Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Topic collections
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 13, Issue 2
- Qualitative Research Methods in Mental Health
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Sarah Peters
- Correspondence to : Dr Sarah Peters, School of Psychological Sciences, The University of Manchester, Coupland Building 1, Oxford Road M13 9PL, UK; sarah.peters{at}manchester.ac.uk
As the evidence base for the study of mental health problems develops, there is a need for increasingly rigorous and systematic research methodologies. Complex questions require complex methodological approaches. Recognising this, the MRC guidelines for developing and testing complex interventions place qualitative methods as integral to each stage of intervention development and implementation. However, mental health research has lagged behind many other healthcare specialities in using qualitative methods within its evidence base. Rigour in qualitative research raises many similar issues to quantitative research and also some additional challenges. This article examines the role of qualitative methods within mental heath research, describes key methodological and analytical approaches and offers guidance on how to differentiate between poor and good quality qualitative research.
https://doi.org/10.1136/ebmh.13.2.35
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
The trajectory of qualitative methods in mental health research
Qualitative methodologies have a clear home within the study of mental health research. Early and, arguably, seminal work into the study of mental illnesses and their management was based on detailed observation, moving towards theory using inductive reasoning. Case studies have been long established in psychiatry to present detailed analysis of unusual cases or novel treatments. Participant observation was the principle method used in Goffman's seminal study of psychiatric patients in asylums that informed his ideas about the institutionalising and medicalising of mental illness by medical practice. 1 However, the 20th century saw the ‘behaviourist revolution’, a movement where quantification and experimentation dominated. Researchers sought to identify cause and effects, and reasoning became more deductive – seeking to use data to confirm theory. The study of health and illness was determined by contemporary thinking about disease, taking a biomedical stance. Psychologists and clinical health researchers exploited natural science methodologies, attempting to measure phenomenon in their smallest entities and do so as objectively as possible. This reductionist and positivist philosophy shaped advances in research methods and meant that qualitative exploration failed to develop as a credible scientific approach. Indeed, ‘objectivity’ and the ‘discovery of truth’ have become synonymous with ‘scientific enquiry’ and qualitative methods are easily dismissed as ‘anecdotal’. The underlying epistemology of this approach chimes well with medical practice for which training is predominately in laboratory and basic sciences (such as physics and chemistry) within which the discourse of natural laws dominate. To this end, research in psychiatry still remains overwhelmingly quantitative. 2
Underlying all research paradigms are assumptions. However, most traditional researchers remain unaware of these until they start to use alternative paradigms. Key assumptions of quantitative research are that facts exist that can be quantified and measured and that these should be examined, as far as possible, objectively, partialling out or controlling for the context within which they exist. There are research questions within mental health where this approach can hold: where phenomenon of interest can be reliably and meaningfully quantified and measured, it is feasible to use data to test predictions and examine change. However, for many questions these assumptions prove unsatisfying. It is often not possible or desirable to try and create laboratory conditions for the research; indeed it would be ecologically invalid to do so. For example, to understand the experience of an individual who has been newly diagnosed with schizophrenia, it is clearly important to consider the context within which they live, their family, social grouping and media messages they are exposed to. Table 1 depicts the key differences between the two methodological approaches and core underlying assumptions for each.
- View inline
Comparison of underlying assumptions of quantitative and qualitative research approaches
It should be cautioned that it is easy to fall into the trap of categorising studies as either quantitative or qualitative. The two traditions are often positioned within the literature as opposing and in conflict. This division is unhelpful and likely to impede methodological advancement. Though, undeniably, there are differences in the two approaches to research, there are also many exceptions that expose this dichotomy to be simplistic: some qualitative studies seek to test a priori hypotheses, and some quantitative studies are atheoretical and exploratory. 3 Hence it is more useful to consider research methodologies as lying along a spectrum and that researchers should be familiar with the full range of methodologies, so that a method is chosen according to the research question rather than the researcher's ability.
Rationale for qualitative methods in current mental health research
There are a number of scientific, practical and ethical reasons why mental health is an area that can particularly benefit from qualitative enquiry. Mental health research is complex. Health problems are multifactorial in their aetiology and the consequences they have on the individual, families and societies. Management can involve self-help, pharmacological, educative, social and psychotherapeutic approaches. Services involved are often multidisciplinary and require liaison between a number of individuals including professionals, service-users and relatives. Many problems are exacerbated by poor treatment compliance and lack of access to, or engagement with, appropriate services. 4
Engagement with mental health research can also be challenging. Topics may be highly sensitive or private. Individuals may have impaired capacity or be at high risk. During the research process there may be revelations of suicidal ideation or criminal activity. Hence mental health research can raise additional ethical issues. In other cases scepticism of services makes for reluctant research participants. However, if we accept the case that meaningful research can be based in subjective enquiry then qualitative methods provide a way of giving voice to participants. Qualitative methods offer an effective way of involving service-users in developing interventions for mental health problems 5 ensuring that the questions asked are meaningful to individuals. This may be particularly beneficial if participants are stakeholders, for example potential users of a new service.
Qualitative methods are valuable for individuals who have limited literacy skills who struggle with pencil and paper measures. For example qualitative research has proved fruitful in understanding children's concepts of mental illness and associated services. 6
How qualitative enquiry is used within mental health research
There are a range of types of research question where qualitative methods prove useful – from the development and testing of theory, to the piloting and establishing efficacy of treatment approaches, to understanding issues around translation and implementation into routine practice. Each is discussed in turn.
Development and testing of theory
Qualitative methods are important in exploratory work and in generating understanding of a phenomenon, stimulating new ideas or building new theory. For example, stigma is a concept that is recognised as a barrier to accessing services and also an added burden to mental health. A focus-group study sought to understand the meaning of stigma from the perspectives of individuals with schizophrenia, their relatives and health professionals. 7 From this they developed a four-dimensional theory which has subsequently informed interventions to reduce stigma and discrimination that target not only engagement with psychiatric services but also interactions with the public and work. 7
Development of tools and measures
Qualitative methods access personal accounts, capturing how individuals talk about a lived experience. This can be invaluable for designing new research tools. For example, Mavaddat and colleagues used focus groups with 56 patients with severe or common mental health problems to explore their experiences of primary care management. 8 Nine focus groups were conducted and analysis identified key themes. From these, items were generated to form a Patient Experience Questionnaire, of which the psychometric properties were subsequently examined quantitatively in a larger sample. Not only can dimensions be identified, the rich qualitative data provide terminology that is meaningful to service users that can then be incorporated into question items.
Development and testing of interventions
As we have seen, qualitative methods can inform the development of new interventions. The gold-standard methodology for investigating treatment effectiveness is the randomised controlled trial (RCT), with the principle output being an effect size or demonstration that the primary outcome was significantly improved for participants in the intervention arm compared with those in the control/comparison arm. Nevertheless, what will be familiar for researchers and clinicians involved in trials is that immense research and clinical learning arises from these substantial, often lengthy and expensive research endeavours. Qualitative methods provide a means to empirically capture these lessons, whether they are about recruitment, therapy training/supervision, treatment delivery or content. These data are essential to improve the feasibility and acceptability of further trials and developing the intervention. Conducting qualitative work prior to embarking on an RCT can inform the design, delivery and recruitment, as well as engage relevant stakeholders early in the process; all of these can prevent costly errors. Qualitative research can also be used during a trial to identify reasons for poor recruitment: in one RCT, implementing findings from this type of investigation led to an increased randomisation rate from 40% to 70%. 9
Nesting qualitative research within a trial can be viewed as taking out an insurance policy as data are generated which can later help explain negative or surprising findings. A recent trial of reattribution training for GPs to manage medically unexplained symptoms demonstrated substantial improvements in GP consultation behaviour. 10 However, effects on clinical outcomes were counterintuitive. A series of nested qualitative studies helped shed light as to why this was the case: patients' illness models were complex, and they resisted engaging with GPs (who they perceived as having more simplistic and dualistic understanding) because they were anxious it would lead to non-identification or misdiagnosis of any potential future disease 11 , an issue that can be addressed in future interventions. Even if the insights are unsurprising to those involved in the research, the data collected have been generated systematically and can be subjected to peer review and disseminated. For this reason, there is an increasing expectation from funding bodies that qualitative methodologies are integral to psychosocial intervention research.
Translation and implementation into clinical practice
Trials provide limited information about how treatments can be implemented into clinical practice or applied to another context. Psychological interventions are more effective when delivered within trial settings by experts involved in their development than when they are delivered within clinical settings. 12 Qualitative methods can help us understand how to implement research findings into routine practice. 13
Understanding what stakeholders value about a service and what barriers exist to its uptake is another evidence base to inform clinicians' practice. Relapse prevention is an effective psychoeducation approach that helps individuals with bipolar disorder extend time to relapse. Qualitative methodologies identified which aspects of the intervention service-users and care-coordinators value, and hence, are likely to utilise in routine care. 14 The intervention facilitated better understanding of bipolar disorder (by both parties), demonstrating, in turn, a rationale for medication. Patients discovered new, empowering and less socially isolated ways of managing their symptoms, which had important impacts on interactions with healthcare staff and family members. Furthermore, care-coordinators' reported how they used elements of the intervention when working with clients with other diagnoses. The research also provided insights as to where difficulties may occur when implementing a particular intervention into routine care. For example, for care-coordinators this proved a novel way of working with clients that was more emotionally demanding, thus highlighting the need for supervision and managerial support. 14
Beginners guide to qualitative approaches: one size doesn't fit all
Just as there is a range of quantitative research designs and statistical analyses to choose from, so there are many types of qualitative methods. Choosing a method can be daunting to an inexperienced or beginner-level qualitative researcher, for it requires engaging with new terms and ways of thinking about knowledge. The following summary sets out analytic and data-generation approaches that are used commonly in mental health research. It is not intended to be comprehensive and is provided only as a point of access/familiarisation to researchers less familiar with the literature.
Data generation
Qualitative data are generated in several ways. Most commonly, researchers seek a sample and conduct a series of individual in-depth interviews, seeking participants' views on topics of interest. Typically these last upwards of 45 min and are organised on the basis of a schedule of topics identified from the literature or pilot work. This does not act as a questionnaire, however; rather, it acts as a flexible framework for exploring areas of interest. The researcher combines open questions to elicit free responses, with focused questions for probing and prompting participants to provide effective responses. Usually interviews are audio-recorded and transcribed verbatim for subsequent analysis.
As interviews are held in privately, and on one-to-one basis, they provide scope to develop a trusting relationship so that participants are comfortable disclosing socially undesirable views. For example, in a study of practice nurses views of chronic fatigue syndrome, some nurses described patients as lazy or illegitimate – a view that challenges the stereotype of a nursing professional as a sympathetic and caring person. 15 This gives important information about the education and supervision required to enable or train general nurses to ensure that they are capable of delivering psychological interventions for these types of problems.
Alternatively, groups of participants are brought together for a focus group, which usually lasts for 2 hours. Although it is tempting to consider focus groups as an efficient way of acquiring data from several participants simultaneously, there are disadvantages. They are difficult to organise for geographically dispersed or busy participants, and there are compromises to confidentiality, particularly within ‘captive’ populations (eg, within an organisation individuals may be unwilling to criticise). Group dynamics must be considered; the presence of a dominant or self-professed expert can inhibit the group and, therefore, prevent useful data generation. When the subject mater is sensitive, individuals may be unwilling to discuss experiences in a group, although it often promotes a shared experience that can be empowering. Most of these problems are avoided by careful planning of the group composition and ensuring the group is conducted by a highly skilled facilitator. Lester and colleagues 16 used focus-group sessions with patients and health professionals to understand the experience of dealing with serious mental illness. Though initially participants were observed via focus-group sessions that used patient-only and health professional only groups, subsequently on combined focus groups were used that contained both patients and health professionals. 16 The primary advantage of focus groups is that they enable generation of data about how individuals discuss and interact about a phenomenon; thus, a well-conducted focus group can be an extremely rich source of data.
A different type of data are naturally occurring dialogue and behaviours. These may be recorded through observation and detailed field notes (see ethnography in Table 2 ) or analysed from audio/ video-recordings. Other data sources include texts, for example, diaries, clinical notes, Internet blogs and so on. Qualitative data can even be generated through postal surveys. We thematically analysed responses to an open-ended question set within a survey about medical educators' views of behavioural and social sciences (BSS). 17 From this, key barriers to integrating BSS within medical training were identified, which included an entrenched biomedical mindset. The themes were analysed in relation to existing literature and revealed that despite radical changes in medical training, the power of the hidden curriculum persists. 17
Key features of a range of analytical approaches used within mental health research
Analysing qualitative data
Researchers bring a wide range of analytical approaches to the data. A comprehensive and detailed discussion of the philosophy underlying different methods is beyond the scope of this paper; however, a summary of the key analytical approaches used in mental health research are provided in Table 2 . An illustrative example is provided for each approach to offer some insight into the commonalities and differences between methodologies. The procedure for analysis for all methods involves successive stages of data familiarisation/immersion, followed by seeking and reviewing patterns within the data, which may then be defined and categorized as specific themes. Researchers move back and forth between data generation and analysis, confirming or disconfirming emerging ideas. The relationship of the analysis to theory-testing or theory-building depends on the methodology used.
Some approaches are more common in healthcare than others. Interpretative phenomenological (lPA) analysis and thematic analysis have proved particularly popular. In contrast, ethnographic research requires a high level of researcher investment and reflexivity and can prove challenging for NHS ethic committees. Consequently, it remains under used in healthcare research.
Recruitment and sampling
Quantitative research is interested in identifying the typical, or average. By contrast, qualitative research aims to discover and examine the breadth of views held within a community. This includes extreme or deviant views and views that are absent. Consequently, qualitative researchers do not necessarily (though in some circumstances they may) seek to identify a representative sample. Instead, the aim may be to sample across the range of views. Hence, qualitative research can comment on what views exist and what this means, but it is not possible to infer the proportions of people from the wider population that hold a particular view.
However, sampling for a qualitative study is not any less systematic or considered. In a quantitative study one would take a statistical approach to sampling, for example, selecting a random sample or recruiting consecutive referrals, or every 10th out-patient attendee. Qualitative studies, instead, often elect to use theoretical means to identify a sample. This is often purposive; that is, the researcher uses theoretical principles to choose the attributes of included participants. Healey and colleagues conducted a study to understand the reasons for individuals with bipolar disorder misusing substances. 18 They sought to include participants who were current users of each substance group, and the recruitment strategy evolved to actively target specific cases.
Qualitative studies typically use far smaller samples than quantitative studies. The number varies depending on the richness of the data yielded and the type of analytic approach that can range from a single case to more than 100 participants. As with all research, it is unethical to recruit more participants than needed to address the question at hand; a qualitative sample should be sufficient for thematic saturation to be achieved from the data.
Ensuring that findings are valid and generalisable
A common question from individuals new to qualitative research is how can findings from a study of few participants be generalised to the wider population? In some circumstances, findings from an individual study (quantitative or qualitative) may have limited generalisability; therefore, more studies may need to be conducted, in order to build local knowledge that can then be tested or explored across similar groups. 4 However, all qualitative studies should create new insights that have theoretical or clinical relevance which enables the study to extend understanding beyond the individual participants and to the wider population. In some cases, this can lead to generation of new theory (see grounded theory in Table 2 ).
Reliability and validity are two important ways of ascertaining rigor in quantitative research. Qualitative research seeks to understand individual construction and, by definition, is subjective. It is unlikely, therefore, that a study could ever be repeated with exactly the same circumstances. Instead, qualitative research is concerned with the question of whether the findings are trustworthy; that is, if the same circumstances were to prevail, would the same conclusions would be drawn?
There are a number of ways to maximise trustworthiness. One is triangulation, of which there are three subtypes. Data triangulation involves using data from several sources (eg, interviews, documentation, observation). A research team may include members from different backgrounds (eg, psychology, psychiatry, sociology), enabling a range of perspectives to be used within the discussion and interpretation of the data. This is termed researcher triangulation . The final subtype, theoretical triangulation, requires using more than one theory to examine the research question. Another technique to establish the trustworthiness of the findings is to use respondent validation. Here, the final or interim analysis is presented to members of the population of interest to ascertain whether interpretations made are valid.
An important aspect of all qualitative studies is researcher reflexivity. Here researchers consider their role and how their experience and knowledge might influence the generation, analysis and interpretation of the data. As with all well-conducted research, a clear record of progress should be kept – to enable scrutiny of recruitment, data generation and development of analysis. However, transparency is particularly important in qualitative research as the concepts and views evolve and are refined during the process.
Judging quality in qualitative research
Within all fields of research there are better and worse ways of conducting a study, and range of quality in mental health qualitative research is variable. Many of the principles for judging quality in qualitative research are the same for judging quality in any other type of research. However, several guidelines have been developed to help readers, reviewers and editors who lack methodological expertise to feel more confident in appraising qualitative studies. Guidelines are a prerequisite for the relatively recent advance of methodologies for systematic reviewing of qualitative literature (see meta-synthesis in Table 2 ). Box 1 provides some key questions that should be considered while studying a qualitative report.
Box 1 Guidelines for authors and reviewers of qualitative research (adapted from Malterud 35 )
▶ Is the research question relevant and clearly stated?
Reflexivity
▶ Are the researcher's motives and background presented?
Method, sampling and data collection
▶ Is a qualitative method appropriate and justified?
▶ Is the sampling strategy clearly described and justified?
▶ Is the method for data generation fully described
▶ Are the characteristics of the sample sufficiently described?
Theoretical framework
▶ Was a theoretical framework used and stated?
▶ Are the principles and procedures for data organisation and analysis described and justified?
▶ Are strategies used to test the trustworthiness of the findings?
▶ Are the findings relevant to the aim of the study?
▶ Are data (e.g. quotes) used to support and enrich the findings?
▶ Are the conclusions directly linked to the study? Are you convinced?
▶ Do the findings have clinical or theoretical value?
▶ Are findings compared to appropriate theoretical and empirical literature?
▶ Are questions about the internal and external validity and reflexivity discussed?
▶ Are shortcomings of the design, and the implications these have on findings, examined?
▶ Are clinical/theoretical implications of the findings made?
Presentation
▶ Is the report understandable and clearly contextualised?
▶ Is it possible to distinguish between the voices of informants and researchers?
▶ Are sources from the field used and appropriately referenced?
Conclusions and future directions
Qualitative research has enormous potential within the field of mental health research, yet researchers are only beginning to exploit the range of methods they use at each stage of enquiry. Strengths of qualitative research primarily lie in developing theory and increasing understanding about effective implementation of treatments and how best to support clinicians and service users in managing mental health problems. An important development in the field is how to integrate methodological approaches to address questions. This raises a number of challenges, such as how to integrate textual and numerical data and how to reconcile different epistemologies. A distinction can be made between mixed- method design (eg, quantitative and qualitative data are gathered and findings combined within a single or series of studies) and mixed- model study, a pragmatist approach, whereby aspects of qualitative and quantitative research are combined at different stages during a research process. 19 Qualitative research is still often viewed as only a support function or as secondary to quantitative research; however, this situation is likely to evolve as more researchers gain a broader skill set.
Though it is undeniable that there has been a marked increase in the volume and quality of qualitative research published within the past two decades, mental health research has been surprisingly slow to develop, compared to other disciplines e.g. general practice and nursing, with relatively fewer qualitative research findings reaching mainstream psychiatric journals. 2 This does not appear to reflect overall editorial policy; however, it may be partly due to the lack of confidence on the part of editors and reviewers while identifying rigorous qualitative research data for further publication. 20 However, the skilled researcher should no longer find him or herself forced into a position of defending a single-methodology camp (quantitative vs qualitative), but should be equipped with the necessary methodological and analytical skills to study and interpret data and to appraise and interpret others' findings from a full range of methodological techniques.
- Crawford MJ ,
- Cordingley L
- Dowrick C ,
- Edwards S ,
- ↵ MRC Developing and Evaluating Complex Interventions 2008
- Nelson ML ,
- Quintana SM
- Schulze B ,
- Angermeyer MC
- Mavaddat N ,
- Lester HE ,
- Donovan J ,
- Morriss R ,
- Barkham M ,
- Stiles WB ,
- Connell J ,
- Chew-Graham C ,
- England E ,
- Kinderman P ,
- Tashakkoria A ,
- Ritchie J ,
- Ssebunnya J ,
- Chilvers R ,
- Glasman D ,
- Finlay WM ,
- Strauss A ,
- Hodges BD ,
- Dobransky K
- Dixon-Woods M ,
- Fitzpatrick R ,
- Espíndola CR ,
Read the full text or download the PDF:
- Open access
- Published: 26 July 2021
A qualitative study about the mental health and wellbeing of older adults in the UK during the COVID-19 pandemic
- A. R. McKinlay 1 ,
- D. Fancourt 1 &
- A. Burton 1
BMC Geriatrics volume 21 , Article number: 439 ( 2021 ) Cite this article
54k Accesses
51 Citations
8 Altmetric
Metrics details
The objective of this study was to examine factors that threatened and protected the wellbeing of older adults living in the UK during social distancing restrictions due to the COVID-19 pandemic.
