with dose adjustment, but some may warrant the use of alternate COVID-19 therapy.
- Ritonavir-boosted nirmatrelvir is not recommended in patients with an estimated glomerular filtration rate (eGFR) of less than 30 mL/min.
- The recommended dose is nirmatrelvir 300 mg with ritonavir 100 mg orally twice daily for 5 days.
- This is a nucleotide analog that inhibits the SARS-CoV-2 RNA polymerase
- The recommended duration of therapy in this setting is 3 days.
- The recommended dose is 200 mg IV on day 1, followed by 100 mg IV for 2 more days.
- It is a mutagenic ribonucleoside antiviral agent.
- Fetal toxicity has been reported in animal studies with this agent. Due to the risk of genotoxicity with this agent, it is not recommended in pregnant patients.
- This agent should only be used if both therapies are unavailable or cannot be given.
- The NIH guidelines recommend against using anti-SARS-CoV-2 monoclonal antibodies (mAbs) for treating COVID-19 in this cohort because the Omicron subvariants are not susceptible to these agents.
- Adequate and close medical follow-up is recommended; however, the frequency and duration of follow-up depend on individual risk factors and the severity of their symptoms.
- Risk factors for progression to severe disease include advanced age and underlying medical conditions. The CDC maintains an updated list of medical conditions associated with a high risk of progression.
- Asthma
- Cerebrovascular disease
- Chronic kidney disease
- Bronchiectasis
- COPD (Chronic obstructive pulmonary disease)
- Interstitial lung disease
- Pulmonary embolism
- Pulmonary hypertension
- Nonalcoholic fatty liver disease
- Alcoholic liver disease
- Autoimmune hepatitis
- Cystic fibrosis
- Diabetes, type 1 and 2
- Heart conditions (such as heart failure, coronary artery disease, or cardiomyopathies)
- HIV (Human immunodeficiency virus)
- Mental health conditions such as mood disorders and Schizophrenia spectrum disorders
- Obesity (defined as body mass index (BMI) of greater than 30 kg/m 2 or greater than 95th percentile in children)
- Pregnancy and recent pregnancy
- Smoking, current and former
- Solid organ or blood stem cell transplantation
- Tuberculosis
- Use of corticosteroids or other immunosuppressive medications ( CDC: Underlying Medical Conditions Associated with Higher Risk )
Therapeutic Management of Hospitalized Adults With COVID-19 Who Do Not Require Oxygen
- If patients are hospitalized for reasons other than COVID-19 illness and are not on oxygen, their management is similar to nonhospitalized patients.
- If they are hospitalized for COVID-19 illness but do not require oxygen, the NIH advises against the use of dexamethasone or any other systemic corticosteroid.
- A prophylactic dose of anticoagulation should be given if there is no contraindication.
- If they are hospitalized for COVID-19 illness, do not require oxygen, but are at high risk of progression to severe disease, they should be treated with remdesivir.
- The benefit of remdesivir is greatest when given early, ideally within ten days of symptom onset.
- Remdesivir should be given for 5 days or until hospital discharge.
Therapeutic Management of Hospitalized Adults With COVID-19 Who Require Conventional Oxygen
- Conventional oxygen is defined as oxygen that is NOT high-flow nasal cannula, noninvasive mechanical ventilation, mechanical ventilation, or extracorporeal membrane oxygenation (ECMO)
- For most patients in this cohort, the recommended treatment is dexamethasone plus remdesivir.
- Dexamethasone dose is 6 mg IV or oral (PO) once daily for up to 10 days or until hospital discharge (dexamethasone should not be continued at discharge). [83]
- If the patient is on minimal oxygen, remdesivir monotherapy (without dexamethasone) should be used.
- If remdesivir cannot be obtained or given, dexamethasone monotherapy is recommended.
- If dexamethasone is unavailable, corticosteroids such as prednisone, methylprednisolone, or hydrocortisone may be used.
- If the patient is already receiving dexamethasone but has rapidly increasing oxygen needs and/or signs of systemic inflammation, oral baricitinib or intravenous (IV) tocilizumab should be added to the treatment regimen as these agents have been shown to improve outcomes in rapidly decompensating patients. [85]
- Alternate immunomodulatory agents for this cohort include oral tofacitinib and IV sarilumab. These agents should only be used if baricitinib and tocilizumab are not available.