Semi-structured telephone or video interviews with 20 adults aged over 70. Purposive sampling methods were used to increase diversity within the group. Transcripts were analysed using reflexive thematic analysis.
Participants described potential threats to their wellbeing during the pandemic, including fears for mortality, grieving normal life, and concerns for the future. Participants also described activities and behaviours that helped to protect their mental health, including adopting a slower pace of life, maintaining routine, socialising, and using past coping skills. Many participants drew on their resilience and life experience to self-manage fear and uncertainty associated with the pandemic, using their time during lockdown to reflect or organise end-of-life affairs.
This study provides UK-based evidence that while some older adults experienced challenges during the first wave of COVID-19, many were resilient throughout social distancing restrictions despite early reported concerns of mental health consequences among the older adult population. Our findings highlight the importance of maintaining access to essentials to promote feelings of normality and use of social support to help reduce uncertainty in times of pandemics.
Peer Review reports
Introduction
Existing concerns about the wellbeing of older adults were exacerbated when severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was declared a pandemic by the World Health Organisation on March 11th, 2020 [ 39 ]. Older adults were identified as especially vulnerable to the virus with high rates of fatalities [ 17 ], particularly in some residential care homes [ 9 , 35 ] during the first wave of the virus [ 23 ]. Hospitalisation rates were high among those living with long term conditions (LTCs) [ 10 , 17 ], many of which affect the older adult population [ 12 , 30 ]. The UK government imposed their first social distancing restrictions on March 23rd, 2020, where adults over the age of 70 were required to self-isolate and “lockdown” at home for 3 months to reduce their infection risk.
Drawing on evidence of negative psychological responses observed during previous epidemics [ 5 ], concerns rose among stakeholders at the start of the pandemic that there would be adverse effects of the COVID-19 pandemic on mental health and wellbeing. Whilst under usual circumstances, older adults do tend to experience psychosocial wellbeing that is equal or better than that of younger age groups [ 11 ], it was predicted that due to the specific isolation rules for older adults and their heightened risk from the virus, psychosocial consequences such as loneliness would be exacerbated in older age groups [ 21 ], leading to negative effects on mental and physical health [ 22 , 34 ]. At a population level, mental health during the COVID-19 pandemic was negatively impacted [ 42 ], but evidence suggests older adults on average experienced more stable and less negative outcomes compared with other subgroups [ 20 , 38 ]. It is presently unclear why this was, or what underlying factors accounted for the experiences reported by older adults during lockdown.
Several theories could help to explain the apparent psychological resilience of older adults during the pandemic. Offers of support from social contacts [ 25 ], a stable living environment [ 6 , 7 ], cohabiting with others [ 19 ], and financial security [ 20 ] may have helped protect many in this group against adverse effects of social distancing measures by providing a psychological buffer against distress. Additionally, older adults may draw on previous life experiences to perceive a greater sense of coherence in the events of the pandemic. Sense of coherence theory incorporates comprehensibility (ability to understand and integrate), manageability (ability to navigate and manage) and meaningfulness (sense making) in relation to interpretation of a new health threat [ 1 ]. It has been shown to support better navigation of life stressors [ 1 ] and is a strong predictor of health status among older adults [ 16 ]. Life wisdom accumulated by older age has also been found to increase the use of problem-focused coping skills, which may protect against distress [ 14 ]. However, whether factors such as these do indeed explain the responses amongst older adults remains unexplored.
Understanding the factors that are transferable across age groups is essential in developing future interventions and policy for those most at risk of harm due to social distancing measures during the pandemic. Further, whilst the average mental health symptom scores and wellbeing levels of older adults have been better than amongst younger age groups during the first wave of the pandemic in the UK [ 15 ], this does not necessarily imply that older adults were psychologically unaffected. Therefore, this study explored in detail the experiences of older adults living in the UK, with two specific research questions: (1) How was the mental health of older adults affected during the pandemic? (2) What factors have protected mental health in older adults during this time?
Study design
This research was undertaken as part of the COVID-19 Social Study (CSS) that began on March 21st 2020 [ 6 , 7 ], which is the largest UK panel survey study on social life during the COVID-19 pandemic. The overall aims of this work are to explore the psychosocial impact of the pandemic among people living in the UK. In this qualitative substudy, conducted separately from the CSS survey, we elicited perspectives of older adults through qualitative interviews, which were carried out from May until September in 2020. We deployed phenomenological methodology to interrogate the data and focus on individual accounts of experience, coupled with reflexive thematic analysis techniques for analysing and framing the research data. The University College London Ethics Committee reviewed and approved this study (Project ID: 14895/005). Content in the following sections are informed by the COREQ reporting guidelines [ 37 ].
Recruitment
Eligibility criteria included: aged 70 years or older, and the ability to speak English sufficiently to understand the study participant information sheet and consent form. We recruited participants by listing the substudy in the CSS newsletter (reaching 3919 subscribers), social media, and through two community organisations who circulated study information within their networks. We did not record response rates during recruitment. People interested in participating were asked to contact the research team directly via email. In order to understand a range of individual experiences, we screened for characteristics (such as gender, ethnicity, educational level) based on previous findings highlighting how some demographics factors have been associated with adverse mental health during the pandemic [ 15 ]. Thus, we used purposive sampling methods to ensure that 20 adults aged over 70 were selected from diverse backgrounds in terms of gender, ethnicity, marital status, and living situation. Recruitment ended after 20 one-off interviews, as the lead author AM identified no new themes during the analysis.
A researcher (AM or AB) responded to expressions of interest in the study with further details about the study and an invitation to ask additional questions. All participants then provided written informed consent prior to attending a remote interview by telephone or video call. Participants were offered a £10 shopping voucher as an expression of gratitude. A team of female, postgraduate-level, qualitative healthcare researchers conducted all interviews (AM, AB, LB, AR, SC). No researcher had prior relations with any research participant. Interview times ranged from 16 to 85 min and lasted for 50 min on average. A complete interview guide can be found in Supplementary File 1 . In brief, interview topics included: normal life before the pandemic, understanding of social distancing guidelines, social life, mental health, and prospection (for question examples, refer Table 1 ). Interview guide questions and prompts were developed based on concepts from social integration and health theory [ 2 ] and Antonovsky’s Sense of Coherence theory [ 13 ]. For example, “Has the pandemic meant that you have any worries for the future? How are these different from the worries you had before?” Although all general topics were discussed during interviews, not all questions or prompts were used or indeed relevant to each participant’s unique circumstances. Interviewers were guided about the questions and prompts to use according to participant responses.
Data analysis
Researchers audio recorded the interviews with consent from participants, which were then transcribed verbatim by a professional transcription service. All transcripts were manually checked for anonymity after transcription before importing into Nvivo version 12 for analysis. Transcripts were not returned to participants for comment or correction, nor did they provide feedback on the findings. For consistency of coding approach, AM and AB double coded 3 transcripts at the start of data analysis and discussed issues of salience raised by participants. We did not calculate the intercoder reliability or quantify agreement during this stage [ 29 ], but rather focused on the impressions that both researchers had on topics of importance when coding the same passage of text. The lead researcher (AM) used an inductive and deductive, reflexive thematic analysis approach, informed by Braun and Clarke [ 3 , 4 ]. An initial coding framework was established from the topic guide, which was formulated based on supporting theory regarding social network structure, social ties, social support (i.e., [ 1 , 2 ]). This framework was applied to each transcript through line-by-line coding, then the framework was updated with new codes as AM identified new concepts in the transcripts described by participants. Themes and subthemes were therefore developed based on participant narratives, and these were presented to the CSS research team on 3 occasions throughout the analysis stages for formative feedback.
Of those who agreed to take part, 9 participants were women and 11 men, with an average age of 79 (Table 2 ). Fourteen participants reported having a physical health condition, including hypertension, diabetes, arthritis, high blood pressure and cancer. Two participants had an anxiety-related mental health condition diagnosed prior to the pandemic, and 3 said they had caregiving responsibilities for a spouse or family member.
Participants reported varied and nuanced experiences from the outset of the COVID-19 pandemic. We therefore generated two overarching themes, each with 4 subthemes. Many participants described potential threats to their wellbeing, including fears for mortality, grieving normal life, restricted access to support, and concerns for the future. However, many spoke of how they protected mental health in response to pandemic-related uncertainty, including adopting a slower pace of life, maintaining routine, socialising, and using past coping skills.
Potential threats to wellbeing
Some participants described a transient period of uncertainty at the start of the first UK lockdown, associated with nervousness and lack of sleep that resolved quickly. Many were understandably concerned about the impact the pandemic was having on their end-of-life experience and consequences for the rest of the world (Table 3 ). Overall, the government restrictions were described as “fair enough” and “required” by many; however, a commonly reported concern among participants was a fear of needing healthcare assistance during the COVID-19 lockdown. Some participants were worried about catching COVID-19 and additional risks due to their age, ethnicity, and medical history. Others said that lockdown measures meant they were unable to engage in activities that usually formed part of their self-care routine.
Concerns about end-of-life, ageing, and mortality
More than half of the group spoke about how the pandemic caused them to think about their experience of end-of-life, ageing, and mortality.
‘It’s just this idea of all of a sudden realising that I’m getting really old. I think that may be the biggest thing, and it’s a combination of getting really old, and the pandemic is probably accentuating it a bit.’ p10, female, aged 75-79
Those who were retired were particularly worried about the physical or cognitive impact of lockdown on their experience of ageing.
‘I thought I’m going to be forced into being isolated at home. Can’t go to the gym, can’t go out walking, I’m going to physically deteriorate. And I really was quite scared about that.’ p1, male, aged 80-84
Some planned for the possibility of becoming unwell from COVID. For instance, one participant had instructed his family to “stay away” should he become gravely ill, to protect them from the virus. For several participants, a reminder of their own mortality risk came from knowing someone who had passed away from COVID:
‘We’ve had one friend who was in his sixties… Suddenly went into hospital went on a respirator and sadly he died. He’s the only person we know who has directly been affected by it. It hits you and it makes you realise your own mortality. Especially when they keep saying it affects older people worse, so you do worry.’ p13, male, aged 75-79
Several participants described concerns about their perceived vulnerability to COVID due to their age, ethnic group, or pre-existing health concerns:
‘It is scary for us at our age. The thought of getting COVID, that really frightens me and frightens me for anybody close to me that if they got it. It really terrifies me. So, we have been very, very careful.’ p11, female, aged 70-74
Grieving the loss of normality
Understandable emotional responses and a longing for normality were frequently described by participants. Some felt the activities they previously enjoyed, like travelling, going to the theatre, or “hitting a tennis ball,” would never return to the normal they were used to. Others said they felt their life was on hold until the virus was under control or a vaccine was introduced.
‘The new normal is not going to be at all like the old normal, I don't think. We won’t really be able to live the kind of life that we lived before until there’s a vaccine, and it looks as though the vaccine is going to be a very long way off.’ p4, female, aged 70-74
Some said they felt grief about the impact COVID was having on the world, particularly regarding death, hardships, and suffering of others.
‘I knew of the wars and the disease and the hunger, but I think COVID has just put a whole blanket round the lot of it and makes it so immense, the state of the world. The horrible state of the world and that is very depressing when you think about it.’ p19, female, aged 80-84
Several said they did not think a COVID vaccine would help life “go back to where we were before.”
‘Whatever happens, even if a vaccine comes, we will never return to shaking strangers’ hands.’ p16, male, aged 75-79
Healthcare concerns
Concerns about catching COVID were variable among the group, but many were more fearful of being hospitalised for any reason because they believed they were at increased risk of death.
‘A lot of people are scared stiff of catching [COVID], I’m not. The only thing I’m scared of is being carted off to a hospital. I want to die peacefully at home, and I would happily do that any night.’ p8, male, aged 90-94
Those living alone in particular worried about the lack of available health services during lockdown, should anything “go wrong” with their health independently from COVID.
‘A friend of mine has just been diagnosed with breast cancer. She’s had to wait about nine weeks for her op… so you worry about if something like that happened to me, would I get the medical attention I need?’ p12, female, aged 75-79
The potential health threat of COVID meant some participants were scared to leave the house.
‘I do feel that perhaps I should be going out more and that sort of thing, but myself and many, many, almost all my friends say that they are very scared to go out.’ p2, female, 70-74
Several participants had decided to self-isolate before the national restrictions were introduced, mainly due to concerns about age-related vulnerability and pre-existing health conditions.
‘Come mid-March when it all happened… we decided ourselves to lockdown before other people did… I’m over 75 and I’ve got blood pressure controlled by medication but I’m over 75. My BMI was over 30… So, I was worried and we were worried. So, we totally shut down.’ p16, male, aged 75-79
Unable to engage with activities that protect wellbeing
Due to social distancing and travel restrictions, some participants were unable to engage in activities such as weekly religious ceremonies, theatre groups, and sports. Although some activities were able to be undertaken online, this was not always possible.
‘Since COVID, [community activities have] all closed down. Well yes, the book club totally because we can’t discuss books over the phone and also people are of an age where you can’t do social media, whatever you call it.’ p19, female, aged 80-84
Several participants commented on the consequences of an abrupt change in routine on their wellbeing during lockdown.
‘That was the first thing that hit me, boredom. I had no idea what the hell am I going to do next, because I was used to a routine and suddenly the routine was completely disrupted…Now suddenly I had nothing to do and I was really lost. I was walking round the house like a bloody zombie trying to find something to do.’ p15, male, aged 80-84
Protective activities and Behaviours
Despite voicing threats to wellbeing, many participants were positive in reflecting on their lockdown experience. This was attributed to a slowed pace of life, maintaining a routine, using coping skills and resources, and accessing social support (Table 3 ).
Slowing the pace of life
The most commonly reported experience during lockdown was feeling like the pace of life had slowed on an individual and societal level, with more time alone to reflect. Although some participants had described a loss of leisure during lockdown, many had found time for new hobbies, reading, crafts, gardening, and learning a new language.
“Sometimes I wake up in the morning, and I think, oh, it’s another day in lockdown, but I think… there are some little positive benefits…Before lockdown, we were all rushing around doing lots of things, and now we’ve had to slow down. And actually, slowing down has been quite nice. And we’re living in the kind of retirement now that, maybe, our grandparents might have lived, when you just cultivate your garden and do your knitting and crochet... But just generally living a slower pace of life.“ p4, female, aged 70-74
Others felt that being required to stay at home presented an opportunity to focus more on their health by going for regular walks and taking up new forms of physical activity. For some, this was the first time in decades they had been so physically active.
“I’ve now started to ride a proper bike as well. I live in a Close, so we don’t get any through traffic and I can cycle around that Close and I do a few laps. But I haven’t ridden a bike for 60 years.” p1, male, aged 80–84
Half of the group said the slowed pace of life gave more time for introspection: “I’m not rushing around so much anymore, it’s given me the time and the opportunity to notice small things.” p4, female, aged 70–74. In particular, many women in the group said they reflected on their life differently and in a more meaningful or positive way than before. Some used this process of reflection to think about the changes they would make to their lives as a result of their pandemic experience.
‘Having grown quite a lot, I feel quite positive about that. I also think I’m going to try and, maybe, achieve more things when I come out of this [lockdown]. I think when you retire, and as you get older, you become very comfortable in your life. I think, perhaps, I was a bit too comfortable. I need to get out and be more proactive.’ p6, female, aged 70-74
Benefits of routine and social responsibility
Nearly half of participants said that maintaining a routine and sense of purpose was important for their wellbeing during the COVID-19 lockdown: “ You have to have a purpose you see. I think mental resilience is all about having a sense of purpose.” (p15, male, aged 80–84).
Many female participants said they experienced meaningful benefits from social responsibilities, such as cooking a meal for family, phoning friends to check in, or caring for a pet:
‘The important thing is to have the necessity to do things. Whether it is to get in touch with people, to write a piece of something… Obligations are a good source of maintaining ones feeling of self-worth, if you like. So I think it’s very important to make sure that whatever it is, even though you may feel oh what a nuisance I’ve got to do that, the very fact of having to do it is a great psychological benefit.’ p3, female, aged 70-74
Social interactions and support
The nature of socialising had changed since the start of lockdown for many but not all participants. Several said they were socialising to try to carry on “life as normal” , particularly keeping in regular contact with family. For some, this resulted in strengthened relationship bonds and connectedness:
‘I think it has made me and my husband stronger really. We’ve never spent as much time together actually… I think we’ve coped with the shopping and organising that. And we’ve been baking together, we’ve never done things like that. And we took it in turns to cook and tidy up after. We have done really well together. I’m really proud of us.’ p11, female, aged 70-74
Utilising skills, experience and accessing practical resources to cope
Participants who had used mental health services in the past spoke of utilising the skills they had previously learned to help cope with the COVID-19 crisis, including use of mindfulness and meditation.
‘I had a wonderful counsellor who I saw about once a year, and she would set me on the right path. And eventually, after many years of trying, I found a mindfulness and meditation book, about the middle of last year… so I feel that that has been a great help to me. Usually I try in the morning and certainly in the evening, before I go to bed, I do some meditation.’ p2, female, 70-74
Others described experiences of hardship in the past that they used as a comparison with COVID times, such as living through war, displacement, and illness:
‘I was diagnosed with what they call non-invasive bladder cancer… Having gone through the concern of something like that, perhaps Covid, you know, you put it into perspective.’ P13, male, aged 75-79
For some who lived alone, they spoke of being accustomed to isolation long before the pandemic arrived: “I’m a fairly sort of isolated person anyway.” p1, male, aged 80–84 . Several said they were accustomed to being alone due to widowhood or retirement, and therefore lockdown did not prompt a dramatic change in their daily living or social life:
‘I’ve been retired for a nice long time… So, in many ways the lockdown, on one side it hasn’t impacted a great deal, because I was used to being at home and certainly over the past two years to being home alone.’ p20, male, aged 80-84
Participants frequently mentioned their access to practical resources and basic necessities that helped reduce uncertainty, such as access to online shopping for home food deliveries and offers from others to drop off medication. Such arrangements had been made during lockdown, with additional support offered by family, friends, and neighbours.
‘I’ve had online shopping every week since lockdown and I haven’t been to any shop. Prescriptions were delivered and anything I wanted, my daughter would fetch.’ p18, female, aged 80-84
In this study, we sought the views of older adults living in the UK about factors that threatened or protected their mental health and wellbeing during the COVID-19 pandemic. Our study identified understandable emotional responses to the pandemic including fears relating to the virus, the future, and mortality. These are justified in the face of unprecedented circumstances, such as those brought about by COVID-19 [ 28 ]. Overall, older adults mostly described engaging with activities and behaviours that helped to protect their mental health and could explain their improved wellbeing relative to other age-groups. For the most part, participants enjoyed feeling less social pressure and having more time for their hobbies. Similarities in experience were drawn by this group between a slower pace of life germane to retirement and day-to-day realities of the COVID-19 lockdown. As described by older adults in Japan [ 36 ], COVID-19 restrictions introduced comparatively few changes to daily life compared with other groups. Those who experienced greater daily changes and uncertainty, such as parents of young children, working age adults and those affected by financial difficulties, have reported greater levels emotional distress during the pandemic [ 32 ]. Fewer changes and transitions experienced by older adults may therefore explain some of the differences observed in levels of psychological distress.
Congruent with international research [ 25 ], many participants began to self-isolate earlier than guidance required and perhaps consequently, practical arrangements were in place for access to essentials from the outset of lockdown (for instance, food and medication deliveries offered to people aged over 70), resulting in greater sense of coherence of COVID-19 as a potential health threat. Being at home early meant less opportunities for virus exposure, perhaps reducing fear of virus transmission and creating an environment of stable predictability (comprehensibility). Many older adults were offered online shopping slots or received offers of help from friends, family or neighbours for medication collection, meaning access to supplies was not restricted (manageability). And for the most part, older adults in our study made sense of the pandemic with reference to previous major events in their lives, such as war and displacement. Explanations about their behaviours and adherence during this time was described as behaviour “for the greater good” for the rest of society (meaningfulness).
Factors that threatened mental health and wellbeing during COVID-19
Given early evidence publicised on mortality risk for older adults [ 41 ], it is unsurprising participants frequently discussed concerns about their end-of-life. Studies have shown an association between social isolation and reduced physical performance, [ 31 ] causing concern among some participants in our study, with many taking extra steps to preserve their activity levels. While this may have provided positive health benefits in the short term, of most concern is the fear many participants described in leaving the house to access routine or preventative health care, which may have longer-term implications for public health services. Aligned with international research [ 24 ], participants in our study also worried about the impact of COVID-19 on the world and spoke of the impact this had for their wellbeing on a daily basis. Feelings of grief and loss were frequently reported and will likely be felt across many societies in response to the pandemic.
Factors that protected mental health and wellbeing during COVID-19
Quantitative data collected during the first UK lockdown suggests that those with restricted finances and access to basic needs experienced higher levels of adversity during the first wave of the pandemic [ 40 ]. Many participants in our study reported having access to basic supplies (via online shopping slots and medication deliveries) and high levels of perceived social support, which may have helped to create a buffer against stress and uncertainty. National averages showed infrequent experiences of loneliness among older adults during the pandemic [ 26 ], which may be explained by our finding that participants engaged frequently in online methods of interaction, spent time with pets, and/or had regular remote “check-ins” with friends and family to mitigate against loneliness. As such, the heightened concern about loneliness in this age group early on in the pandemic may have led older adults and those around them to proactively take steps that helped prevent these experiences in many individuals. Indeed, many participants reported enhanced feelings of connectedness with social contacts throughout the lockdown, which can prevent isolation and protect against emotional distress [ 34 ]. However, a small number of participants did not feel connected, particularly those who had been separated from their family because of the pandemic, highlighting the difficulties experienced when such support was not available.
Implications
This study highlights a number of important implications. First, the potential threats to wellbeing amongst older adults require further consideration as they have implications for the immediate future and for future pandemics. In trying to remove barriers to healthcare access, supporting older adults in engaging with telecare may be a helpful alternative for some health concerns. However, in our CSS work involving people with mental health conditions in the UK, we found service users felt this was an unhelpful substitute [ 8 , 9 ]. Future research must address indirect health consequences of the pandemic resultant of delayed or diminished access to healthcare during the lockdown. Second, as discussed elsewhere [ 18 ], interventions to mitigate the impact of prolonged isolation on experiences of grief are warranted. Grief can prompt search for meaning and seeking out others with similar experiences. Clinicians play a role in supporting people in processing their grief associated with COVID-19, but spaces online and within groups may also facilitate healing from loss experienced during the pandemic [ 18 ]. Schemes such as social prescribing could be deployed to support older adults psychosocially, and may provide additional support in the aftermath of COVID-19 [ 33 ]. Finally, it is evident that forward-planning by families and communities to address initial concerns about older adults during the pandemic played an important role in supporting their coping and buffering against loneliness, isolation, and uncertainty. For future pandemics, such a response is again encouraged. In particular, interventions that bolster feelings of certainty and connectedness may serve as helpful targets for those experiencing pandemic-related distress.
Strengths and limitations
A strength of this research is that data were collected from participants via purposive recruitment throughout the first UK lockdown and as restrictions began to ease before the second wave. However, findings must be interpreted cautiously. Our participants were generally healthy, with well-established social networks, living in the community, and predominantly without solo caregiving responsibilities. Therefore, their experiences are not likely to be representative of those living with serious health concerns, who may be more likely to have experienced distress during the pandemic [ 27 ]. We conducted interviews via video call or telephone, which meant being able to capture experiences safely amid restrictions, but also means that those without access to the internet or telephone would not have had equitable access to participate and may have faced additional challenges. We also did not collect data on, or sample based on socioeconomic status or previous COVID-19 infection. To our knowledge, no participant had experienced a confirmed diagnosis. Future studies are needed to ascertain how older adults who experienced COVID-19 were impacted psychologically [ 26 ].
Conclusions
Contrary to early concerns at the start of the pandemic, the mental health of older adults fared well compared with other age groups, and this study adds to the literature on this topic by providing evidence as to why these results may have been found. Overall, many participants described their experience of lockdown as a time for reduced social pressures and increased opportunities for personal growth. However, this group experienced challenges, particularly among those who were concerned about staying well, advancing frailty, or hospitalisation risk. This research therefore highlights the importance of nuance when considering the relative better experiences of older adults. It also provides valuable insight into factors that protected wellbeing of older adults during the COVID-19 pandemic, which may be utilised by policy makers to support at-risk groups who have experienced psychological hardship during the crisis, including timely access to essential supplies, communicating offers of help to improve perceived support, and providing structure and routine in times of uncertainty.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available and are not available from the corresponding author on request due to reasons concerning participant privacy and confidentiality.
Antonovsky A. Health, Stress, and Coping. San Francisco: Jossey-Bass Inc; 1979.
Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51(6):843–57.
Article CAS PubMed Google Scholar
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exercise Health. 2019;11(4):589–97. https://doi.org/10.1080/2159676X.2019.1628806 .
Article Google Scholar
Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis?. Qual Res Psychol. 2020:1–25. https://doi.org/10.1080/14780887.2020.1769238 .
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. https://doi.org/10.1016/S0140-6736(20)30460-8 .
Article CAS PubMed PubMed Central Google Scholar
Bu F, Steptoe A, Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med. 2020a;265:113521. https://doi.org/10.1016/j.socscimed.2020.113521 .
Article PubMed PubMed Central Google Scholar
Bu F, Steptoe A, Mak HW, Fancourt D. Time-use and mental health during the COVID-19 pandemic: A panel analysis of 55,204 adults followed across 11 weeks of lockdown in the UK: Medrxiv: The Preprint Server for Health Sciences; 2020b. https://doi.org/10.1101/2020.08.18.20177345 .
Burton A, McKinlay AR, Aughterson H, Fancourt D. Impact of the Covid-19 pandemic on the mental health and wellbeing of adults with mental health conditions in the UK: A qualitative interview study: Medrxiv: The Preprint Server for Health Sciences; 2020a. https://doi.org/10.1101/2020.12.01.20241067 .
Burton JK, Bayne G, Evans C, Garbe F, Gorman D, Honhold N, et al. Evolution and effects of COVID-19 outbreaks in care homes: A population analysis in 189 care homes in one geographical region of the UK. Lancet Healthy Longevity. 2020b;1(1):e21–31. https://doi.org/10.1016/S2666-7568(20)30012-X .
Article PubMed Google Scholar
CDC COVID-19 Response Team, CDC COVID-19 Response Team, Bialek S, Boundy E, Bowen V, Chow N, Cohn A, et al. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–6. https://doi.org/10.15585/mmwr.mm6912e2 .
Charles ST, Carstensen LL. Social and emotional aging. Annu Rev Psychol. 2010;61(1):383–409. https://doi.org/10.1146/annurev.psych.093008.100448 .
Denton FT, Spencer BG. Chronic health conditions: changing prevalence in an aging population and some implications for the delivery of health care services. Can J Aging. 2010;29(1):11–21. https://doi.org/10.1017/S0714980809990390 .
Eriksson M, Lindstrom B. Antonovsky’s sense of coherence scale and its relation with quality of life: A systematic review. J Epidemiol Community Health. 2007;61(11):938–44. https://doi.org/10.1136/jech.2006.056028 .
Etezadi S, Pushkar D. Why are wise people happier? An explanatory model of wisdom and emotional well-being in older adults. J Happiness Stud. 2013;14(3):929–50. https://doi.org/10.1007/s10902-012-9362-2 .
Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry. 2020;8(2):141–9. https://doi.org/10.1016/S2215-0366(20)30482-X .
Forbes DA. Enhancing mastery and sense of coherence: important determinants of health in older adults. Geriatr Nurs. 2001;22(1):29–32. https://doi.org/10.1067/mgn.2001.113532 .
Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–64. https://doi.org/10.15585/mmwr.mm6915e3 .
Goveas JS, Shear MK. Grief and the COVID-19 pandemic in older adults. Am J Geriatr Psychiatry. 2020;28(10):1119–25. https://doi.org/10.1016/j.jagp.2020.06.021 .
Groarke JM, Berry E, Graham-Wisener L, McKenna-Plumley PE, McGlinchey E, Armour C. Loneliness in the UK during the COVID-19 pandemic: cross-sectional results from the COVID-19 psychological wellbeing study. PLoS One. 2020;15(9):e0239698. https://doi.org/10.1371/journal.pone.0239698 .
Holingue C, Badillo-Goicoechea E, Riehm KE, Veldhuis CB, Thrul J, Johnson RM, et al. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: findings from American trend panel survey. Prev Med. 2020;139:106231. https://doi.org/10.1016/j.ypmed.2020.106231 .
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60. https://doi.org/10.1016/S2215-0366(20)30168-1 .
Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspect Psychol Sci. 2015;10(2):227–37. https://doi.org/10.1177/1745691614568352 .
Ioannidis JPA, Axfors C, Contopoulos-Ioannidis DG. Second versus first wave of COVID-19 deaths: shifts in age distribution and in nursing home fatalities: Medrxiv: The Preprint Server for Health Sciences; 2020. https://doi.org/10.1101/2020.11.28.20240366 .
Kivi M, Hansson I, Bjälkebring P. Up and about: older adults’ well-being during the COVID-19 pandemic in a Swedish longitudinal study. J Gerontol B Psychol Sci Soc Sci. 2020;76(2):e4–9. https://doi.org/10.1093/geronb/gbaa084 .
Article PubMed Central Google Scholar
Krendl AC, Perry BL. The impact of sheltering-in-place during the COVID-19 pandemic on older adults’ social and mental well-being. J Gerontol B Psychol Sci Soc Sci. 2020. https://doi.org/10.1093/geronb/gbaa110 .
Li LZ, Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291:113267. https://doi.org/10.1016/j.psychres.2020.113267 .
Lima CK, de Medeiros Carvalho PM, Lima ID, de Oliveira Nunes JV, Saraiva JS, de Souza RI, et al. The emotional impact of coronavirus 2019-nCoV (new coronavirus disease). Psychiatry Res. 2020;287:112915. https://doi.org/10.1016/j.psychres.2020.112915 .
Morgan C, Rose N. Multidisciplinary research priorities for the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):e33. https://doi.org/10.1016/S2215-0366(20)30230-3 .
O’Connor C, Joffe H. Intercoder reliability in qualitative research: debates and practical guidelines. Int J Qual Methods. 2020;19:160940691989922. https://doi.org/10.1177/1609406919899220 .
Office for National Statistics. (2020). People with long-term health conditions, UK: January to December 2019. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/adhocs/11478peoplewithlongtermhealthconditionsukjanuarytodecember2019
Google Scholar
Philip KEJ, Polkey MI, Hopkinson NS, Steptoe A, Fancourt D. Social isolation, loneliness and physical performance in older-adults: fixed effects analyses of a cohort study. Sci Rep. 2020;10(1):13908. https://doi.org/10.1038/s41598-020-70483-3 .
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–92. https://doi.org/10.1016/S2215-0366(20)30308-4 .
Razai MS, Oakeshott P, Kankam H, Galea S, Stokes-Lampard H. Mitigating the psychological effects of social isolation during the covid-19 pandemic. BMJ. 2020:m1904. https://doi.org/10.1136/bmj.m1904 .
Santini ZI, Jose PE, York Cornwell E, Koyanagi A, Nielsen L, Hinrichsen C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health. 2020;5(1):e62–70. https://doi.org/10.1016/S2468-2667(19)30230-0 .
Strang P, Fürst P, Schultz T. Excess deaths from COVID-19 correlate with age and socio-economic status. A database study in the Stockholm region. Ups J Med Sci. 2020;125(4):297–304. https://doi.org/10.1080/03009734.2020.1828513 .
Takashima R, Onishi R, Saeki K, Hirano M. Perception of COVID-19 restrictions on daily life among Japanese older adults: A qualitative focus group study. Healthcare. 2020;8(4):450. https://doi.org/10.3390/healthcare8040450 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, de Vries DH. Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. J Gerontol B Psychol Sci Soc Sci. 2020. https://doi.org/10.1093/geronb/gbaa111 .
World Health Organisation. (2020). Coronavirus disease 2019 (COVID-19) Situation Report – 51. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10
Wright L, Steptoe A, Fancourt D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J Epidemiol Community Health. 2020:jech-2020-214475. https://doi.org/10.1136/jech-2020-214475 .
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. https://doi.org/10.1001/jama.2020.2648 .
Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55–64. https://doi.org/10.1016/j.jad.2020.08.001 .
Download references
Acknowledgements
The researchers are grateful for the support of AgeUK, the Alzheimer’s Society and Healthwise Wales during recruitment. Many thanks to Anna Roberts, Louise Baxter Sara Esser and Rana Conway for their help with conducting interviews. Thank you to the COVID-19 Social Study Team (Tom May, Katey Warren, Joanna Dawes, and Henry Aughterson) who provided feedback on the themes and subthemes. We wish to thank the anonymous reviewers for their constructive suggestions that helped us to refine this manuscript.
This work was supported by the Nuffield Foundation [WEL/FR-000022583], but the views expressed are those of the authors and not necessarily the Foundation. The study was also supported by the MARCH Mental Health Network funded by the Cross-Disciplinary Mental Health Network Plus initiative supported by UK Research and Innovation [ES/S002588/1], and by the Wellcome Trust [221400/Z/20/Z]. DF was funded by the Wellcome Trust [205407/Z/16/Z].
Author information
Authors and affiliations.
Research Department of Behavioural Science and Health, Institute of Epidemiology & Health Care, University College London, 1-19 Torrington Place, London, WC1E 7HB, UK
A. R. McKinlay, D. Fancourt & A. Burton
You can also search for this author in PubMed Google Scholar
Contributions
DF and AB were involved with study design. AM collected study data and led the analysis and interpretation of study findings, with support from AB. AM wrote the first paper draft. DF and AB provided critical revisions. All authors have read and approve the final version of the manuscript.
Corresponding author
Correspondence to A. R. McKinlay .
Ethics declarations
Ethics approval and consent to participate.
The University College London Ethics Committee reviewed and approved this study (Project ID: 14895/005). After receipt of a Participant Information Sheet and opportunity to ask questions, all participants then provided written informed consent to participate. We confirm that all methods were carried out in accordance with relevant guidelines and regulations under ethics approval, including participants’ informed consent to participate.
Consent for publication
All participants provided written informed consent for study publication.
Competing interests
None declared.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview topic guide: Adult groups.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
McKinlay, A.R., Fancourt, D. & Burton, A. A qualitative study about the mental health and wellbeing of older adults in the UK during the COVID-19 pandemic. BMC Geriatr 21 , 439 (2021). https://doi.org/10.1186/s12877-021-02367-8
Download citation
Received : 14 January 2021
Accepted : 29 June 2021
Published : 26 July 2021
DOI : https://doi.org/10.1186/s12877-021-02367-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Older adults
- Mental health
- Social support
BMC Geriatrics
ISSN: 1471-2318
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Advertisement
Barriers to Accessing Mental Health Care Under the Mental Health Services Act: A Qualitative Case Study in Orange County, California
- Original Paper
- Published: 19 September 2022
- Volume 59 , pages 381–390, ( 2023 )
Cite this article
- Elizabeth Siantz ORCID: orcid.org/0000-0001-8305-3818 1 ,
- Sarah Hiller 2 ,
- Victoria D. Ojeda 2 &
- Todd P. Gilmer 2
1287 Accesses
8 Altmetric
Explore all metrics
Despite progress made under California’s Mental Health Services Act, limited access to care for cultural and linguistic minority groups remains a serious issue in community mental health. In this qualitative study we report findings from a large-scale community-level assessment that explored barriers to accessing care from the perspectives of multiple stakeholders including county advisors, advocates, community members, and consumers representing a range of cultural and linguistic communities in Orange County, California. We conducted 14 focus groups with N = 112 participants. Qualitative analysis revealed that system fragmentation, limited availability of linguistically appropriate care, and stigma continue to undermine access to mental health care. Peer health navigation and culturally responsive peer support are potential ways to promote service engagement with persons from cultural and linguistic minority groups that encounter barriers when accessing mental health services.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Community Interventions to Promote Mental Health and Social Equity
Enrico G. Castillo, Roya Ijadi-Maghsoodi, … Kenneth B. Wells

Insiders’ Insight: Discrimination against Indigenous Peoples through the Eyes of Health Care Professionals
Lloy Wylie & Stephanie McConkey

Access to health services among culturally and linguistically diverse populations in the Australian universal health care system: issues and challenges
Resham B. Khatri & Yibeltal Assefa
Amelia Seraphia, Derr (2016) Mental Health Service Use Among Immigrants in the United States: A Systematic Review. Psychiatric Services 67(3) 265-274 10.1176/appi.ps.201500004
Article Google Scholar
Alegría, M., Alvarez, K., Ishikawa, R. Z., DiMarzio, K., & McPeck, S. (2016). Removing obstacles to eliminating racial and ethnic disparities in behavioral health care. Health Affairs , 35 (6), 991–999. doi: https://doi.org/10.1377/hlthaff.2016.0029
Ashwood, K., Chamberlain, et al. (2018). Evaluation of the Mental Health Services Act in Los Angeles County: implementation and outcomes for key programs.Rand Health Quarterly,
Bombard, Y., Baker, G. R., Orlando, E., Fancott, C., Bhatia, P., Casalino, S., & Pomey, M. P. (2018). Engaging patients to improve quality of care: a systematic review. Implementation Science , 13 (1), 1–22. doi: https://doi.org/10.1186/s13012-018-0784-z
Boivin, A., Lehoux, P., Lacombe, R., Burgers, J., & Grol, R. (2014). Involving patients in setting priorities for healthcare improvement: a cluster randomized trial. Implementation Science , 9 (1), 24. doi: https://doi.org/10.1186/1748-5908-9-24
Boyatzis, R. E. (1998). Transforming qualitative information: Thematic analysis and code development. Sage Publications, Inc.
Buchmueller, T. C., & Levy, H. G. (2020). The ACA’s Impact On Racial And Ethnic Disparities In Health Insurance Coverage And Access To Care. Health Affairs , 39 (3), 395–402. doi: https://doi.org/10.1377/hlthaff.2019.01394
Cabassa, L. J., Siantz, E., Nicasio, A., Guarnaccia, P., & Lewis-Fernández, R. (2014). Contextual factors in the health of people with serious mental illness. Qualitative Health Research , 24 (8), 1126–1137. doi: https://doi.org/10.1177/1049732314541681
Cashin, C., Scheffler, R., Felton, M., et al. (2008). Transformation of the California mental health system: stakeholder-driven planning as a transformational activity. Psychiatric Services , 59 , 1107–1114. doi: https://doi.org/10.1176/ps.2008.59.10.1107
Chinman, M., George, P., Dougherty, R. H., Daniels, A. S., Ghose, S. S., Swift, A., & Delphin-Rittmon, M. E. (2014). Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatric Services, 65(4), 429-441. https://doi.org/10.1176/appi.ps.201300244
Coleman, K. J., Stewart, C., Waitzfelder, B. E., Zeber, J. E., Morales, L. S., Ahmed, A. T., & Hunkeler, E. M. (2016). Racial-ethnic differences in psychiatric diagnoses and treatment across 11 health care systems in the mental health research network. Psychiatric Services , 67 (7), 749–757. doi: https://doi.org/10.1176/appi.ps.201500217
County Funding Request for Mental Health Services Act (MHSA) Community Program Planning. Letter No. 05 – 01. Sacramento, State of California, Department of Mental Health, Jan 18, 2005. Available at: https://www.dhcs.ca.gov/formsandpubs/MHArchiveLtrs/MH-Ltrs05-01.pdf
Derr, A. S. (2016). Mental health service use among immigrants in the United States: A systematic review. Psychiatric Services. 67(3), 265–274
Felton, M. C., Cashin, C. E., & Brown, T. T. (2010). What does it take? California county funding requests for recovery-oriented full service partnerships under the Mental Health Services Act. Community Mental Health Journal , 46 (5), 441–451. Doi: https://doi.org/10.1007/s10597-010-9304-6
Gilmer, T. P., Stefancic, A., Tsemberis, S., et al. (2014). Full-service partnerships among adults with serious mental illness in California: impact on utilization and costs. Psychiatric Services , 65 , 1120–1125. https://doi.org/10.1176/appi.ps.201300380
Gilmer, T. P., Henwood, B. F., Goode, M., Sarkin, A. J., & Innes-Gomberg, D. (2016). Implementation of integrated health homes and health outcomes for persons with serious mental illness in Los Angeles County. Psychiatric Services , 67 (10), 1062–1067. doi https://doi.org/10.1176/appi.ps.201500092
Health Resources Service Administration: Retrieved from: https://data.hrsa.gov/tools/shortage-area/hpsa-find Accessed 6/23/2022
Kelly, E., Fulginiti, A., Pahwa, R., Tallen, L., Duan, L., & Brekke, J. S. (2014). A pilot test of a peer navigator intervention for improving the health of individuals with serious mental illness. Community mental health journal, 50(4), 435–446
Macdonell, K., Christie, K., Robson, K., Pytlik, K., Lee, S. K., & O’Brien, K. (2013). Implementing family-integrated care in the NICU: engaging veteran parents in program design and delivery. Advancing Neonatal Care , 13 (4), 262–269. doi: https://doi.org/10.1097/ANC.0b013e31829d8319
Manuel, J. I. (2018). Racial/ethnic and gender disparities in health care use and access. Health Services Research , 53 (3), 1407–1429. doi: https://doi.org/10.1111/1475-6773.12705
Miles, M. B., & Huberman, A. M. (1994). Qualitative Data Analysis: An Expamded Sourcebook (2nd ed.). Thousand Oaks: Sage
Google Scholar
Sunderji, N., Nicholas Angl, E., Polaha, J., & Gao, C. (2019). Why and how to use patient-oriented research to promote translational research
Ojeda, V. D., Hiller, S. P., Hurst, S., Jones, N., McMenamin, S., Burgdorf, J., & Gilmer, T. P. (2016). Implementation of Age-Specific Services for Transition-Age Youths in California. Psychiatric Services , 67 (9), 970–976. doi: https://doi.org/10.1176/appi.ps.201500084
Ojeda, V. D., Munson, M. R., Jones, N., Berliant, E., & Gilmer, T. P. (2021). The Availability of Peer Support and Disparities in Outpatient Mental Health Service Use Among Minority Youth with Serious Mental Illness. Administration and Policy in Mental Healthand Mental Health Services Research , 48 (2), 290–298. doi: https://doi.org/10.1007/s10488-020-01073-8
Park-Lee, E., Lipari, R. N., Hedden, S. L., Kroutil, L. A., & Porter, J. D. (2012). 2017 Sep. CBHSQ Data Review . Rockville (MD): Substance Abuse and Mental Health Services Administration (US). Receipt of Services for Substance Use and Mental Health Issues Among Adults: Results from the 2016 National Survey on Drug Use and Health
Siantz, E., Henwood, B., & Baezcondi-Garbanati, L. (2018). From physical wellness to cultural brokering: Unpacking the roles of peer providers in integrated health care settings. Community Mental Health Journal , 54 (8), 1127–1135. doi: https://doi.org/10.1007/s10597-018-0320-2
Starks, S. L., Arns, P. G., Padwa, H., Friedman, J. R., Marrow, J., Meldrum, M. L., & Braslow, J. T. (2017). System transformation under the California Mental Health Services Act: Implementation of full-service partnerships in LA County. Psychiatric Services , 68 (6), 587–595. doi: https://doi.org/10.1176/appi.ps.201500390
Substance Abuse and Mental Health Services Administration (2019). Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19-5068, NSDUH Series H-54). Retrieved from https://www.samhsa.gov/data/
Substance Abuse and Mental Health Services Administration, Racial. (2015). Ethnic Differences in Mental Health Service Use among Adults. HHS Publication No. SMA-15-4906 . Rockville, MD: Substance Abuse and Mental Health Services Administration
Nadiya, Sunderji Allyson, Ion Annie, Zhu Athina, Perivolaris David, Rodie Benoit H., Mulsant (2019) Challenges in conducting research on collaborative mental health care: a qualitative study. CMAJ Open 7(2) E405-E414 /cmajo/7/2/E405.atom https://doi.org/10.9778/cmajo.20180172
Palinkas, L. A., Criado, V., Fuentes, D., Shepherd, S., Milian, H., Folsom, D., & Jeste, D. V. (2007). Unmet needs for services for older adults with mental illness: comparison of views of different stakeholder groups. The American Journal of Geriatric Psychiatry , 15(6), 530-540
Patton, M. Q. (2005). Qualitative research. In Encyclopedia of statistics in behavioral science. Hoboken: Wiley.