- If the D-dimer level is above normal in this cohort of patients, they recommend therapeutic anticoagulation if the patient is not pregnant and has no increased risk of bleeding. Contraindications for therapeutic anticoagulation in these patients include a platelet count of less than 50 x10^9 /L, hemoglobin less than 8 g/dL, use of dual antiplatelet therapy, any significant bleeding within the past 30 days, a history of a bleeding disorder or an inherited or active acquired bleeding disorder.
- For pregnant patients, a prophylactic dose of anticoagulation is recommended.
Therapeutic Management of Hospitalized Adults With COVID-19 who Require High-flow Nasal Cannula (HFNC) or Noninvasive Mechanical Ventilation (NIV)
- A meta-analysis study evaluating the effectiveness of HFNC compared to conventional oxygen therapy and NIV before mechanical ventilation reported that HFNC, when used before mechanical ventilation, could improve the prognosis of patients compared to conventional oxygen therapy and NIV. [86] HFNC or NIV is associated with decreased dispersion of exhaled air, especially when used with good interface fitting, thus creating a low risk of nosocomial transmission of the infection. [87] However, these treatment modalities are associated with a greater risk of aerosolization and should be used in negative-pressure rooms. [88]
- According to the NIH, dexamethasone plus oral baricitinib or dexamethasone plus IV tocilizumab are the preferred treatment regimens in these patients.
- Alternate immunomodulatory agents for this cohort include oral tofacitinib and IV sarilumab.
- Dexamethasone monotherapy is recommended if baricitinib, tocilizumab, or sarilumab cannot be obtained/given.
- Clinicians may consider adding remdesivir to corticosteroid and immunomodulator combination regimens in immunocompromised patients who require HFNC or NIV ventilation; however, using remdesivir without immunomodulators is not recommended.
- A prophylactic dose of anticoagulation is recommended in these patients.
- If patients were started on a therapeutic dose of heparin while on conventional oxygen therapy, they should be switched to prophylactic dosing at this time unless they have another indication for full anticoagulation.
Therapeutic Management of Hospitalized Adults With COVID-19 who Require Mechanical Ventilation (MV)
- The management of this cohort is the same as those requiring HFNC or NIV, except that remdesivir is not recommended.
- Remdesivir is most effective earlier in the course of the disease and in patients not on mechanical ventilation or ECMO.
- According to the NIH, one study showed a slight trend toward an increase in mortality in patients who received remdesivir while on mechanical ventilation or ECMO. [89]
- With this data in mind, the NIH recommends against using remdesivir in patients receiving MV or ECMO; however, if the patient was started on remdesivir and progressed to requiring mechanical ventilation or ECMO, they recommended continuing remdesivir to complete the treatment course.
High-Titer COVID-19 Convalescent Plasma (CCP)
- The United States Food and Drug Administration (FDA) approved convalescent plasma therapy under a EUA for patients with severe life-threatening COVID-19. [90] [91] Data from multiple studies evaluating the use of convalescent plasma in life-threatening COVID-19 has generated mixed results. Data from 3 small randomized control trials showed no significant differences in clinical improvement or overall mortality in patients treated with convalescent plasma versus standard therapy. [92] [93] [94]
- According to the NIH, high-titer CCP is not recommended in immunocompetent individuals.
- However, the NIH states that some experts consider it appropriate for use in immunocompromised individuals. Therefore, the current NIH guidelines state that there is insufficient evidence for or against the use of high-titer CCP for treating COVID-19 in hospitalized or nonhospitalized patients who are immunocompromised.
Medications/Treatments That Should NOT Be Used for the Treatment of COVID-19 According to the Latest NIH Guidelines [ NIH COVID-19 Treatment Guidelines ]
- Chloroquine or hydroxychloroquine with or without azithromycin
- Lopinavir/ritonavir
- Azithromycin
- Doxycycline
- Fluvoxamine
- Inhaled corticosteroids
- Excess supplementation of vitamin C, vitamin D, and zinc
- Interferons alfa, beta, or lambda
- Nitazoxanide
- Bamlanivimab plus etesevimab
- Bebtelovimab
- Casirivimab plus imdevimab
Preexposure Prophylaxis for SARS-CoV-2 Infection
- According to the NIH guidelines, tixagevimab plus cilgavimab is authorized by the FDA for preexposure prophylaxis of SARS-CoV-2 in people who are not expected to mount an adequate immune response to COVID-19 vaccination; however, the prevalence of Omicron subvariants that are resistant to tixagevimab plus cilgavimab is noted to be increasing rapidly.