Report to the Governer and Legislature (Dec 2013). Sacramento, CA,Mental Health Services Oversight and Accountability Commission,
Tran, L. D., & Ponce, N. A. (2017). Who gets needed mental health care? Use of mental health services among adults with mental illness in California. California Journal of Health Promotion , 15 (1), 36–45. https://doi.org/10.32398/cjhp.v15i1.1887
Villamil-Grest, C., Siantz, E., & Cederbaum, J. A. (2021). Behavioral health services use among racial and ethnic groups: Results from the California Health Interview Survey. Journal of Immigrant and Minority Health. 1-7. doi: https://doi.org/10.1007/s10903-021-01250-3
Download references
Author information
Authors and affiliations.
College of Social Work, University of Utah, Salt Lake City, UT, USA
Elizabeth Siantz
Herbert Wertheim School of Public Health and Human Longevity Sciences, University of California San Diego, La Jolla, CA, USA
Sarah Hiller, Victoria D. Ojeda & Todd P. Gilmer
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Elizabeth Siantz .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Siantz, E., Hiller, S., Ojeda, V.D. et al. Barriers to Accessing Mental Health Care Under the Mental Health Services Act: A Qualitative Case Study in Orange County, California. Community Ment Health J 59 , 381–390 (2023). https://doi.org/10.1007/s10597-022-01016-7
Download citation
Received : 09 March 2022
Accepted : 01 August 2022
Published : 19 September 2022
Issue Date : February 2023
DOI : https://doi.org/10.1007/s10597-022-01016-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health equity
- Qualitative
- Community mental health
- Cultural and linguistic diversity
- Access to mental health services
- Find a journal
- Publish with us
- Track your research
- Research article
- Open access
- Published: 05 October 2018
A qualitative study on the stigma experienced by people with mental health problems and epilepsy in the Philippines
- Chika Tanaka ORCID: orcid.org/0000-0002-6288-5532 1 ,
- Maria Teresa Reyes Tuliao 2 ,
- Eizaburo Tanaka 3 ,
- Tadashi Yamashita 4 &
- Hiroya Matsuo 1
BMC Psychiatry volume 18 , Article number: 325 ( 2018 ) Cite this article
139k Accesses
33 Citations
8 Altmetric
Metrics details
Stigma towards people with mental health problems (PMHP) is known to have substantial negative impacts on their lives. More in-depth exploration of the stigma and discrimination experienced by PMHP in low- and middle-income countries is needed. Previous research suggests that negative attitudes towards PMHP are widespread among the Filipino general public. However, no study has investigated PMHP’s own experiences of being stigmatised in the Philippines.
A qualitative study was conducted on the stigma experienced by PMHP (including people with epilepsy) and its related factors in the Philippines, employing the constructivist grounded theory approach. We analysed data on 39 PMHP collected through interviews with PMHP, their carers, and community health volunteers who know them well.
The findings highlight the culturally and socio-economically specific contexts, consequences, and impact modifiers of experiences of stigma. Participants emphasised that PMHP face stigma because of the cultural traits such as the perception of mental health problem as a disease of the family and the tendency to be overly optimistic about the severity of the mental health problem and its impact on their life. Further, stigma was experienced under conditions where mental health care was not readily available and people in the local community could not resolve the PMHP’s mental health crisis. Stigma experiences reduced social networks and opportunities for PMHP, threatened the economic survival of their entire family, and exacerbated their mental health problems. An individual’s reaction to negative experiences can be fatalistic in nature (e.g. believing in it is God’s will). This fatalism can help PMHP to remain hopeful. In addition, traditional communal unity alleviated some of the social exclusion associated with stigma.
Conclusions
The study indicates that existing stigma-reduction strategies might have limitations in their effectiveness across cultural settings. Therefore, we propose context-specific practical implications (e.g. emphasis on environmental factors as a cause of mental health problems, messages to increase understanding not only of the possibility of recovery but also of challenges PMHP face) for the Philippines.
Peer Review reports
Stigma and discrimination against people with mental health problems (PMHP) are a global public health issue [ 1 , 2 , 3 ] and can have substantial negative impacts on all aspects of a person’s life, from employment and housing to social and family life [ 4 , 5 , 6 , 7 ]. Public stigma, the general public’s reaction towards a stigmatised group, can be conceptualised as having three distinct elements [ 8 ]. First, a negative belief about a stigmatised group is seen as stereotype. Second, an emotional reaction to the stereotype is seen as prejudice. Third, a behavioural manifestation of the prejudice is discrimination. Historically, research on stigma related to mental health has been conducted mainly on stereotypes, prejudices, and intentions to discriminate that are held by the general public with regard to PMHP. Such research revealed that the general public frequently label PMHP as dangerous, blameworthy, incompetent and weak, which is often accompanied with emotions of fear and anger and can lead to behavioural intention of avoidance, punishment, and coercion [ 9 , 10 , 11 , 12 ]. Further, the literature shows that internalisation of public stigma or self-stigma is also frequent among PMHP, which reduces self-esteem, causes social isolation, and inhibits help-seeking behaviour [ 6 , 13 , 14 , 15 ].
Recent research has more often investigated levels of discrimination using direct reports from PMHP. The results of such research suggest that discrimination against PMHP is a universal phenomenon around the world [ 2 , 3 , 16 ]; however, PMHP’s experiences of discrimination and its related factors might differ in high-income countries (HICs) versus low- and middle- income countries (LMICs). Some studies suggest that PMHP experience a lower level of stigma in LMICs [ 17 ], such as India [ 18 ], China [ 19 ], and Nigeria [ 20 ], compared with HICs. The reasons for the more positive acceptance of PMHP in those settings have been considered to be a more supportive environment with social cohesion as well as more social role options that PMHP are able to fulfil [ 21 , 22 ]. At the same time, there is also accumulating evidence revealing that in LMICs, experiences of stigma, discrimination and human rights abuses related to mental health problems are common and severe [ 23 , 24 , 25 , 26 , 27 ]. The stigmatisation in LMICs has been attributed to the combined effects of socioeconomic and ethno-cultural characteristics of the setting [ 28 ]. For example, the economic situation of widespread poverty may contribute to further marginalisation of PMHP who are not able to financially contribute to society [ 29 ]. Moreover, the cultural value of collectivism may results in discrimination towards PMHP especially with regarding to marriage and childrearing, since a person’s mental health problem is often seen as the family’s mental health problem [ 30 ]. Overall, practices and outcomes of stigma differ across cultures and socioeconomic backgrounds [ 29 , 31 , 32 ], and meaningful comparison across cultural settings may not be achievable with cross-cultural measures [ 33 ]. In consideration of this, researchers have called for an in-depth qualitative exploration of the experiences of stigma among PMHP in LMICs settings, where about 85% of the world’s population live [ 21 ].
PMHP in the Philippines, a lower-middle income country in Asia, might experience a significant level of stigma and discrimination. Filipino immigrants believed that personal characteristics (i.e. self-centeredness and “soul weakness”) resulted in mental health problems [ 34 , 35 ], which have been shown to be related to blaming PMHP and discriminatory behaviour in other settings [ 36 ]. Also, a multi-country survey revealed that, among 16 countries surveyed, the Philippines had the second highest proportion of citizens who agreed that PMHP should not be hired for a job even if they are qualified [ 37 ]. Further, some studies that involved interviews with Filipino immigrants living in Australia and the United States and that sampled from the general population revealed that a fear of being labelled as ‘crazy’ and spoiling their family’s reputation made Filipinos hesitate to seek help from mental health professionals [ 35 , 38 , 39 ]. Although these previous studies provide some knowledge regarding public stigma in the Filipino context, all of them looked at stereotypes, prejudices and intentions to discriminate held by the general public towards PMHP. To our knowledge, there is no study investigating PMHP’s own experiences of being stigmatised and discriminated against and the related factors in the Philippines.
To fill the gaps in the literature, we conducted a qualitative study on the factors related to experiences of stigma as well as the experiences itself of PMHP in the Philippines, using interviews with PMHP and people who know them well. Revealing the existence, types, and sources of stigma experienced by PMHP in the Philippines can contribute to the stigma research in Asian LMIC settings. Further, exploring the experiences of stigma and its related factors can provide fundamental knowledge for the design of an effective stigma reduction program in the Filipino setting.
The current research utilised the principles of constructivist grounded theory, which is deemed suitable for revealing the social phenomenon of PMHP’s experiences of stigma [ 40 ] in the Filipino context. The constructivist grounded theory assumes a relativist ontology (accepting that multiple realities exist) and a subjectivist epistemology (involving a co-construction of meaning through interaction between the researcher and participant) [ 41 ]. It provides a means of studying power, inequality, and marginality [ 42 ].
Our study was conducted in Muntinlupa, the southernmost city in the Philippines’ National Capital Region. The city has a population of 481,461 as of 2016. The majority comprises Tagalog ethnic groups and professes Christian, primarily Roman Catholic, faith. Households below the food threshold, the minimum income required to meet basic food needs, account for 21.5% of the total in the city [ 43 ]. The majority of citizens cannot afford private medical services, which cost five times more than the public medical services [ 44 ]. With respect to public psychiatric service, the city has one outpatient and no in-patient facility. The nearest public in-patient psychiatric facility is located about 23 km away.
Main data collection
Participants.
We collected data on PMHP from three different sources of information: PMHP themselves, their carers, and community health volunteers who knew them well. The eligibility criteria for PMHP were 1) having a mental health problem, listed in the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5), or epilepsy, and 2) currently not using residential care. Epilepsy was included for several reasons. First, people with epilepsy are known to suffer stigma and discrimination [ 45 , 46 ]. Second, the condition has a long history of being classified as a psychiatric problem [ 47 ]. Third, even with the present-day efforts promoting mental health in LMICs, epilepsy is often treated together with mental health issues [ 48 ]. Last, pilot interviews revealed that local lay people do not clearly differentiate epilepsy from mental health problems.
For the recruitment, we approached 42 PMHP in person; one of them declined to participate owing to time constraints. Thus, we obtained informed consent from 41 PMHP. Among them, two PMHP were excluded because they were confirmed to have only physical health problems and no mental health problems as listed in DSM-5. Consequently, we used data of 39 PMHP for our analysis. The profiles of the final sample are shown in Table 1 . In 20 of the PMHP, we interviewed the PMHP and their main carer, usually a parent or sibling. In the remaining 19 PMHP, only a main carer was interviewed, as the 19 PMHP had communication difficulties that hindered them from answering interview questions. Additionally, in 11 PMHP, we conducted interviews with a community health volunteer who was in charge of the district in which the PMHP lived.
Recruitment
We aimed to include a wide variation in the characteristics of the PMHP, namely, gender, age, marital status, educational attainment, employment status, religion, type of mental health problem, and history of using health and welfare services. To achieve this, the participants were recruited by purposive sampling in cooperation with two different collaborating stakeholders. First, as stigma was considered to inhibit Filipino people from seeking professional help for their mental condition [ 35 , 49 ], we recruited the majority of PMHP ( n = 36) in cooperation with community health volunteers, which enabled us to recruit PMHP regardless of their history of receiving health care. The community health volunteers had good knowledge of the profiles of the residents of the district under their charge and covered all the areas of the city. Second, we recruited a small number of PMHP ( n = 3) with common mental health problems (e.g. anxiety and depressive problems) from the outpatient clinical practice of a psychiatrist, as the community health volunteers did not identify any people with these types of problems.
To check the eligibility of those who had never been diagnosed by a specialist as having a mental health problem, a research member, ET, carefully reviewed the data of the individual participants, including interview recordings, transcriptions, and field notes, and then provided informed presumption if the participants had a mental health problem or not. ET also assessed which chapter, the broadest classification in DSM-5, the participant most fitted. ET has clinical experience as a psychiatrist in Japan for over 15 years.
Interview procedures
Data on the PMHP were collected through semi-structured in-depth interviews. Prior to the beginning of data collection, an interview guide was developed, referring to previous research [ 18 , 50 ], and then modified based on six pilot interviews in the setting. The interview guide had a series of open questions on three major topics: onset of mental health problems and coping behaviours, experiences of being treated negatively owing to the problem and its consequences, and activities PMHP gave up because of how others might respond to their health problem. The interview guides for interviews with PMHP and for interviews with carers and community health volunteers can be accessed in Additional files 1 and 2 , respectively. Consistent with the grounded theory methods, we used the interview guide as a flexible tool that could be revised as the analysis progressed. The carers and community health volunteers were not asked about their own experiences of stigma as a carer or person working in mental health. Instead, we asked them about the PMHP’s experiences regarding the same topics, based on their observations. Demographic data of the PMHP were also obtained at the beginning of the interview.
The first author, CT (female, a Japanese public health nurse), conducted all of the data collection between January and March 2017. During the interview, Tagalog or English was used as preferred by the participants. When Tagalog was chosen, the interviews were interpreted by one of two health workers who had lived in the city for more than 30 years and were fluent in both Tagalog and English. After explaining the study and gaining informed consent, the interviews were conducted in their home, a health centre, or the city hospital, depending on the participants’ preference. Wherever possible, we conducted interviews in a space where there was no one but the interviewee, interviewer, and interpreter around. However, five PMHP were not willing to be interviewed alone. In which case, a family member was in the same place and assisted the interview. All the interviews were digitally recorded with interviewees’ permission and lasted between 19 and 53 min; the median length was 29 min. The participants received 100 Philippine pesos (1.9 US dollars) as acknowledgement for their participation.
Supplementary data collection
We included data of interviews with seven health workers into our analysis to gain a wider perspective on the stigma experienced by PMHP. CT conducted the interviews during her one-month participant observation at health services provided by the city government. During the observation, CT discussed the role of stigma and its impact on PMHP with more than 85 health and welfare workers. We analysed seven interviews with those who shared episodes on PMHP with whom they were in direct contact as a part of their duty at work. The interviewees were three community health volunteers, two nurses, one doctor, and one rehabilitation program officer. Notes were taken during the interviews and six out of seven interviews were audiotaped with their permission.
All of the recordings were transcribed verbatim by two trained transcribers. Tagalog recordings were simultaneously translated into English by the transcribers fluent in English and Tagalog. An independent research assistant randomly selected 10% of the English transcripts and checked their accuracy by matching them with the Tagalog and English recordings. During this checking process, no significant errors were found thus the transcripts were quality assured.
Data analysis started as soon as the initial data were collected. We set aside theoretical ideas from the existing literature; instead, we remained open to exploring the theoretical possibilities we could discern from the data. After reading each of the transcripts at least twice, CT and ET independently conducted the initial coding. Simple codes were created to describe the phenomenon in each segment of data, using the qualitative data analysis software, Nvivo Version 11.4.1 (QSR International, 2016). The initial codes with identical meanings were merged through discussion, whereas those with different meanings were left unchanged to increase the variety in the interpretation of the data. We used data from interviews with cares, health volunteers, health and welfare workers to increase variety of data on stigma experienced by PMHP and gain comprehensive understanding of its context. Thus, when accounts showed some discrepancy between a person with mental health problem and his/her carer or a person who knew him/her well, we used the data from both accounts for our analysis.
The authors gradually moved on to the focus coding, in which the initial codes were concentrated on or collapsed into categories that make analytical sense, and then tested these against extensive data. The interpersonal interaction between people with and without mental health problems was treated as the central phenomenon of our interest. To explore comprehensively PMHP’s experiences of stigma, we decided to treat any “uncomfortable treatments from others” reported as stigma experience, regardless of the actors’ motivation. We constantly compared data on similarities and differences within a participant as well as across participants to examine the categories and develop links among them. CT led the preliminary focus coding. Subsequently, discussions were held between CT, ET, and HM, in which we reviewed the developed categories and links to determine if they were grounded in data and sufficiently explained the phenomenon.
After analysing the data of the 35 PMHP, a tentative model that explains the relations between categories was developed. We then collected and analysed data on four additional PMHP. Through discussion, the full research team determined that the categories and themes were sufficiently relevant and that the model held true for these additional PMHP. We then concluded that the model was theoretically saturated.
Analyses revealed four interrelated themes surrounding stigma experienced by PMHP: (1) the context affecting stigma experience, (2) stigma experience, (3) impact modifier of the stigma experience, and (4) consequence of the stigma experience. Figure 1 shows the relationship among the themes.
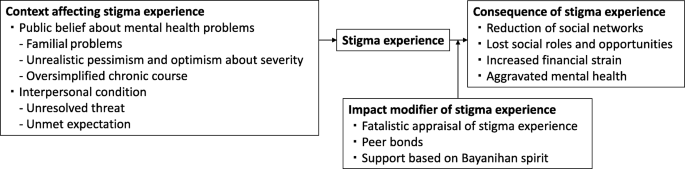
Stigma experienced by people with mental health problems and its related factors in the Philippines
Context affecting stigma experience
We identified two contextual categories that changed how others treated PMHP in a negative way.
Public belief about mental health problems
Public beliefs surrounding mental health issues are a contextual category of stigma experienced by PMHP in the Philippines. It consists of three themes: familial problems, unrealistic pessimism and optimism about severity, and oversimplified chronic course.
Familial problems
Community health volunteers and health workers observed that families of PMHP and people in the local community do not provide appropriate support for PMHP because they perceive mental affliction as a family problem and indicative of so-called “bad blood”. The belief that mental health problems can be transmitted among relatives pushed families of PMHP to deny the existence of mental health issues and people in the community to distance themselves from PMHP. A nurse shared an episode of a male patient with depression:
His family could not accept the idea that one of their relatives is actually depressed. (…) It’s because in our culture, when it comes to mental illness, it tends to be a family affair. People think if one of you has a history of mental illness, there is a chance that almost all of you already have that as well. We care about how others think about our family more than anything else. And other people feel that it is not their place to intervene in some family matters. (Interview 48, Nurse, Female)
In particular, marrying age PMHP faced stigma because of the belief in heredity. People in the community often believe that PMHP have mental health problems in their family’s blood and are afraid of developing those problems in their kinship via marriage.
I had one neighbour that I reported to the barangay [district government] because she mocked me. She was saying that I had mental illness in our blood and no one dare marry me and get in trouble. (Interview 51, PMHP, Male)
Unrealistic pessimism and optimism about severity
PMHP experienced stigma when others were overly pessimistic about the severity of a mental health problem. Participants often criticised those who believe that mental health problems generally cause severe functional impairments. This belief has resulted in unfair treatment towards PMHP in the Philippines.
[Researcher: What is the biggest challenge for the [social inclusion] program?] Finding a job. It’s very difficult. The community people don’t believe they [PMHP] are functional and don’t hire them. (…) So now some barangays [district governments] have started to hire them. We hope people see them working hard and start to trust them. (Interview 27, Rehabilitation program officer, Male)
Meanwhile, unrealistic optimism about its severity also caused stigma. The commonly held belief is that individuals are able to overcome any psychological suffering by themselves, and as a result, it will not become a serious problem. It was common for PMHP to be doubted or withheld empathy in such a culture that emphasises resilience and humour under stressful situations.
Filipinos are proud of being resilient. We find something funny in any difficult situation. But when you have this illness, that kind of thinking gives you a huge pressure. (…) One day, I opened up about my mental illness to my friends, but they all had the same reaction. They laughed at me and didn’t take it seriously. (Interview 71, PMHP, Female)
Oversimplified chronic course
The oversimplified chronic course of mental health problems emerged as one of the causes of stigma. People without any experience of a mental health problem often misunderstand the repetitive relapse and remission in the course of a mental health problem. They tend to apply an acute illness model and expect a complete cure in the short term. However, as the symptoms are prolonged, they begin to mistrust the PMHP’s account.
After one month of no work, I was able to work and sleep. But in February, it came back. I couldn’t sleep for several days. (...) My supervisors were thinking that I should be working a night shift duty, but I told them that I would have to take sick leave. But because it was the same reason for my previous absent, they are already thinking that I am making up stories. (Interview 30, PMHP, Male)
Interpersonal condition
Interpersonal condition was identified as a direct trigger of stigma experience. It consists of two themes: unresolved threat and unmet expectation.
Unresolved threat
Unresolved threat is a condition where PMHP are at risk of hurting themselves or others owing to their mental health problems, with the people in contact with the PMHP failing to manage such risks. Under such conditions, PMHP often experience physical violence, being avoided, and being restricted by others. Although the PMHP, their families, and community health volunteers attributed the threats to PMHP’s personal factors, such as personality and outwardly noticeable symptoms, they also emphasised the culpability of people in the local community for their lack of understanding and skills in interacting with PMHP. When others became familiar with PMHP, they successfully managed those threats and prevented PMHP from experiencing stigma. The mother of a boy with a neurodevelopmental problem told us:
My son easily becomes violent. For example, when someone takes and plays with his toy. The neighbours don’t understand why he is angry and they bully him. But there are also some playmates who fully understand him. When they know that my son is about to be angry, they immediately keep distance from him. And after a while, my son calms down and they start playing around together. (Interview 4, Mother of a boy with a mental health problem)
Unmet expectation
Unmet expectation was another context of stigma. In this context, there is a gap between PMHP’s abilities and other people’s expectations of them. Some PMHP reported suffering from stigma when others’ expectations were too high for their situation. People in this cultural setting tend to value strong bonds and reciprocity among families and neighbours. PMHP sometimes were unable to perform in accordance with this value owing to their mental health conditions. Violation of this value was judged as morally wrong.
They [the neighbours] say I should help my mum by doing washing, cleaning, and taking care of my brother, even when I say I feel weak or don’t know how to. (Interview 5, PMHP, Female) She is big but still doesn’t help her mother. That’s why the neighbours don’t like her. They say she is not a good daughter. (Interview 18, Community health volunteer, Female)
Meanwhile, some other PMHP experienced stigma when others underestimated PMHP’s abilities. Families often criticised other people that looked only at PMHP’s disabilities but not at their abilities.
When someone in our neighbourhood was trying to talk to my sister and she did not respond back, they started bullying her and calling her crazy. [Researcher: How do you think we can change such situation?] I think proper communication towards her would be the best since she’s really a good listener. The problem is that other people don’t know she actually understands things really well. (Interview 8, Sister of a woman with a mental health problem)
Stigma experience
Although we frequently found that PMHP were positively treated by others because of their mental health problems, we also discovered that almost all the PMHP participants were faced with negative treatment from others. PMHP experienced psychological abuse (e.g. being verbally insulted, laughed at, stared at, gossiped about, doubted), physical violence (e.g. being hit, stones being thrown at them), being restricted (e.g. being told not to go outside alone, tied with a rope to a pillar), not being supported (e.g. lack of understanding and sympathy), being taken advantage of (e.g. being cheated out of money and belongings), being neglected (e.g. privacy not being protected, medical care not being provided), and being rejected (e.g. not being associated with, not being hired). Families were an important source of stigma in terms of prominence as stigma from families was often repetitive (e.g. frequently being slapped) and prolonged (e.g. being locked up in a room for several months). PMHP also experienced stigma frequently from their neighbours, and sometimes from school friends, co-workers and employers. People who were involved with PMHP as a part of their duty at work (i.e. health workers and public safety officers) were a source of stigma as well. For complete information on the stigma experience by source, please see Table 2 .
Impact modifier of stigma experience
Even if the nature of stigma experiences were similar, the extent and degree of its influence on PMHP’s life varied depending on impact modifier of stigma experience . PMHP had three impact modifiers consisting of internal (i.e. fatalistic appraisal) and external (i.e. peer bonds, community unity) factors.
Fatalistic appraisal of stigma experience
Fatalistic appraisal of stigma experience offered PMHP and their families a strategy to cope with the emotional pain caused by stigma experience. People in the setting generally believed that God predetermined life events in the past, present and future. Some PMHP and their family accepted unfair treatments from others as “fate.” They were able to remain hopeful because they believed that God would help them if they had faith in God.
Sometimes people say he is crazy. [Researcher: What do you do in response to that?] Nothing. People say what they want to say. We just say “God is good.” As long as we believe in Him, it will be alright. (Interview 23, Sister of a man with a mental health problem)
Peer bonds , the emotional bonds with other people with similar mental health problems, empowered PMHP to change their stigmatised situation in a positive way. Stigma experience could marginalise them in the community, but when they were together with peers who understood not only their health condition but also their lowered social status, they were empowered and motivated to change the situation for themselves and their peers.
[Researcher: What are the barriers to your recovery?] The different perceptions of people towards us [she and other people with mental health problems]. It is so discouraging for us. And we are the only ones who can understand each other very well. We are like brothers and sisters already. Nevertheless, we make sure that the reason we join the [rehabilitation] program is not only for ourselves but to show them that we can change ourselves for the better. If we will be given a chance to work again, we will make 100 percent effort to get things done accordingly. (Interview 34, PMHP, Female)
Support based on Bayanihan spirit
Support based on Bayanihan spirit , a traditional concept of community unity, relieved the negative impacts of stigma on PMHP. It was not rare that community people gave food or rented a house free to PMHP and their family who had little income. Helping one another in a time of need was inherent in their lives, called Bayanihan in Tagalog. For example, a homeless woman with schizophrenia told us that she had felt hopeless because she had been bullied at school and was in a materially deprived circumstance. However, she was now enjoying her life and managing to make a living because some of her neighbours treated her as a valued community member (e.g. regularly invited her to a local dancing event) and occasionally gave her food. A community health volunteer explained why she had good relationships with the community as follows:
That is natural here. When your family member is sick, neighbours and friends are there to pay for medicines, bring food, help with housework, and take care of small kids. We call it Bayanihan. (Interview 3, Community health volunteer, Female)
Consequence of stigma experience
Stigma experience was found to bring about a substantial negative impact on PMHP’s social networks, roles, opportunities, and mental health.
Reduction of social networks
Stigma experience reduced PMHP’s social networks, which led to them spending their days isolated at home without any interaction with people outside of their immediate family. This was due not only to the direct influence of experiences of stigma (i.e. being physically restrained , being avoided by others ) but also the indirect influence of changes in three aspects: PMHP’s behaviour, restriction by families, and relationships with others. First, after being negatively treated, PMHP tended to “close off to everybody” and distanced themselves from others.
Going out is sometimes like an obstacle. (…) After that [hearing my friends gossiping about me], I have been afraid of people’s judgments. (Interview 62, PMHP, Female)
Second, families started to restrict PMHP’s behaviour to protect them from further stigma experiences.
We do not allow him to go out. We are afraid that something like that [neighbours calling him crazy] might happen to him again or someone might abduct him. (Interview 9, Sister of a man with a mental health problem)
Third, stigma experiences provoked conflicts, from a quarrel to a physical fight, and worsened the relationship between PMHP and others. The conflicting relationships produced a further stigmatising attitude towards PMHP.
He got into a fight with his playmates because they said bad words to him. (…) Many of our neighbours told me that he should be in a cell. They told me that they knew a policeman who could put him in jail. (Interview 1, Mother of a man with metal health problem)
Lost social roles and opportunities
As a result of stigma experience, PMHP lost social roles and opportunities , such as being employed, going to school, having a romantic partner, getting married, parenting, helping with household chores and the family business, taking care of younger siblings and joining religious activities.
She was a member of the choir in church. She likes singing and has a good voice. And plenty of friends visited her in the past and they went to church together. But no more. Nobody visits her, and she quit attending it. (Interview 10, Mother of a woman with a mental health problem)
Increased financial strain
Lost social roles and opportunities increased financial strain, which negatively affected the families as well as PMHP themselves. In this setting, PMHP and their families lived in communities where many people find it difficult to make a living. The cost of transportation to medical facilities and treatment fees put them in a further difficult situation economically. In such conditions, entire families often suffered from the financial strain that was due to stigma to the degree that they could not afford basic items including food and clothing.
If only I could find a good job like when I was well. Even though we do not have enough money to buy things, my family really makes an effort to find ways that we can buy those medicines. (Interview 20, PMHP, Male)
Aggravated mental health
The participants reported that the stigma experiences aggravated mental health in PMHP. The memory of negative treatment from others often stuck in their mind and its influence lasted for a long time. A 32-year-old woman with anxiety problem explained how the experience of being bullied when she was a teenager influenced her current condition:
It triggers my anxiety. When I remember their facial expressions, even now, I feel overwhelmed and breathless (Interview 39, PMHP, Female).
The experience of stigma also affected the mental health condition of PMHP by preventing them from seeking help. Some PMHP and their families choose to keep their mental health status a secret. However, families have limited capacities to take care of a person with a mental health problem, especially in the case of someone with severe symptoms. In the worst case in terms of the influence of stigma on PMHP’s mental health, a community health volunteer reported that the parents of a daughter with a mental health problem locked her up in her room and took care of her without seeking professional help. However, her condition kept deteriorating and eventually she committed suicide inside her room.
To our knowledge, this is the first study to document the stigma experienced by PMHP in the Philippines. This study adds to the understanding of discrimination in LMIC settings and its related contextual factors in the Philippines.
First, our results showed that PMHP in the Philippines experienced stigma, which brought about negative impacts on PMHP’s social networks, roles and opportunities, financial burden, and mental health. Although stigma types, sources, and areas of impact were generally consistent with the existing literature in this field [ 4 , 6 , 51 ], we found that experiences of stigma threatened the economic survival of the entire family of PMHP and increased the mental health crisis in the LMIC context, given the minimal welfare and mental health care provisions. Several studies with participants recruited from clinical settings have shown that PMHP in LMICs suffered less from stigma [ 2 , 18 , 19 , 20 ]. In this study, we involved PMHP without psychiatric service use, which prevented us from overlooking the stigma experienced by the poorest and most marginalised PMHP. Our findings might better reflect the reality in LMIC settings, where it is estimated that more than 70% of PMHP receive no treatment for their mental health conditions [ 52 ].
Second, we found that pessimistic and over-optimistic reactions to a mental health problem are among the important contexts of experiences of stigma in the Philippines. Historically, stigma research has mainly focused on the pessimistic view on the prognosis and its negative effects [ 10 , 53 , 54 , 55 , 56 ]. Meanwhile, when the over-optimistic view on the outcome of mental health problems has been documented among Filipino immigrants, it was only recognised as a barrier to help-seeking [ 35 , 39 ]. Our qualitative exploration’s original finding is that the over-optimistic belief among the community regarding the severity of mental health problems results in PMHP’s receiving inappropriate or negative treatment. This is an important finding for the Philippines, because resilience and optimism under difficult situations are among the well-known cultural traits of Filipinos [ 57 , 58 ]. Stigma resulting from optimism might be prevalent in the Philippines; a prior study showed that among the 16 countries, the Philippines posted the highest proportion of respondents who agreed that mental illness would improve on its own [ 59 ].
Third, the results indicated that mental health problems were perceived as problems of the family and discouraged people from accepting mental health problems. The finding is consistent with psychiatrists’ clinical experiences with Filipino patients [ 60 , 61 ]. We also found that a belief in transmissibility among relatives led to PMHP experiencing reduced marriage opportunities. Previous studies conducted on Chinese descent groups [ 62 , 63 , 64 ] showed that the threat of genetic contamination was related to endorsement of reproductive restriction. We propose that it might hold true in the Filipino context, meaning that the threat to family lineage through genetic contamination via marriage accounts for some of the discrimination experienced by PMHP.
Fourth, we revealed a context-specific impact modifier of stigma experiences, namely, fatalistic appraisal of stigma experience . Existing studies have discussed that Filipinos typically attribute illness to “the will of God” [ 39 , 49 , 65 ]. A new finding of this study is that negative treatments from others were also attributed to fate. Globally, it is known that fatalistic appraisal of negative events inhibits active coping and worsens health [ 66 , 67 ]. However, we found that fatalism offered a spiritual coping strategy and shielded PMHP from the adverse effects of stigma in the Catholic dominant setting of the Philippines. These findings are consistent with the literature that have showed that fatalism facilitates adjustment to negative life events [ 49 , 68 , 69 ]. Moreover, support based on Bayanihan spirit was another culturally relevant impact modifier. The origin of the Bayanihan spirit is traced back to the country’s tradition wherein towns’ people cooperate to carry a family’s entire house on their shoulders to a new location. It is considered a core essence of the Filipino culture. Our finding supports the arguments by Lasalvia [ 21 ] and Mascayano et al. [ 29 ] that communal network, which tends to be better maintained in LMICs, is among the existing strengths to reduce the negative effects of stigma.
Lastly, the research method of obtaining perspectives from multiple participants who witnessed and experienced stigma allowed us to reveal that the interpersonal conditions (i.e. unresolved threat and unmet expectations ) preceded stigma experiences. Consistent with previous research from India [ 24 ] and Indonesia [ 70 ], in the setting where mental health care is not readily available at a local level, people in the community needed to cope with the possible danger of PMHP to self or others and can violate PMHP’s human rights. Similar to the results of prior qualitative analyses of interviews with PMHP and their families [ 18 , 71 ], the expectations of others in contrast to PMHP’s actual capabilities caused negative reactions from others. Those interpersonal conditions might be a more important determinant of stigma experiences than PMHP’s personal factors, considering the previous studies showing individual variables (e.g. employment status, symptom, and treatment experiences) accounted for only less than 30% of total variance of experienced stigma [ 2 , 3 ].
Practical implications
Our results suggest that mental health care must have the objective of the reduction of stigma towards PMHP. The Department of Health and Local Government Units are required by the Mental Health Act [ 72 ], established in 2018 as the first law of its kind in the Philippines, to initiate and sustain nationwide campaigns to raise the level of awareness on the protection and promotion of mental health and rights. In conducting stigma reduction campaigns, they should: 1) target families of PMHP, community people, health workers, and public safety officers; 2) avoid genetic explanations for mental health problems and emphasise the role of environmental and social factors as its cause; 3) increase public understanding of not only the possibility of recovery but also the challenges that PMHP face; and 4) improve families’ and community members’ skills in assessing and coping with possible danger posed by PMHP to self or others [ 73 , 74 , 75 , 76 ]. These interventions might be more effective when they utilise the existing communal network and increase social contact between PMHP and others [ 77 , 78 ] We also propose that mental health and welfare services for PMHP should: 1) be community-based and support PMHP in meeting expectations that are meaningful for themselves and others; 2) provide opportunities for PMHP to share their experiences with peers to empower them [ 79 , 80 , 81 ]; and 3) prevent PMHP from internalising experiences of stigma with acknowledgement of fatalistic appraisal of them as a coping strategy. Lastly, to mitigate the adverse influences of stigma, it is necessary to change the structure of health care and welfare service provision for PMHP (e.g. inclusive education, welfare benefits, and job schemes). It is also essential to provide effective and accessible mental health care.
Study limitations
We were unable to recruit people with common mental health problems who were not using psychiatric services. In fact, community health volunteers do not recognise any people having common mental health problems. This may reflect stigma-related situations where local people do not recognise the manifestation of symptoms of those problems as a health issue, or where people with those problems hide their conditions. Additionally, cultural and language barriers may have played a part in data collection and interpretation. However, we also encountered a number of situations where the interviewee provided the data collector, who was from another cultural background, with further explanations, especially on their culture. Further, some interviews were too short to be considered an in-depth interview. Also, we needed to rely in part on data from narratives of people who know PMHP well, instead of from PMHP themselves. These were because the interviewer had difficulty encouraging some participants, especially PMHP, to talk about sensitive topics. Thus, there might be experiences and related themes that we could not explore. Lastly, we conducted the study in one city; thus, the results may not be generalisable to another part of the Philippines (e.g. rural and Muslim-dominant areas).
Our findings highlight that PMHP in the Philippines experience substantial discrimination and its adverse effects are severe to the degree that it threatens the financial survival of the entire family. Culture-bound beliefs and social structure (e.g. perceiving mental health problems as a familial problems, traditional communal unity) played important roles in shaping and modifying stigma experiences. More research is needed to develop stigma reduction interventions utilising these findings and to evaluate their effectiveness.
Abbreviations
The Diagnostic and Statistical Manual of Mental Disorders
High-income countries
Low- and middle-income countries
People with mental health problems
Seeman N, Tang S, Brown AD, Ing A. World survey of mental illness stigma. J Affect Disord. 2016;190:115–121. Available from: https://doi.org/10.1016/j.jad.2015.10.011 Elsevier.
Article Google Scholar
Lasalvia A, Zoppei S, Van Bortel T, Bonetto C, Cristofalo D, Wahlbeck K, et al. Global pattern of experienced and anticipated discrimination reported by people with major depressive disorder: a cross-sectional survey. Lancet. 2013;381:55–62. Available from: https://doi.org/10.1016/S0140-6736(12)61379-8 Elsevier Ltd
Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet; 2009;373:408–415. Available from: https://doi.org/10.1016/S0140-6736(08)61817-6 . Elsevier Ltd
Sharac J, McCrone P, Clement S, Thornicroft G. The economic impact of mental health stigma and discrimination: a systematic review. Epidemiol Psichiatr Soc. 2010;19:223. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21261218 .
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45:11–27 Available from: http://www.ncbi.nlm.nih.gov/pubmed/24569086 .
Article CAS Google Scholar
Livingston JD, Boyd JE. Correlates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysis. Soc Sci Med. 2010;71:2150–2161. Available from: https://doi.org/10.1016/j.socscimed.2010.09.030 Elsevier Ltd
Link BG, Phelan JC. Conceptualising stigma. Annu Rev Sociol. 2001 [cited 2018 Jul 3];27:363–385. Available from: https://www.annualreviews.org/doi/pdf/10.1146/annurev.soc.27.1.363
Corrigan PW. Mental health stigma as social attribution: implications for research methods and attitude change. Clin Psychol Sci Pract. 2006;7:48–67 Available from: http://doi.wiley.com/10.1093/clipsy.7.1.48 .
Mannarini S, Boffo M. Anxiety, bulimia, drug and alcohol addiction, depression, and schizophrenia: what do you think about their aetiology, dangerousness, social distance, and treatment? A latent class analysis approach. Soc Psychiatry Psychiatr Epidemiol. 2015;50:27–37.
McGinty EE, Goldman HH, Pescosolido B, Barry CL. Portraying mental illness and drug addiction as treatable health conditions: effects of a randomized experiment on stigma and discrimination. Soc Sci Med; 2015;126:73–85. Available from: https://doi.org/10.1016/j.socscimed.2014.12.010 . Elsevier Ltd
Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113:163–79.
Corrigan PW, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003;44:162–79.
Corrigan P, Watson A. The paradox of self-stigma and mental illness. Clin Psychol Sci Pract. 2002;9:35–53 Available from: https://onlinelibrary.wiley.com/doi/10.1093/clipsy.9.1.35 .