- In the absence of alternative options, the NIH still recommends tixagevimab 300 mg plus cilgavimab 300 mg at this time.
- Tixagevimab and cilgavimab are potent anti-spike neutralizing monoclonal antibodies obtained from antibodies isolated from B cells of patients infected with SARS-CoV-2 that have demonstrated neutralizing activity against SARS-CoV-2 virus by binding to nonoverlapping epitopes of the viral spike-protein RBD. [95] [96] [97]
- The EUA authorizes its use in adult and pediatric patients with no current evidence of SARS-CoV-2 infection and no recent exposure to SARS-CoV-2-positive individuals. They must be moderately or severely immunocompromised or be on immunosuppressive medications.
- Differential Diagnosis
The symptoms of the early stages of the disease are nonspecific. Differential diagnosis should include the possibility of a wide range of infectious and noninfectious respiratory disorders.
- Community-acquired bacterial pneumonia
- Viral pneumonia
- Influenza infection
- Aspiration pneumonia
- Pneumocystis jirovecii pneumonia
- Middle East respiratory syndrome (MERS)
- Avian influenza A (H7N9) viral infection
- Avian influenza A (H5N1) viral infection
- Pulmonary tuberculosis
The prognosis of COVID-19 depends on various factors, including the patient's age, the severity of illness at presentation, preexisting conditions, how quickly treatment can be implemented, and response to treatment. The WHO currently estimates the global case fatality rate for COVID-19 is 2.2%. Results from a European multicenter prospective cohort study that included 4000 critically ill patients with COVID-19 reported a 90-day mortality of 31%, with higher mortality noted in geriatric patients and patients with diabetes, obesity, and severe ARDS. [98]
- Complications
COVID-19 is a systemic viral illness based on its involvement in multiple major organ systems.
- Patients with advanced age and comorbid conditions such as obesity, diabetes mellitus, chronic lung disease, cardiovascular disease, chronic kidney disease, chronic liver disease, and neoplastic conditions are at risk of developing severe COVID-19 and its associated complications. The most common complication of severe COVID-19 illness is progressive or sudden clinical deterioration leading to acute respiratory failure and ARDS or multiorgan failure leading to death.
- Patients with COVID-19 illness are also at increased risk of developing prothrombotic complications such as pulmonary embolisms, myocardial infarctions, ischemic strokes, and arterial thrombosis. [55]
- Cardiovascular system involvement results in malignant arrhythmias, cardiomyopathy, and cardiogenic shock.
- GI complications such as bowel ischemia, transaminitis, gastrointestinal bleeding, pancreatitis, Ogilvie syndrome, mesenteric ischemia, and severe ileus are often noted in critically ill patients with COVID-19. [99]
- Acute renal failure is the most common extrapulmonary manifestation of COVID-19 and is associated with an increased mortality risk. [69]
- A meta-analysis study of 14 studies evaluating the prevalence of disseminated intravascular coagulation (DIC) in hospitalized patients with COVID-19 reported that DIC was observed in 3% (95%: 1%-5%, P <0.001) of the included patients. Additionally, DIC was noted to be associated with severe illness and was a poor prognostic indicator. [100]
- More recent data have emerged regarding prolonged symptoms in patients who have recovered from COVID-19 infection, termed "post-acute COVID-19 syndrome." A large cohort study of 1773 patients performed 6 months after hospitalization with COVID-19 revealed that most exhibited at least one persistent symptom: fatigue, muscle weakness, sleep difficulties, or anxiety. Patients with severe illness also had an increased risk of chronic lung issues. [101]
- A retrospective cohort study that included 236,379 patients reported substantial neurological (intracranial hemorrhage, ischemic stroke) and psychiatric morbidity (anxiety disorder, psychotic disorder) 6 months after being diagnosed with COVID-19. [102]
- Secondary invasive fungal infections such as COVID-19-associated pulmonary aspergillosis and rhino-cerebro-orbital mucormycosis have increasingly been reported as complications in patients recovering from COVID-19. Risk factors for developing secondary fungal infection include comorbid conditions such as uncontrolled diabetes, associated lymphopenia, and excessive use of corticosteroids.