Google Scholar
Evans-Lacko S, Brohan E, Mojtabai R, Thornicroft G. Association between public views of mental illness and self-stigma among individuals with mental illness in 14 European countries. Psychol Med. 2012;42:1741–52.
Mccann TV, Renzaho A, Mugavin J, Lubman DI. Stigma of mental illness and substance misuse in sub-Saharan African migrants: a qualitative study. Int J Ment Health Nurs. 2017;27:956–65.
Camden Schizoph E, Corker EA, Beldie A, Brain C, Jakovljevic M, Jarema M, et al. Experience of stigma and discrimination reported by people experiencing the first episode of schizophrenia and those with a first episode of depression: The FEDORA project Anamaria Vasilache 2 , Margda Waern 3,4 , Norman Sartorius 10 , Graham Thornicroft 1 and the FEDORA study group. Int J Soc Psychiatry. 2015 [cited 2018 Jul 3];61:438–445. Available from: http://journals.sagepub.com/doi/pdf/10.1177/0020764014551941
Lasalvia A, Van Bortel T, Bonetto C, Jayaram G, Van Weeghel J, Zoppei S, et al. Cross-national variations in reported discrimination among people treated for major depression worldwide : the ASPEN / INDIGO international study. Br J Psychiatry. 2015;207:507–14.
Koschorke M, Padmavati R, Kumar S, Cohen A, Weiss HA, Chatterjee S, et al. Experiences of stigma and discrimination of people with schizophrenia in India. Soc Sci Med; 2014;123:149–159. Available from: https://doi.org/10.1016/j.socscimed.2014.10.035 . Elsevier Ltd
Lv Y, Wolf A, Wang X. Experienced stigma and self-stigma in Chinese patients with schizophrenia. Gen Hosp Psychiatry. 2013;35:83–8. Available from: https://doi.org/10.1016/j.genhosppsych.2012.07.007 Elsevier Inc.
Oshodi YO, Abdulmalik J, Ola B, James BO, Bonetto C, Cristofalo D, et al. Pattern of experienced and anticipated discrimination among people with depression in Nigeria: a cross-sectional study. Soc Psychiatry Psychiatr Epidemiol. 2014;49:259–66.
Lasalvia A. Tackling the mental illness stigma in low- and middle-income countries: lessons learned from high-income countries and mistakes to avoid. Epidemiol Psychiatr Sci. 2015;24:395–8 Available from: https://www.cambridge.org/core/journals/epidemiology-and-psychiatric-sciences/article/tackling-the-mental-illness-stigma-in-low-and-middleincome-countries-lessonslearned-from-highincome-countries-and-mistakes-to-avoid/83D63EA7FD15A3A3F2F9085E7E1700A2 .
Rosen A. Destigmatizing day-to-day practices: what developed countries can learn from developing countries. World Psychiatry. 2006;5:21–24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1472257/ .
Alonso J, Buron A, Bruffaerts R, He Y, Posada-Villa J, Lepine JP, et al. Association of perceived stigma and mood and anxiety disorders: results from the world mental health surveys. Acta Psychiatr Scand. 2008;118:305–14.
Mathias K, Kermode M, San Sebastian M, Koschorke M, Goicolea I. Under the banyan tree--exclusion and inclusion of people with mental disorders in rural North India. BMC Public Health. 2015;15:–446 Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-1778-2 .
Maramis A, Van Tuan N, Minas H. Mental health in Southeast Asia. Lancet. 2011;377:700–2.
Minas H, Diatri H. Pasung: Physical restraint and confinement of the mentally ill in the community. Int J Ment Health Syst. 2008;2 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2442049/ .
Tawiah PE, Adongo PB, Aikins M. Mental Health-Related Stigma and Discrimination in Ghana: Experience of Patients and Their Caregivers. Ghana Med J. 2015 [cited 2018 Jul 3];49:30–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26339082 .
Lauber C, Rössler W. Stigma towards people with mental illness in developing countries in Asia. Int Rev Psychiatry [Internet]. 2007;19:157–78 Available from: https://www.ncbi.nlm.nih.gov/pubmed/17464793 .
Mascayano F, Armijo JE, Yang LH. Addressing stigma relating to mental illness in low- and middle-income countries. Front Psychiatry. 2015;6:1–4.
Abdullah T, Brown TL. Mental illness stigma and ethnocultural beliefs, values, and norms. Clin Psychol Rev. 2011;31:934–48.
Semrau M, Evans-Lacko S, Koschorke M, Ashenafi L, Thornicroft G. stugma and discrimination related to mental illness in low- and middle-income countries. Epidemiol. Psychiatr. Sci. [Internet]. 2015;24:382–94. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25937022 .
Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64:1524–35.
Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing “what matters most” to identify culture-specific aspects of stigma. Int. J. Epidemiol. [internet]. 2014;43:494–510. Available from. https://www.ncbi.nlm.nih.gov/pubmed/24639447 .
Edman JL, Johnson RC. Filipino American and Caucasian American beliefs about the causes and treatment of mental problems. Cultur Divers Ethnic Minor Psychol. 1999;5:380–6.
Thompson S, Hartel G, Manderson L, Woelz-Stirling N, Kelaher M. The mental health status of Filipinas in Queensland. Aust N Z J Psychiatry. 2002;36:674–80.
Corrigan PW, Rowan D, Green A, Lundin R, River P, Uphoff-Wasowski K, et al. Challenging two mental illness Stigmas : personal responsibility and dangerousness. Schizophr Bull. 2002;28:293–310.
Pescosolido BA, Medina TR, Martin JK, Long JS. The “Backbone” of Stigma: Identifying the Global Core of Public Prejudice Associated With Mental Illness. Am. J. Public Health [Internet]. 2013;103:853–60. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23488508 .
Gong F, Gage SJL, Tacata LA. Helpseeking behavior among Filipino Americans: a cultural analysis of face and language. J Community Psychol. 2003;31:469–88.
Javier JR, Supan J, Lansang A, Beyer W, Kubicek K, Palinkas LA. Preventing Filipino mental health disparities: perspectives from adolescents, caregivers, providers, and advocates. Asian Am J Psychol [Internet]. 2014;5:316–24 Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4319658/ .
Charmaz K. Constructing Grounded Theory. 2nd ed. SAGE Publications Ltd; 2014.
Charmaz K. Grounded theory methods in social justice research. In: Denzin NK, Lincoln YS, editors. SAGE Handb. Qual. Res. SAGE; 2011. p. 359–380.
Charmaz K. The Power of Constructivist Grounded Theory for Critical Inquiry. Qual. Inq. [Internet]. 2017;23:34–45. Available from: http://journals.sagepub.com/doi/10.1177/1077800416657105
City Government of Muntinlupa. POVERTY AND EMPLOYMENT STATISTICS [Internet]. 2017 [cited 2017 Jun 30].
Philippine Statistics Authority. Philippines National Demographic and Health Survey 2013. 2013 [cited 2017 Jun 30]. Available from: https://dhsprogram.com/pubs/pdf/FR294/FR294.pdf .
Boling W, Means M, Fletcher A. Quality of Life and Stigma in Epilepsy, Perspectives from Selected Regions of Asia and Sub-Saharan Africa. Brain Sci. [Internet]. Multidisciplinary Digital Publishing Institute (MDPI); 2018 [cited 2018 Jun 27];8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29614761 .
Herrmann LK, Welter E, Berg AT, Perzynski AT, Van Doren JR, Sajatovic M. Epilepsy misconceptions and stigma reduction: Current status in Western countries. Epilepsy Behav. [Internet]. 2016 [cited 2018 Jun 27];60:165–73. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27208826 .
Koch-Stoecker S. Neuropsychiatric issues in epilepsy. In: Matsuura M, Inoue Y, editors. Neuropsychiatr. issues epilepsy [Internet]. John Libbey Eurotext; 2010 [cited 2018 Jun 27]. p. 233. Available from: https://books.google.co.jp/books?id=FQXhAAAAQBAJ&pg=PA174&lpg=PA174&dq=epilepsy+Emil+Kraepelin&source=bl&ots=r35Oh0rwjA&sig=IZa-67-5hrTVkzSl4HEIoGkaobQ&hl=en&sa=X&ved=0ahUKEwjd26SwkvPbAhWEnZQKHUvrDZsQ6AEIsAEwEw#v=onepage&q=epilepsyAQ28EmilKraepelin&f=false .
World Health Organization. mhGAP Training Manuals - for the mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings, version 2.0 [Internet]. WHO. World Health Organization; 2017 [cited 2018 Jun 27]. Available from: http://www.who.int/mental_health/mhgap/training_manuals/en/
Tuliao AP. Mental health help seeking among Filipinos: a review of the literature. Asia Pacific J Couns Psychother [Internet]. 2014;5:124–36 Available from: http://www.tandfonline.com/doi/abs/10.1080/21507686.2014.913641 .
Yang LH, Valencia E, Alvarado R, Link B, Huynh N, Nguyen K, et al. A theoretical and empirical framework for constructing culture-specific stigma instruments for Chile. Cad. saude coletiva [Internet]. 2013;21:71–9. Available from: /pmc/articles/PMC3753780/?report=abstract.
Hamilton S, Pinfold V, Cotney J, Couperthwaite L, Matthews J, Barret K, et al. Qualitative analysis of mental health service users’ reported experiences of discrimination. Acta Psychiatr Scand. 2016;134:14–22.
Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA [internet]. 2004;291:2581–90. Available from. http://www.ncbi.nlm.nih.gov/pubmed/15173149 .
Wig NN, Suleiman MA, Routledge R, Murthy RS, Ladrido-Ignacio L, Ibrahim HH, et al. Community reactions to mental disorders. A key informant study in three developing countries. Acta Psychiatr. Scand. [Internet]. 1980;61:111–26. Available from: https://www.ncbi.nlm.nih.gov/pubmed/7361584 .
Ando S, Yamaguchi S, Aoki Y, Thornicroft G. Review of mental-health-related stigma in Japan. Psychiatry Clin Neurosci. 2013;67:471–82.
van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Comparing stigmatising attitudes towards people with substance use disorders between the general public, GPs, mental health and addiction specialists and clients. Int J Soc Psychiatry [Internet]. 2014;61:539–49 Available from: http://isp.sagepub.com/cgi/doi/10.1177/0020764014562051 .
Clement S, Jarrett M, Henderson C, Thornicroft G. Messages to use in population-level campaigns to reduce mental health-related stigma: consensus development study. Epidemiol Psichiatr Soc. 2010;19:72–9.
Dy MB. Values in Philippine culture and education. Washington, DC: CRVP; 1994.
Social Weather Stations. Social Weather Station Survey. [Internet]. 2017 [cited 2017 Nov 9]. Available from: https://www.sws.org.ph/swsmain/artcldisppage/?artcsyscode=ART-20170816103037
Pescosolido BA, Martin JK, Olafsdottir S, Long JS, Medina TR, Martin JK. The theory of industrial society and cultural schemata: does the “cultural myth of stigma” underlie the WHO schizophrenia paradox? Am J Sociol. 2015;121:783–825.
Araneta EG. Psychiatric Care of Pilipino Americans. In: Gaw AC, editor. Cult. Ethn. Ment. Illn. Washington, DC: American Psychiatric Press; 1993. p. 377–412.
Sanchez F, Gaw A. Mental health Care of Filipino Americans. Psychiatr Serv [Internet] 2007;58:810–815. Available from: https://www.ncbi.nlm.nih.gov/pubmed/17535941
Wonpat-Borja AJ, Yang LH, Link BG, Phelan JC. Eugenics, genetics, and mental illness stigma in Chinese Americans. Soc Psychiatry Psychiatr Epidemiol. 2012;47:145–56.
Yang LH, Purdie-Vaughns V, Kotabe H, Link BG, Saw A, Wong G, et al. Culture, threat, and mental illness stigma: identifying culture-specific threat among Chinese-American groups. Soc. Sci. Med. [internet]. Elsevier Ltd. 2013;88:56–67 Available from: https://doi.org/10.1016/j.socscimed.2013.03.036 .
Yang LH, Kleinman A. “Face” and the embodiment of stigma in China: the cases of schizophrenia and AIDS. Soc Sci Med. 2008;67:398–408.
Abad PJB, Tan ML, Baluyot MMP, Villa AQ, Talapian GL, Reyes ME, et al. Cultural beliefs on disease causation in the Philippines: challenge and implications in genetic counseling. J Community Genet. 2014;5:399–407.
De Los Monteros KE, Gallo LC. The relevance of fatalism in the study of Latinas’ cancer screening behavior: a systematic review of the literature. Int J Behav Med. 2011;18:310–8.
Roberts RE, Roberts CR, Chen IG. Fatalism and risk of adolescent depression. Psychiatry [internet]. 2000;63:239–52. Available from. http://www.ncbi.nlm.nih.gov/pubmed/11125670 .
Cheng H, Sit JWH, Twinn SF, Cheng KKF, Thorne S. Coping with breast Cancer survivorship in Chinese women the role of fatalism or fatalistic voluntarism. Cancer Nurs. 2013;36:236–44.
Gonzalez P, Nuñez A, Wang-Letzkus M, Lim J-W, Flores KF, Nápoles AM. Coping with breast cancer: reflections from Chinese American, Korean American, and Mexican American women. Heal Psychol [Internet] 2016;35:19–28. Available from: https://www.ncbi.nlm.nih.gov/pubmed/26389720 .
Nurjannah I ,Mills J PT& UK. Human rights of the mentally ill in Indonesia. Int Nurs Rev. 2015;62:153–61.
Habtamu K, Alem A, Hanlon C. Conceptualizing and contextualizing functioning in people with severe mental disorders in rural Ethiopia: a qualitative study. BMC psychiatry [internet]. 2015;15:34. Available from: https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0418-9 .
An act establishing a national mental health policy for the purpose of enhancing the delivery of integrated mental health services, promoting and protecting the rights of persons utilizing psychiatric, neurologic and psychosocial health services, APPROPRI [Internet]. Republic of the Philippines; 2018. Available from: http://www.officialgazette.gov.ph/2018/06/20/republic-act-no-11036/
Kitchener B, Jorm A. Mental health first aid training for the public: evaluation of effects on knowledge, attitudes and helping behavior. BMC Psychiatry [Internet]. 2002;2:10. Available from: http://www.biomedcentral.com/1471-244X/2/10
Morgan AJ, Ross A, Reavley NJ. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. Doran CM, editor. PLoS One [Internet]. 2018 [cited 2018 Jun 28];13:e0197102. Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197102 .
Bond KS, Jorm AF, Kitchener BA, Reavley NJ. Mental health first aid training for Australian medical and nursing students: an evaluation study. BMC Psychol. [Internet]. 2015 [cited 2018 Jun 28];3:11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25914827 .
Jorm AF, Kitchener BA, Fischer J-A, Cvetkovski S. Mental Health First Aid Training by e-Learning: A Randomized Controlled Trial. Aust. New Zeal. J. Psychiatry [Internet]. 2010 [cited 2018 Jun 28];44:1072–81. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21070103 .
Corrigan PW, Morris SB, Michaels PJ, Rafacz JDRN. Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatr. Serv. [Internet]. 2012;63:963–73 Available from: https://www.ncbi.nlm.nih.gov/pubmed/23032675 .
Corrigan PW, Michaels PJ, Vega E, Gause M, Larson J, Krzyzanowski R, et al. Key ingredients to contact-based stigma change: A cross-validation. Psychiatr. Rehabil. J. [Internet]. 2014 [cited 2018 Jun 28];37:62–4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24417232 .
Corrigan PW, Larson JE, Michaels PJ, Buchholz BA, Del Rossi R, Fontecchio MJ, et al. Diminishing the self-stigma of mental illness by coming out proud. Psychiatry Res. 2015;229:148–54.
Rüsch N, Abbruzzese E, Hagedorn E, Hartenhauer D, Kaufmann I, Curschellas J, et al. Efficacy of Coming Out Proud to reduce stigma’s impact among people with mental illness: pilot randomised controlled trial. Br. J. Psychiatry [Internet]. 2014 [cited 2018 Jun 28];204:391–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24434073 .
Corrigan PW, Rüsch N, Scior K. Adapting disclosure programs to reduce the stigma of mental illness. Psychiatr. Serv. [internet]. 2018 [cited 2018 Jun 28];appi.Ps.2017004. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29606076 .
Download references
Acknowledgments
We are grateful to the interviewees for their participation. We would like to thank Dr. Magdalena C. Meana, Dr. Ma. Luisa Babaran-Echavez, and barangay health workers for their assistance with data collection.
Availability of data and materials
The transcripts from the interviews are confidential and will not be shared.
Author information
Authors and affiliations.
Graduate School of Health Sciences, Kobe University, 701, 2-6-2, Yamamoto-dori, Chuo-ku, Kobe, Hyogo, 650-0003, Japan
Chika Tanaka & Hiroya Matsuo
City Health Office, City Government of Muntinlupa, Muntinlupa, Philippines
Maria Teresa Reyes Tuliao
Hyogo Institute for Traumatic Stress, Kobe, Japan
Eizaburo Tanaka
Kobe City College of Nursing, Kobe, Japan
Tadashi Yamashita
You can also search for this author in PubMed Google Scholar
Contributions
CT had a major role in the conception of the study, undertook the data collection, carried out the data analysis, and had a major role in writing the manuscript. MT contributed to the design of the study, assisted the data collection and interpretation, and supervised writing the manuscript. ET assisted data collection, conducted data analysis, and revised the manuscript. YT assisted data collection and revised the manuscript. HM supervised the design of the study, had a role in data analysis, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chika Tanaka .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the ethical committee of the Graduate School of Health Sciences, Kobe University, Japan (reference number 561). The study was conducted in accordance with the ethical guidelines set forth by the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects provided by the Ministry of Health, Labour, and Welfare of Japan. The City Health Office of the local government approved a head of time our study protocol, especially ethical aspects for potentially participating citizens. Potential participants received written and oral information about the study. It was emphasized that participation was voluntary. During the data collection, we obtained written consent from all the interviewees and verbal assent from PMHP whose carers participated in the interviews. In the case where the interviewee was under 18 years old, we gained verbal assent from them and written consent from their parents.
Consent for publication
Participants were informed that the information they shared in the interviews would be published in anonymised form. Written informed consent for publication was obtained.
Competing interests
The authors declare that they have no competing interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Interview guide for interviews with people with mental health problems. A set of questions we referred while interviewing PMHP. (DOCX 88 kb)
Additional file 2:
Interview guide for interviews with carers and community health volunteers. A set of questions we referred while interviewing carers and community health volunteers. (DOCX 90 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Tanaka, C., Tuliao, M.T.R., Tanaka, E. et al. A qualitative study on the stigma experienced by people with mental health problems and epilepsy in the Philippines. BMC Psychiatry 18 , 325 (2018). https://doi.org/10.1186/s12888-018-1902-9
Download citation
Received : 20 December 2017
Accepted : 20 September 2018
Published : 05 October 2018
DOI : https://doi.org/10.1186/s12888-018-1902-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Discrimination
- Mental illness
- The Philippines
- Qualitative
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Systematic review
- Open access
- Published: 10 October 2019
An integrative review on methodological considerations in mental health research – design, sampling, data collection procedure and quality assurance
- Eric Badu ORCID: orcid.org/0000-0002-0593-3550 1 ,
- Anthony Paul O’Brien 2 &
- Rebecca Mitchell 3
Archives of Public Health volume 77 , Article number: 37 ( 2019 ) Cite this article
22k Accesses
19 Citations
1 Altmetric
Metrics details
Several typologies and guidelines are available to address the methodological and practical considerations required in mental health research. However, few studies have actually attempted to systematically identify and synthesise these considerations. This paper provides an integrative review that identifies and synthesises the available research evidence on mental health research methodological considerations.
A search of the published literature was conducted using EMBASE, Medline, PsycINFO, CINAHL, Web of Science, and Scopus. The search was limited to papers published in English for the timeframe 2000–2018. Using pre-defined inclusion and exclusion criteria, three reviewers independently screened the retrieved papers. A data extraction form was used to extract data from the included papers.
Of 27 papers meeting the inclusion criteria, 13 focused on qualitative research, 8 mixed methods and 6 papers focused on quantitative methodology. A total of 14 papers targeted global mental health research, with 2 papers each describing studies in Germany, Sweden and China. The review identified several methodological considerations relating to study design, methods, data collection, and quality assurance. Methodological issues regarding the study design included assembling team members, familiarisation and sharing information on the topic, and seeking the contribution of team members. Methodological considerations to facilitate data collection involved adequate preparation prior to fieldwork, appropriateness and adequacy of the sampling and data collection approach, selection of consumers, the social or cultural context, practical and organisational skills; and ethical and sensitivity issues.
The evidence confirms that studies on methodological considerations in conducting mental health research largely focus on qualitative studies in a transcultural setting, as well as recommendations derived from multi-site surveys. Mental health research should adequately consider the methodological issues around study design, sampling, data collection procedures and quality assurance in order to maintain the quality of data collection.