- Deterrence and Patient Education
The NIH COVID-19 Treatment Guidelines recommend COVID-19 vaccination as soon as possible for all eligible individuals. The CDC’s Advisory Committee on Immunization Practices (AI) determines eligibility eligibility. Four vaccines are authorized or approved in the United States to prevent COVID-19. According to the NIH guidelines, the preferred vaccines include:[ NIH COVID-19 Treatment Guidelines ]
- mRNA vaccine BNT162b2 (Pfizer-BioNTech)
- mRNA-1273 (Moderna)
- Recombinant spike protein with matrix-M1 adjuvant vaccine NVX-CoV2373 (Novavax)
The adenovirus vector vaccine Ad26.COV2.S (Johnson & Johnson/Janssen) is less preferred due to its risk of serious adverse events.[ NIH COVID-19 Treatment Guidelines ]
A primary series of COVID-19 vaccination is recommended for everyone older than 6 months in the United States. Bivalent mRNA vaccines that protect against the original SARS-CoV-2 virus strain and Omicron subvariants are recommended at least 2 months after receiving the primary vaccine series or a booster dose.[ NIH COVID-19 Treatment Guidelines ]
- Enhancing Healthcare Team Outcomes
SARS-CoV-2 and its variants continue to cause significant morbidity and mortality worldwide. Prevention and management of this highly transmissible respiratory viral illness require a holistic and interprofessional approach that includes physicians' expertise across specialties, nurses, pharmacists, public health experts, and government authorities. There should be open communication among the clinical providers, pharmacists, and nursing staff while managing patients with COVID-19. Each team member should strive to keep abreast of the latest recommendations and guidelines and be free to speak up if they notice anything that does not comply with the latest tenets for managing COVID patients; there is no place for a hierarchy in communication that prohibits any team member from voicing their concerns. This open interprofessional approach will yield the best outcomes.
Clinical providers managing COVID-19 patients on the frontlines should keep themselves periodically updated with the latest clinical guidelines about diagnostic and therapeutic options available in managing COVID-19, especially considering the emergence of new SARS-CoV-2 variants, which could significantly impact morbidity and mortality. Continued viral surveillance of new variants is crucial at regular intervals with viral genomic sequencing, given the possibility that more highly transmissible, more virulent, and treatment-resistant variants could emerge that can have a more catastrophic effect on global health in addition to the current scenario. A multi-pronged approach involving interprofessional team members can improve patient care and outcomes for this potentially devastating disease and help the world end this pandemic.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Covid 19, Corona Replication Contributed by Rohan Bir Singh, MD
Clinical Presentation of Patients with CoVID-19 Contributed by Rohan Bir Singh, MD; Made with Biorender.com
SARS- CoV 2 Structure Contributed by Rohan Bir Singh, MD; Made with Biorender.com
Transmission Cycle of SARS CoV 2 Contributed by Rohan Bir Singh, MD; Made with Biorender.com
Single-stranded RNA genome of SARS-CoV2 Contributed by Rohan Bir Singh, MD; Made with Biorender.com
Disclosure: Marco Cascella declares no relevant financial relationships with ineligible companies.
Disclosure: Michael Rajnik declares no relevant financial relationships with ineligible companies.
Disclosure: Abdul Aleem declares no relevant financial relationships with ineligible companies.
Disclosure: Scott Dulebohn declares no relevant financial relationships with ineligible companies.
Disclosure: Raffaela Di Napoli declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Cascella M, Rajnik M, Aleem A, et al. Features, Evaluation, and Treatment of Coronavirus (COVID-19) [Updated 2023 Aug 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review The Biological Functions and Clinical Significance of SARS-CoV-2 Variants of Corcern. [Front Med (Lausanne). 2022] Review The Biological Functions and Clinical Significance of SARS-CoV-2 Variants of Corcern. Akkız H. Front Med (Lausanne). 2022; 9:849217. Epub 2022 May 20.