Peer Review reports
In the past decades there has been considerable attention on research methods to facilitate studies in various academic fields, such as public health, education, humanities, behavioural and social sciences [ 1 , 2 , 3 , 4 ]. These research methodologies have generally focused on the two major research pillars known as quantitative or qualitative research. In recent years, researchers conducting mental health research appear to be either employing both qualitative and quantitative research methods separately, or mixed methods approaches to triangulate and validate findings [ 5 , 6 ].
A combination of study designs has been utilised to answer research questions associated with mental health services and consumer outcomes [ 7 , 8 ]. Study designs in the public health and clinical domains, for example, have largely focused on observational studies (non-interventional) and experimental research (interventional) [ 1 , 3 , 9 ]. Observational design in non-interventional research requires the investigator to simply observe, record, classify, count and analyse the data [ 1 , 2 , 10 ]. This design is different from the observational approaches used in social science research, which may involve observing (participant and non- participant) phenomena in the fieldwork [ 1 ]. Furthermore, the observational study has been categorized into five types, namely cross-sectional design, case-control studies, cohort studies, case report and case series studies [ 1 , 2 , 3 , 9 , 10 , 11 ]. The cross-sectional design is used to measure the occurrence of a condition at a one-time point, sometimes referred to as a prevalence study. This approach of conducting research is relatively quick and easy but does not permit a distinction between cause and effect [ 1 ]. Conversely, the case-control is a design that examines the relationship between an attribute and a disease by comparing those with and without the disease [ 1 , 2 , 12 ]. In addition, the case-control design is usually retrospective and aims to identify predictors of a particular outcome. This type of design is relevant when investigating rare or chronic diseases which may result from long-term exposure to particular risk factors [ 10 ]. Cohort studies measure the relationship between exposure to a factor and the probability of the occurrence of a disease [ 1 , 10 ]. In a case series design, medical records are reviewed for exposure to determinants of disease and outcomes. More importantly, case series and case reports are often used as preliminary research to provide information on key clinical issues [ 12 ].
The interventional study design describes a research approach that applies clinical care to evaluate treatment effects on outcomes [ 13 ]. Several previous studies have explained the various forms of experimental study design used in public health and clinical research [ 14 , 15 ]. In particular, experimental studies have been categorized into randomized controlled trials (RCTs), non-randomized controlled trials, and quasi-experimental designs [ 14 ]. The randomized trial is a comparative study where participants are randomly assigned to one of two groups. This research examines a comparison between a group receiving treatment and a control group receiving treatment as usual or receiving a placebo. Herein, the exposure to the intervention is determined by random allocation [ 16 , 17 ].
Recently, research methodologists have given considerable attention to the development of methodologies to conduct research in vulnerable populations. Vulnerable population research, such as with mental health consumers often involves considering the challenges associated with sampling (selecting marginalized participants), collecting data and analysing it, as well as research engagement. Consequently, several empirical studies have been undertaken to document the methodological issues and challenges in research involving marginalized populations. In particular, these studies largely addresses the typologies and practical guidelines for conducting empirical studies in mental health. Despite the increasing evidence, however, only a few studies have yet attempted to systematically identify and synthesise the methodological considerations in conducting mental health research from the perspective of consumers.
A preliminary search using the search engines Medline, Web of Science, Google Scholar, and Scopus Index and EMBASE identified only two reviews of mental health based research. Among these two papers, one focused on the various types of mixed methods used in mental health research [ 18 ], whilst the other paper, focused on the role of qualitative studies in mental health research involving mixed methods [ 19 ]. Even though the latter two studies attempted to systematically review mixed methods mental health research, this integrative review is unique, as it collectively synthesises the design, data collection, sampling, and quality assurance issues together, which has not been previously attempted.
This paper provides an integrative review addressing the available evidence on mental health research methodological considerations. The paper also synthesises evidence on the methods, study designs, data collection procedures, analyses and quality assurance measures. Identifying and synthesising evidence on the conduct of mental health research has relevance to clinicians and academic researchers where the evidence provides a guide regarding the methodological issues involved when conducting research in the mental health domain. Additionally, the synthesis can inform clinicians and academia about the gaps in the literature related to methodological considerations.
Methodology
An integrative review was conducted to synthesise the available evidence on mental health research methodological considerations. To guide the review, the World Health Organization (WHO) definition of mental health has been utilised. The WHO defines mental health as: “a state of well-being, in which the individual realises his or her own potentials, ability to cope with the normal stresses of life, functionality and work productivity, as well as the ability to contribute effectively in community life” [ 20 ]. The integrative review enabled the simultaneous inclusion of diverse methodologies (i.e., experimental and non-experimental research) and varied perspectives to fully understand a phenomenon of concern [ 21 , 22 ]. The review also uses diverse data sources to develop a holistic understanding of methodological considerations in mental health research. The methodology employed involves five stages: 1) problem identification (ensuring that the research question and purpose are clearly defined); 2) literature search (incorporating a comprehensive search strategy); 3) data evaluation; 4) data analysis (data reduction, display, comparison and conclusions) and; 5) presentation (synthesising findings in a model or theory and describing the implications for practice, policy and further research) [ 21 ].
Inclusion criteria
The integrative review focused on methodological issues in mental health research. This included core areas such as study design and methods, particularly qualitative, quantitative or both. The review targeted papers that addressed study design, sampling, data collection procedures, quality assurance and the data analysis process. More specifically, the included papers addressed methodological issues on empirical studies in mental health research. The methodological issues in this context are not limited to a particular mental illness. Studies that met the inclusion criteria were peer-reviewed articles published in the English Language, from January 2000 to July 2018.
Exclusion criteria
Articles that were excluded were based purely on general health services or clinical effectiveness of a particular intervention with no connection to mental health research. Articles were also excluded when it addresses non-methodological issues. Other general exclusion criteria were book chapters, conference abstracts, papers that present opinion, editorials, commentaries and clinical case reviews.
Search strategy and selection procedure
The search of published articles was conducted from six electronic databases, namely EMBASE, CINAHL (EBSCO), Web of Science, Scopus, PsycINFO and Medline. We developed a search strategy based on the recommended guidelines by the Joanna Briggs Institute (JBI) [ 23 ]. Specifically, a three-step search strategy was utilised to conduct the search for information (see Table 1 ). An initial limited search was conducted in Medline and Embase (see Table 1 ). We analysed the text words contained in the title and abstract and of the index terms from the initial search results [ 23 ]. A second search using all identified keywords and index terms was then repeated across all remaining five databases (see Table 1 ). Finally, the reference lists of all eligible studies were manually hand searched [ 23 ].
The selection of eligible articles adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 24 ] (see Fig. 1 ). Firstly, three authors independently screened the titles of articles that were retrieved and then approved those meeting the selection criteria. The authors reviewed all the titles and abstracts and agreed on those needing full-text screening. E.B (Eric Badu) conducted the initial screening of titles and abstracts. A.P.O’B (Anthony Paul O’Brien) and R.M (Rebecca Mitchell) conducted the second screening of titles and abstracts of all the identified papers. The authors (E.B, A.P.O’B and R.M) conducted full-text screening according to the inclusion and exclusion criteria.
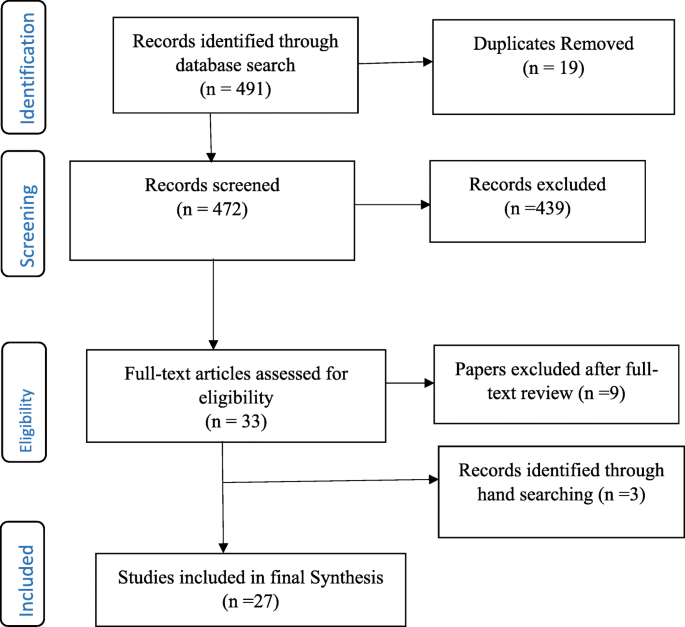
Flow Chart of studies included in the review
Data management and extraction
The integrative review used Endnote ×8 to screen and handle duplicate references. A predefined data extraction form was developed to extract data from all included articles (see Additional file 1 ). The data extraction form was developed according to Joanna Briggs Institute (JBI) [ 23 ] and Cochrane [ 24 ] manuals, as well as the literature associated with concepts and methods in mental health research. The data extraction form was categorised into sub-sections, such as study details (citation, year of publication, author, contact details of lead author, and funder/sponsoring organisation, publication type), objective of the paper, primary subject area of the paper (study design, methods, sampling, data collection, data analysis, quality assurance). The data extraction form also had a section on additional information on methodological consideration, recommendations and other potential references. The authors extracted results of the included papers in numerical and textual format [ 23 ]. EB (Eric Badu) conducted the data extraction, A.P.O’B (Anthony Paul O’Brien) and R.M (Rebecca Mitchell), conducted the second review of the extracted data.
Data synthesis
Content analysis was used to synthesise the extracted data. The content analysis process involved several stages which involved noting patterns and themes, seeing plausibility, clustering, counting, making contrasts and comparisons, discerning common and unusual patterns, subsuming particulars into general, noting relations between variability, finding intervening factors and building a logical chain of evidence [ 21 ] (see Table 2 ).
Study characteristics
The integrative review identified a total of 491 records from all databases, after which 19 duplicates were removed. Out of this, 472 titles and abstracts were assessed for eligibility, after which 439 articles were excluded. Articles not meeting the inclusion criteria were excluded. Specifically, papers excluded were those that did not address methodological issues as well as papers addressing methodological consideration in other disciplines. A total of 33 full-text articles were assessed – 9 articles were further excluded, whilst an additional 3 articles were identified from reference lists. Overall, 27 articles were included in the final synthesis (see Fig. 1 ). Of the total included papers, 12 contained qualitative research, 9 were mixed methods (both qualitative and quantitative) and 6 papers focused on quantitative data. Conversely, a total of 14 papers targeted global mental health research and 2 papers each describing studies in Germany, Sweden and China. The papers addressed different methodological issues, such as study design, methods, data collection, and analysis as well as quality assurance (see Table 3 ).
Mixed methods design in mental health research
Mixed methods research is defined as a research process where the elements of qualitative and quantitative research are combined in the design, data collection, and its triangulation and validation [ 48 ]. The integrative review identified four sub-themes that describe mixed methods design in the context of mental health research. The sub-themes include the categories of mixed methods, their function, structure, process and further methodological considerations for mixed methods design. These sub-themes are explained as follows:
Categorizing mixed methods in mental health research
Four studies highlighted the categories of mixed methods design applicable to mental health research [ 18 , 19 , 43 , 48 ]. Generally, there are differences in the categories of mixed methods design, however, three distinct categories predominantly appear to cross cut in all studies. These categories are function, structure and process. Some studies further categorised mixed method design to include rationale, objectives, or purpose. For instance, Schoonenboom and Johnson [ 48 ] categorised mixed methods design into primary and secondary dimensions.
The function of mixed methods in mental health research
Six studies explain the function of conducting mixed methods design in mental health research. Two studies specifically recommended that mixed methods have the ability to provide a more robust understanding of services by expanding and strengthening the conclusions from the study [ 42 , 45 ]. More importantly, the use of both qualitative and quantitative methods have the ability to provide innovative solutions to important and complex problems, especially by addressing diversity and divergence [ 48 ]. The review identified five underlying functions of a mixed method design in mental health research which include achieving convergence, complementarity, expansion, development and sampling [ 18 , 19 , 43 ].
The use of mixed methods to achieve convergence aims to employ both qualitative and quantitative data to answer the same question, either through triangulation (to confirm the conclusions from each of the methods) or transformation (using qualitative techniques to transform quantitative data). Similarly, complementarity in mixed methods integrates both qualitative and quantitative methods to answer questions for the purpose of evaluation or elaboration [ 18 , 19 , 43 ]. Two papers recommend that qualitative methods are used to provide the depth of understanding, whilst the quantitative methods provide a breadth of understanding [ 18 , 43 ]. In mental health research, the qualitative data is often used to examine treatment processes, whilst the quantitative methods are used to examine treatment outcomes against quality care key performance targets.
Additionally, three papers indicated that expansion as a function of mixed methods uses one type of method to answer questions raised by the other type of method [ 18 , 19 , 43 ]. For instance, qualitative data is used to explain findings from quantitative analysis. Also, some studies highlight that development as a function of mixed methods aims to use one method to answer research questions, and use the findings to inform other methods to answer different research questions. A qualitative method, for example, is used to identify the content of items to be used in a quantitative study. This approach aims to use qualitative methods to create a conceptual framework for generating hypotheses to be tested by using a quantitative method [ 18 , 19 , 43 ]. Three papers suggested that using mixed methods for the purpose of sampling utilize one method (eg. quantitative) to identify a sample of participants to conduct research using other methods (eg. qualitative) [ 18 , 19 , 43 ]. For instance, quantitative data is sequentially utilized to identify potential participants to participate in a qualitative study and the vice versa.
Structure of mixed methods in mental health research
Five studies categorised the structure of conducting mixed methods in mental health research, into two broader concepts including simultaneous (concurrent) and sequential (see Table 3 ). In both categories, one method is regarded as primary and the other as secondary, although equal weight can be given to both methods [ 18 , 19 , 42 , 43 , 48 ]. Two studies suggested that the sequential design is a process where the data collection and analysis of one component (eg. quantitative) takes place after the data collection and analysis of the other component (eg qualitative). Herein, the data collection and analysis of one component (e.g. qualitative) may depend on the outcomes of the other component (e.g. quantitative) [ 43 , 48 ]. An earlier review suggested that the majority of contemporary studies in mental health research use a sequential design, with qualitative methods, more often preceding quantitative methods [ 18 ].
Alternatively, the concurrent design collects and analyses data of both components (e.g. quantitative and qualitative) simultaneously and independently. Palinkas, Horwitz [ 42 ] recommend that one component is used as secondary to the other component, or that both components are assigned equal priority. Such a mixed methods approach aims to provide a depth of understanding afforded by qualitative methods, with the breadth of understanding offered by the quantitative data to elaborate on the findings of one component or seek convergence through triangulation of the results. Schoonenboom and Johnson [ 48 ] recommended the use of capital letters for one component and lower case letters for another component in the same design to indicate that one component is primary and the other is secondary or supplemental.
Process of mixed methods in mental health research
Five papers highlighted the process for the use of mixed methods in mental health research [ 18 , 19 , 42 , 43 , 48 ]. The papers suggested three distinct processes or strategies for combining qualitative and quantitative data. These include merging or converging the two data sets, connecting the two datasets by having one build upon the other; and embedding one data set within the other [ 19 , 43 ]. The process of connecting occurs when the analysis of one dataset leads to the need for the other data set. For instance, in the situation where quantitative results lead to the subsequent collection and analysis of qualitative data [ 18 , 43 ]. A previous study suggested that most studies in mental health sought to connect the data sets. Similarly, the process of merging the datasets brings together two sets of data during the interpretation, or transforms one type of data into the other type, by combining the data into new variables [ 18 ]. The process of embedding data into mixed method designs in mental health uses one dataset to provide a supportive role to the other dataset [ 43 ].
Consideration for using mixed methods in mental health research
Three studies highlighted several factors that need to be considered when conducting mixed methods design in mental health research [ 18 , 19 , 45 ]. Accordingly, these factors include developing familiarity with the topic under investigation based on experience, willingness to share information on the topic [ 19 ], establishing early collaboration, willingness to negotiate emerging problems, seeking the contribution of team members, and soliciting third-party assistance to resolve any emerging problems [ 45 ]. Additionally, Palinkas, Horwitz [ 18 ] recommended that mixed methods in the context of mental health research are mostly applied in studies that assess needs of services, examine existing services, developing new or adapting existing services, evaluating services in randomised control trials, and examining service implementation.
Qualitative study in mental health research
This theme describes the various qualitative methods used in mental health research. The theme also addresses methodological considerations for using qualitative methods in mental health research. The key emerging issues are discussed below:
Considering qualitative components in conducting mental health research
Six studies recommended the use of qualitative methods in mental health research [ 19 , 26 , 28 , 32 , 36 , 44 ]. Two qualitative research paradigms were identified, including the interpretive and critical approach [ 32 ]. The interpretive methodologies predominantly explore the meaning of human experiences and actions, whilst the critical approach emphasises the social and historical origins and contexts of meaning [ 32 ]. Two studies suggested that the interpretive qualitative methods used in mental health research are ethnography, phenomenology and narrative approaches [ 32 , 36 ].
The ethnographic approach describes the everyday meaning of the phenomena within a societal and cultural context, for instance, the way phenomena or experience is contrasted within a community, or by collective members over time [ 32 ]. Alternatively, the phenomenological approach explores the claims and concerns of a subject with a speculative development of an interpretative account within their cultural and physical environments focusing on the lived experience [ 32 , 36 ].
Moreover, the critical qualitative approaches used in mental health research are predominantly emancipatory (for instance, socio-political traditions) and participatory action-based research. The emancipatory traditions recognise that knowledge is acquired through critical discourse and debate but are not seen as discovered by objective inquiry [ 32 ]. Alternatively, the participatory action based approach uses critical perspectives to engage key stakeholders as participants in the design and conduct of the research [ 32 ].
Some studies highlighted several reasons why qualitative methods are relevant to mental health research. In particular, qualitative methods are significant as they emphasise naturalistic inquiry and have a discovery-oriented approach [ 19 , 26 ]. Two studies suggested that qualitative methods are often relevant in the initial stages of research studies to understand specific issues such as behaviour, or symptoms of consumers of mental services [ 19 ]. Specifically, Palinkas [ 19 ] suggests that qualitative methods help to obtain initial pilot data, or when there is too little previous research or in the absence of a theory, such as provided in exploratory studies, or previously under-researched phenomena.
Three studies stressed that qualitative methods can help to better understand socially sensitive issues, such as exploring the solutions to overcome challenges in mental health clinical policies [ 19 , 28 , 44 ]. Consequently, Razafsha, Behforuzi [ 44 ] recommended that the natural holistic view of qualitative methods can help to understand the more recovery-oriented policy of mental health, rather than simply the treatment of symptoms. Similarly, the subjective experiences of consumers using qualitative approaches have been found useful to inform clinical policy development [ 28 ].
Sampling in mental health research
The theme explains the sampling approaches used in mental health research. The section also describes the methodological considerations when sampling participants for mental health research. The sub-themes emerging are explained in the following sections:
Sampling approaches (quantitative)
Some studies reviewed highlighted the sampling approaches previously used in mental health research [ 25 , 34 , 35 ]. Generally, all quantitative studies tend to use several probability sampling approaches, whilst qualitative studies used non-probability techniques. The quantitative mental health studies conducted at community and population level employ multi-stage sampling techniques usually involving systematic sampling, stratified and random sampling [ 25 , 34 ]. Similarly, quantitative studies that recruit consumers in the hospital setting employ consecutive sampling [ 35 ]. Two studies reviewed highlighted that the identification of consumers of mental health services for research is usually conducted by service providers. For instance, Korver, Quee [ 35 ] research used a consecutive sampling approach by identifying consumers through clinicians working in regional psychosis departments, or academic centres.

Sampling approaches (qualitative)
Seven studies suggested that the sampling procedures widely used in mental health research involving qualitative methods are non-probability techniques, which include purposive [ 19 , 28 , 32 , 42 , 46 ], snowballing [ 30 , 32 , 46 ] and theoretical sampling [ 31 , 32 ]. The purposive sampling identifies participants that possess relevant characteristics to answer a research question [ 28 ]. Purposive sampling can be used in a single case study, or for multiple cases. The purposive sampling used in mental health research is usually extreme, or deviant case sampling, criterion sampling, and maximum variation sampling [ 19 ]. Furthermore, it is advised when using purposive sampling in a multistage level study, that it should aim to begin with the broader picture to achieve variation, or dispersion, before moving to the more focused view that considers similarity, or central tendencies [ 42 ].
Two studies added that theoretical sampling involved sampling participants, situations and processes based on concepts on theoretical grounds and then using the findings to build theory, such as in a Grounded Theory study [ 31 , 32 ]. Some studies highlighted that snowball sampling is another strategy widely used in mental health research [ 30 , 32 , 46 ]. This is ascribed to the fact that people with mental illness are perceived as marginalised in research and practically hard-to-reach using conventional sampling [ 30 , 32 ]. Snowballing sampling involves asking the marginalised participants to recommend individuals who might have direct knowledge relevant to the study [ 30 , 32 , 46 ]. Although this approach is relevant, some studies advise the limited possibility of generalising the sample, because of the likelihood of selection bias [ 30 ].