- Emerging Variants of SARS-CoV-2 and Novel Therapeutics Against Coronavirus (COVID-19). [StatPearls. 2024] Emerging Variants of SARS-CoV-2 and Novel Therapeutics Against Coronavirus (COVID-19). Aleem A, Akbar Samad AB, Vaqar S. StatPearls. 2024 Jan
- Review Molecular evolution of SARS-CoV-2 from December 2019 to August 2022. [J Med Virol. 2023] Review Molecular evolution of SARS-CoV-2 from December 2019 to August 2022. Wolf JM, Wolf LM, Bello GL, Maccari JG, Nasi LA. J Med Virol. 2023 Jan; 95(1):e28366.
- Unraveling the Dynamics of Omicron (BA.1, BA.2, and BA.5) Waves and Emergence of the Deltacton Variant: Genomic Epidemiology of the SARS-CoV-2 Epidemic in Cyprus (Oct 2021-Oct 2022). [Viruses. 2023] Unraveling the Dynamics of Omicron (BA.1, BA.2, and BA.5) Waves and Emergence of the Deltacton Variant: Genomic Epidemiology of the SARS-CoV-2 Epidemic in Cyprus (Oct 2021-Oct 2022). Chrysostomou AC, Vrancken B, Haralambous C, Alexandrou M, Gregoriou I, Ioannides M, Ioannou C, Kalakouta O, Karagiannis C, Marcou M, et al. Viruses. 2023 Sep 15; 15(9). Epub 2023 Sep 15.
- Mutations of SARS-CoV-2 Structural Proteins in the Alpha, Beta, Gamma, and Delta Variants: Bioinformatics Analysis. [JMIR Bioinform Biotechnol. 2023] Mutations of SARS-CoV-2 Structural Proteins in the Alpha, Beta, Gamma, and Delta Variants: Bioinformatics Analysis. Khetran SR, Mustafa R. JMIR Bioinform Biotechnol. 2023; 4:e43906. Epub 2023 Jul 14.
Recent Activity
- Features, Evaluation, and Treatment of Coronavirus (COVID-19) - StatPearls Features, Evaluation, and Treatment of Coronavirus (COVID-19) - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
COMMENTS
Case 17-2020: A 68-Year-Old Man with Covid-19 and Acute Kidney Injury. Authors: ... among patients with Covid-19, chest imaging studies may show peripheral lung opacities without radiographically ...
Literature regarding post-traumatic stress disorder (PTSD) related to the Covid-19 pandemic is accruing rapidly, but this diagnosis is not plausible in this case, given that the DSM-5 criteria for ...
In patients with Covid-19, an elevated d-dimer level has been associated with numerous poor outcomes, including ICU admission, the need for mechanical ventilation, thrombosis, bleeding, and death ...
Today's report (5th April 2020; daily updates in the prepared website) shows that the confirmed cases of COVID‐19 in the United States, Spain, Italy, and Germany are 308850, 126168, 124632, and 96092, respectively. Calculating the total case fatality rate (CFR) of Italy (4th April 2020), about 13.3% of confirmed cases have passed away.
This case study of severe Covid-19 pneumonia and CRS illustrates some of the diagnostic and therapeutic challenges and controversies regarding the management of this novel and complex infection. Meticulous monitoring for and early treatment of the hyperinflammatory phase of the disease may be crucial in preventing progression to severe ARDS ...
Technical guidance. Unity Studies: Early Investigation Protocols. Case management. National laboratories. Surveillance, rapid response teams, and case investigation. Infection prevention and control. Points of entry and mass gatherings. Naming the coronavirus disease (COVID-19) and the virus that causes it.
Coronavirus Disease (COVID-19) Best Practice Case Studies. The COVID-19 incident period ended on May 11, 2023. FEMA will continue to provide funeral assistance until Sept. 30, 2025, to those who have lost loved ones due to this pandemic. The following is a collection of key findings and considerations for jurisdictions and communities regarding ...
In a recent case report, an infant delivered from a COVID-19-positive mother was tested negative for 7 samples of pharynx, blood, and stool; on the other hand, some studies demonstrated that immunoglobulin M against SARS-CoV-2 was detected in blood samples of newborns; therefore, vertical transmission of SARS-CoV-2 is still a matter of conflict ...
A recent study found that almost half of the 99 hospitalized patients infected with COVID-19 showed liver involvement; the cause of elevated aminotransferase serum levels remains unclear, but it may be due to liver damage by COVID-19 or by antiviral drugs (Table 2). In our case series, eight (20%) patients had diarrhea, but only one (3% ...
COVID-19 case data: From the 31 December 2019 to the 21 March 2020, WHO collected the numbers of confirmed COVID-19 cases and deaths through official communications under the International Health Regulations (IHR, 2005), complemented by monitoring the official ministries of health websites and social media accounts. Since 22 March 2020, global ...
Epidemiological studies have indicated human-to-human transmission in China and elsewhere. To aid the analysis and tracking of the COVID-19 epidemic we collected and curated individual-level data ...
Viet Nam: a primary health care case study in the context of the COVID-19 pandemic. Since 2020, the COVID-19 pandemic has showcased the importance of primary health care (PHC) and revealed health system strengths as well as weaknesses. As a defining global and national policy priority, COVID-19 has had enormous impacts on country health systems ...
This case series study examines the epidemiology, clinical, and laboratory features of children hospitalized with coronavirus disease 2019 (COVID-19) in ... of whom 9 (18%) had an exposure to an individual with a confirmed case of COVID-19. No patient had a history of international travel within 14 days before symptom onset. Two parents ...
Overall, when COVID-19 articles were stratified by study design, a mean case series score (out of 5) (SD) of 3.3 (1.1), mean NOS cohort study score (out of 8) of 5.8 (1.5), mean NOS case-control ...
One study using a US electronic medical database identified an increased risk for a number of autoimmune diseases among patients with COVID-19; another study published using the same database found a decreased risk of incident inflammatory bowel diseases following COVID-19. No study assessed the effect of COVID-19 vaccine on the occurrence of ...
An outbreak of novel coronavirus (2019-nCoV) that began in Wuhan, China, has spread rapidly, with cases now confirmed in multiple countries. We report the first case of 2019-nCoV infection confirme...
3 Discussion. COVID-19 is the cause of severe viral pneumonia rapidly leading to ARDS. In a case series of 135 patients, Wan et al reported 88.9% of patients presented with a fever and 76.5% had a cough. Fatigue and myalgias (32.5%), headache (17.7%), and dyspnea (13.3%) were less commonly reported. These symptoms were also found on presentation with our patient.
Covid-19 Epidemiological DataAs of 16 March 2021, there have been 62,377 confirmed cases of COVID-19 with 1,954 deaths reported to WHO. m El-Salvador (CFR: 3.1%). In the past week, there have been 1,286 new cases with 51 new deaths - represents approx. 38% increase in incident cases and a 9% increase in incident deaths this past we.
Our study provides a new and promising direction for building effective and interpretable data-driven models for COVID-19 cases, which could have significant implications for public health policy ...
Oliguria developed. Additional laboratory studies were obtained . Urgent management decisions were made. ... First case of COVID-19 complicated with fulminant myocarditis: a case report and ...
We conducted a retrospective case-control study by drawing persons with COVID-19 cases and noninfected controls from a cohort of contact tracing records of the central SRRT team at the Department of Disease Control (DDC), MoPH, Thailand. ... The last date that a COVID-19 case was detected was April 9, 2020. Among the 839 controls, 695 (82.8% ...
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
After the onset of the COVID-19 pandemic, both the United States and Canada implemented policies to limit elective surgical procedures with the aim to free up resources to aid in the care of patients with COVID-19. 4,5,7 This study found that in the 16 months after the COVID-19 pandemic was declared, the total number of elective hand surgeries ...
To evaluate the effectiveness of mRNA vaccines in preventing Covid-19 among health care personnel in the United States, we conducted a multisite, test-negative case-control study involving ...
The social and emotional effects of the Covid-19 pandemic on teenagers may have resulted in accelerated brain aging in adolescents, according to a new study.
Case Study; Jul 17, 2024; Knocking Down Public Health and Health Care Silos: An Innovative Covid-19 Health Equity Response ... Coronavirus (Covid-19): Stay current with the latest clinical research and resources from our sister publications, the New England Journal of Medicine coronavirus page and NEJM Journal Watch. JOURNAL
Coronavirus disease 2019 (COVID-19) is a highly contagious viral illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 has had a catastrophic effect on the world, resulting in more than 6 million deaths worldwide. After the first cases of this predominantly respiratory viral illness were reported in Wuhan, Hubei Province, China, in late December 2019, SARS ...