Sampling consideration
Four studies in this section highlighted some of the sampling considerations in mental health research [ 30 , 31 , 32 , 46 ]. Generally, mental health research should consider the appropriateness and adequacy of sampling approach by applying attributes such as shared social, or cultural experiences, or shared concern related to the study [ 32 ], diversity and variety of participants [ 31 ], practical and organisational skills, as well as ethical and sensitivity issues [ 46 ]. Robinson [ 46 ] further suggested that sampling can be homogenous or heterogeneous depending on the research questions for the study. Achieving homogeneity in sampling should employ a variety of parameters, which include demographic, graphical, physical, psychological, or life history homogeneity [ 46 ]. Additionally, applying homogeneity in sampling can be influenced by theoretical and practical factors. Alternatively, some samples are intentionally selected based on heterogeneous factors [ 46 ].
Data collection in mental health research
This theme highlights the data collection methods used in mental health research. The theme is explained according to three sub-themes, which include approaches for collecting qualitative data, methodological considerations, as well as preparations for data collection. The sub-themes are as follows:
Approaches for collecting qualitative data
The studies reviewed recommended the approaches that are widely applied in collecting data in mental health research. The widely used qualitative data collection approaches in mental health research are focus group discussions (FGDs) [ 19 , 28 , 30 , 31 , 41 , 44 , 47 ], extended in-depth interviews [ 19 , 30 , 34 ], participant and non-participant observation [ 19 ], Delphi data collection, quasi-statistical techniques [ 19 ] and field notes [ 31 , 40 ]. Seven studies suggest that FGDs are widely used data collection approaches [ 19 , 28 , 30 , 31 , 41 , 44 , 47 ] because they are valuable in gathering information on consumers’ perspectives of services, especially regarding satisfaction, unmet/met service needs and the perceived impact of services [ 47 ]. Conversely, Ekblad and Baarnhielm [ 31 ] recommended that this approach is relevant to improve clinical understanding of the thoughts, emotions, meanings and attitudes towards mental health services.
Such data collection approaches are particularly relevant to consumers of mental health services, due to their low self-confidence and self-esteem [ 41 ]. The approach can help to understand specific terms, vocabulary, opinions and attitudes of consumers of mental health services, as well as their reasoning about personal distress and healing [ 31 ]. Similarly, the reliance on verbal rather than written communication helps to promote the participation of participants with serious and enduring mental health problems [ 31 , 41 ]. Although FGD has several important outcomes, there are some limitations that need critical consideration. Ekblad and Baarnhielm [ 31 ] for example suggest, that marginalised participants may not always feel free to talk about private issues regarding their condition at the group level mostly due to perceived stigma and group confidentiality.
Some studies reviewed recommended that attempting to capture comprehensive information and analysing group interactions in mental health research requires the research method to use field notes as a supplementary data source to help validate the FGDs [ 31 , 40 , 41 ]. The use of field notes in addition to FGDs essentially provides greater detail in the accounts of consumers’ subjective experiences. Furthermore, Montgomery and Bailey [ 40 ] suggest that field notes require observational sensitivity, and also require having specific content such as descriptive and interpretive data.
Three studies in this section suggested that in-depth interviews are used to collect data from consumers of mental health services [ 19 , 30 , 34 ]. This approach is particularly important to explore the behaviour, subjective experiences and psychological processes; opinions, and perceptions of mental health services. de Jong and Van Ommeren [ 30 ] recommend that in-depth interviews help to collect data on culturally marked disorders, their personal and interpersonal significance, patient and family explanatory models, individual and family coping styles, symptom symbols and protective mediators. Palinkas [ 19 ] also highlights that the structured narrative form of extended interviewing is the type of in-depth interview used in mental health research. This approach provides participants with the opportunity to describe the experience of living with an illness and seeking services that assist them.
Consideration for data collection
Six studies recommended consideration required in the data collection process [ 31 , 32 , 37 , 41 , 47 , 49 ]. Some studies highlighted that consumers of mental health services might refuse to participate in research due to several factors [ 37 ] like the severity of their illness, stigma and discrimination [ 41 ]. Subsequently, such issues are recommended to be addressed by building confidence and trust between the researcher and consumers [ 31 , 37 ]. This is a significant prerequisite, as it can sensitise and normalise the research process and aims with the participants prior to discussing their personal mental health issues. Similarly, some studies added that the researcher can gain the confidence of service providers who manage consumers of mental health services [ 41 , 47 ], seek ethical approval from the relevant committee(s) [ 41 , 47 ], meet and greet the consumers of mental health services before data collection, and arrange a mutually acceptable venue for the groups and possibly supply transport [ 41 ].
Two studies further suggested that the cultural and social differences of the participants need consideration [ 26 , 31 ]. These factors could influence the perception and interpretation of ethical issues in the research situation.
Additionally, two studies recommended the use of standardised assessment instruments for mental health research that involve quantitative data collection [ 33 , 49 ]. A recent survey suggested that measures to standardise the data collection approach can convert self-completion instruments to interviewer-completion instruments [ 49 ]. The interviewer can then read the items of the instruments to respondents and record their responses. The study further suggested the need to collect demographic and behavioural information about the participant(s).
Preparing for data collection
Eight studies highlighted the procedures involved in preparing for data collection in mental health research [ 25 , 30 , 33 , 34 , 35 , 39 , 41 , 49 ]. These studies suggest that the preparation process involve organising meetings of researchers, colleagues and representatives of the research population. The meeting of researchers generally involves training of interviewers about the overall design, objectives and research questions associated with the study. de Jong and Van Ommeren [ 30 ] recommended that preparation for the use of quantitative data encompasses translating and adapting instruments with the aim of achieving content, semantic, concept, criterion and technical equivalence.
Quality assurance procedures in mental health research
This section describes the quality assurance procedures used in mental health research. Quality assurance is explained according to three sub-themes: 1) seeking informed consent, 2) the procedure for ensuring quality assurance in a quantitative study and 3) the procedure for ensuring quality control in a qualitative study. The sub-themes are explained in the following content.
Seeking informed consent
The papers analysed for the integrative review suggested that the rights of participants to safeguard their integrity must always be respected, and so each potential subject must be adequately informed of the aims, methods, anticipated benefits and potential hazards of the study and any potential discomforts (see Table 3 ). Seven studies highlight that potential participants of mental health research must be consented to the study prior to data collection [ 25 , 26 , 33 , 35 , 37 , 39 , 47 ]. The consent process helps to assure participants of anonymity and confidentiality and further explain the research procedure to them. Baarnhielm and Ekblad [ 26 ] argue that the research should be guided by four basic moral values for medical ethics, autonomy, non-maleficence, beneficence, and justice. In particular, potential consumers of mental health services who may have severe conditions and unable to consent themselves are expected to have their consent signed by a respective family caregiver [ 37 ]. Latvala, Vuokila-Oikkonen [ 37 ] further suggested that researchers are responsible to agree on the criteria to determine the competency of potential participants in mental health research. The criteria are particularly relevant when potential participants have difficulties in understanding information due to their mental illness.
Procedure for ensuring quality control (quantitative)
Several studies highlighted procedures for ensuring quality control in mental health research (see Table 3 ). The quality control measures are used to achieve the highest reliability, validity and timeliness. Some studies demonstrate that ensuring quality control should consider factors such as pre-testing tools [ 25 , 49 ], minimising non-response rates [ 25 , 39 ] and monitoring of data collection processes [ 25 , 33 , 49 ].
Accordingly, two studies suggested that efforts should be made to re-approach participants who initially refuse to participate in the study. For instance, Liu, Huang [ 39 ] recommended that when a consumer of mental health services refuse to participate in a study (due to low self-esteem) when approached for the first time, a different interviewer can re-approach the same participant to see if they are more comfortable to participate after the first invitation. Three studies further recommend that monitoring data quality can be accomplished through “checks across individuals, completion status and checks across variables” [ 25 , 33 , 49 ]. For example, Alonso, Angermeyer [ 25 ] advocate that various checks are used to verify completion of the interview, and consistency across instruments against the standard procedure.
Procedure for ensuring quality control (qualitative)
Four studies highlighted the procedures for ensuring quality control of qualitative data in mental health research [ 19 , 32 , 37 , 46 ]. A further two studies suggested that the quality of qualitative research is governed by the principles of credibility, dependability, transferability, reflexivity, confirmability [ 19 , 32 ]. Some studies explain that the credibility or trustworthiness of qualitative research in mental health is determined by methodological and interpretive rigour of the phenomenon being investigated [ 32 , 37 ]. Consequently, Fossey, Harvey [ 32 ] propose that the methodological rigour for assessing the credibility of qualitative research are congruence, responsiveness or sensitivity to social context, appropriateness (importance and impact), adequacy and transparency. Similarly, interpretive rigour is classified as authenticity, coherence, reciprocity, typicality and permeability of the researcher’s intentions; including engagement and interpretation [ 32 ].
Robinson [ 46 ] explained that transparency (openness and honesty) is achieved if the research report explicitly addresses how the sampling, data collection, analysis, and presentation are met. In particular, efforts to address these methodological issues highlight the extent to which the criteria for quality profoundly interacts with standards for ethics. Similarly, responsiveness, or sensitivity, helps to situate or locate the study within a place, a time and a meaningful group [ 46 ]. The study should also consider the researcher’s background, location and connection to the study setting, particularly in the recruitment process. This is often described as role conflict or research bias.
In the interpretive phenomenon, coherence highlights the ability to select an appropriate sampling procedure that mutually matches the research aims, questions, data collection, analysis, as well as any theoretical concepts or frameworks [ 32 , 46 ]. Similarly, authenticity explains the appropriate representation of participants’ perspectives in the research process and the interpretation of results. Authenticity is maximised by providing evidence that participants are adequately represented in the interpretive process, or provided an opportunity to give feedback on the researcher’s interpretation [ 32 ]. Again, the contribution of the researcher’s perspective to the interpretation enhances permeability. Fossey, Harvey [ 32 ] further suggest that reflexive reporting, which distinguishes the participants’ voices from that of the researcher in the report, enhances the permeability of the researcher’s role and perspective.
One study highlighted the approaches used to ensure validity in qualitative research, which includes saturation, identification of deviant or non-confirmatory cases, member checking and coding by consensus. Saturation involves completeness in the research process, where all relevant data collection, codes and themes required to answer the phenomenon of inquiry are achieved; and no new data emerges [ 19 ]. Similarly, member checking is the process whereby participants or others who share similar characteristics review study findings to elaborate on confirming them [ 19 ]. The coding by consensus involves a collaborative approach to analysing the data. Ensuring regular meetings among coders to discuss procedures for assigning codes to segments of data and resolve differences in coding procedures, and by comparison of codes assigned on selected transcripts to calculate a percentage agreement or kappa measure of interrater reliability, are commonly applied [ 19 ].
Two studies recommend the need to acknowledge the importance of generalisability (transferability). This concept aims to provide sufficient information about the research setting, findings and interpretations for readers to appropriately determine the replicability of the findings from one context, or population to another, otherwise known as reliability in quantitative research [ 19 , 32 ]. Similarly, the researchers should employ reflexivity as a means of identifying and addressing potential biases in data collection and interpretation. Palinkas [ 19 ] suggests that such bias is associated with theoretical orientations; pre-conceived beliefs, assumptions, and demographic characteristics; and familiarity and experience with the methods and phenomenon. Another approach to enhance the rigour of analysis involves peer debriefing and support meetings held among team members which facilitate detailed auditing during data analysis [ 19 ].
The integrative review was conducted to synthesise evidence into recommended methodological considerations when conducting mental health research. The evidence from the review has been discussed according to five major themes: 1) mixed methods study in mental health research; 2) qualitative study in mental health research; 3) sampling in mental health research; 4) data collection in mental health research; and 5) quality assurance procedures in mental health research.
Mixed methods study in mental health research
The evidence suggests that mixed methods approach in mental health are generally categorised according to their function (rationale, objectives or purpose), structure and process [ 18 , 19 , 43 , 48 ]. The mixed methods study can be conducted for the purpose of achieving convergence, complementarity, expansion, development and sampling [ 18 , 19 , 43 ]. Researchers conducting mental health studies should understand the underlying functions or purpose of mixed methods. Similarly, mixed methods in mental health studies can be structured simultaneously (concurrent) and sequential [ 18 , 19 , 42 , 43 , 48 ]. More importantly, the process of combining qualitative and quantitative data can be achieved through merging or converging, connecting and embedding one data set within the other [ 18 , 19 , 42 , 43 , 48 ]. The evidence further recommends that researchers need to understand the stage of integrating the two sets of data and the rationale for doing so. This can inform researchers regarding the best stage and appropriate ways of combining the two components of data to adequately address the research question(s).
The evidence recommended some methodological consideration in the design of mixed methods projects in mental health [ 18 , 19 , 45 ]. These issues include establishing early collaboration, becoming familiar with the topic, sharing information on the topic, negotiating any emerging problems and seeking contributions from team members. The involvement of various expertise could ensure that methodological issues are clearly identified. However, addressing such issues midway, or late through the design can negatively affect the implementation [ 45 ]. Any robust discoveries can rarely be accommodated under the existing design. Therefore, the inclusion of various methodological expertise during inception can lead to a more robust mixed-methods design which maximises the contributions of team members. Whilst fundamental and philosophical differences in qualitative and quantitative methods may not be resolved, some workable solutions can be employed, particularly if challenges are viewed as philosophical rather than personal [ 45 ]. The cultural issues can be alleviated by understanding the concepts, norms and values of the setting, further to respecting and including perspectives of the various stakeholders.
The review findings suggest that qualitative methods are relevant when conducting mental health research. The qualitative methods are mostly used where there has been limited previous research and an absence of theoretical perspectives. The approach is also used to gather initial pilot data. More importantly, the qualitative methods are relevant when we want to understand sensitive issues, especially from consumers of mental health services, where the ‘lived experience is paramount [ 19 , 28 , 44 ]. Qualitative methods can help understand the experiences of consumers in the process of treatment, as well as their therapeutic relationship with mental health professionals. The experiences of consumers from qualitative data are particularly important in developing clinical policy [ 28 ]. The review findings find two paradigms of qualitative methods are used in mental health research. These paradigms are the interpretive and critical approach [ 32 ]. The interpretive qualitative method(s) include phenomenology, ethnography and narrative approaches [ 32 , 36 ]. Conversely, critical qualitative approaches are participatory action research and emancipatory approach. The review findings suggest that these approaches to qualitative methods need critical considerations, particularly when dealing with consumers of mental health services.
The review findings identified several sampling techniques used in mental health research. Quantitative studies, usually employ probability sampling, whilst qualitative studies use non-probability sampling [ 25 , 34 ]. The most common sampling techniques for quantitative studies are multi-stage sampling, which involves systematic, stratified, random sampling and consecutive sampling. In contrast, the predominant sampling approaches for qualitative studies are purposive [ 19 , 28 , 32 , 42 , 46 ], snowballing [ 30 , 32 , 46 ] and theoretical sampling [ 31 , 32 ].
The sampling of consumers of mental health services requires some important considerations. The sampling should consider the appropriateness and adequacy of the sampling approach, diversity and variety of consumers of services, attributes such as social, or cultural experiences, shared concerns related to the study, practical and organisational skills, as well as ethical and sensitivity issues are all relevant [ 31 , 32 , 46 ]. Sampling consumers of mental health services should also consider the homogeneity and heterogeneity of consumers. However, failure to address these considerations can present difficulty in sampling and subsequently result in selection and reporting bias in mental health research.
The evidence recommends several data collection approaches in collecting data in mental health research, including focus group discussion, extended in-depth interviews, observations, field notes, Delphi data collection and quasi-statistical techniques. The focus group discussions appear as an approach widely used to collect data from consumers of mental health services [ 19 , 28 , 30 , 31 , 41 , 44 , 47 ]. The focus group discussion appears to be a significant source of obtaining information. This approach promotes the participation of consumers with severe conditions, particularly at the group level interaction. Mental health researchers are encouraged to use this approach to collect data from consumers, in order to promote group level interaction. Additionally, field notes can be used to supplement information and to more deeply analyse the interactions of consumers of mental health services. Field notes are significant when wanting to gather detailed accounts about the subjective experiences of consumers of mental health services [ 40 ]. Field notes can help researchers to capture the gestures and opinions of consumers of mental health services which cannot be covered in the audio-tape recording. Particularly, the field note is relevant to complement the richness of information collected through focus group discussion from consumers of mental health services.
Furthermore, it was found that in-depth interviews can be used to explore specific mental health issues, particularly culturally marked disorders, their personal and interpersonal significance, patient and family explanatory models, individual and family coping styles, as well as symptom symbols and protective mediators [ 19 , 30 , 34 ]. The in-depth interviews are particularly relevant if the study is interested in the lived experiences of consumers without the contamination of others in a group situation. The in-depth interviews are relevant when consumers of mental health services are uncomfortable in disclosing their confidential information in front of others [ 31 ]. The lived experience in a phenomenological context preferably allows the consumer the opportunity to express themselves anonymously without any tacit coercion created by a group context.
The review findings recommend significant factors requiring consideration when collecting data in mental health research. These considerations include building confidence and trust between the researcher and consumers [ 31 , 37 ], gaining confidence of mental health professionals who manage consumers of mental health services, seeking ethical approval from the relevant committees, meeting consumers of services before data collection as well as arranging a mutually acceptable venue for the groups and providing transport services [ 41 , 47 ]. The evidence confirms that the identification of consumers of mental health services to participate in research can be facilitated by mental health professionals. Similarly, the cultural and social differences of the consumers of mental health services need consideration when collecting data from them [ 26 , 31 ].
Moreover, our review advocates that standardised assessment instruments can be used to collect data from consumers of mental health services, particularly in quantitative data. The self-completion instruments for collecting such information can be converted to interviewer-completion instruments [ 33 , 49 ]. The interviewer can read the questions to consumers of mental health services and record their responses. It is recommended that collecting data from consumers of mental health services requires significant preparation, such as training with co-investigators and representatives from consumers of mental health services [ 25 , 30 , 33 , 34 , 35 , 39 , 49 ]. The training helps interviewers and other investigators to understand the research project, particularly translating and adapting an instrument for the study setting with the aim to achieve content, semantic, concept, criteria and technical equivalence [ 30 ]. The evidence indicates that there is a need to adequately train interviewers when preparing for fieldwork to collect data from consumers of mental health services.
The evidence provides several approaches that can be employed to ensure quality assurance in mental health research involving quantitative methods. The quality assurance approach encompasses seeking informed consent from consumers of mental health services [ 26 , 37 ], pre-testing of tools [ 25 , 49 ], minimising non-response rates and monitoring of the data collection process [ 25 , 33 , 49 ]. The quality assurance process in mental health research primarily aims to achieve the highest reliability, validity and timeliness, to improve the quality of care provided. For instance, the informed consent exposes consumers of mental health services to the aim(s), methods, anticipated benefits and potential hazards and discomforts of participating in the study. Herein, consumers of mental health services who cannot respond to the inform consent process because of the severity of their illness can have it signed by their family caregivers. The implication is that researchers should determine which category of consumers of mental health services need family caregivers involved in the consent process [ 37 ].
The review findings advises that researchers should use pre-testing to evaluate the data collection procedure on a small scale and then to subsequently make any necessary changes [ 25 ]. The pre-testing aims to help the interviewers get acquainted with the procedures and to detect any potential problems [ 49 ]. The researchers can discuss the findings of the pre-testing and then further resolve any challenges that may arise prior to the actual field work being commenced. The non-response rates in mental health research can be minimised by re-approaching consumers of mental health services who initially refuse to participate in the study.
In addition, quality assurance for qualitative data can be ensured by applying the principles of credibility, dependability, transferability, reflexivity, confirmability [ 19 , 32 ]. It was found that the credibility of qualitative research in mental health is achieved through methodological and interpretive rigour [ 32 , 37 ]. The methodological rigour for assessing credibility relates to congruence, responsiveness or sensitivity to a social context, appropriateness, adequacy and transparency. By contrast, ensuring interpretive rigour is achieved through authenticity, coherence, reciprocity, typicality and permeability of researchers’ intentions, engagement and interpretation [ 32 , 46 ].
Strengths and limitations
The evidence has several strengths and limitations that require interpretation and explanation. Firstly, we employed a systematic approach involving five stages of problem identification, literature search, data evaluation, data synthesis and presentation of results [ 21 ]. Similarly, we searched six databases and developed a data extraction form to extract information. The rigorous process employed in this study, for instance, searching databases and data extraction forms, helped to capture comprehensive information on the subject.
The integrative review has several limitations largely related to the search words, language limitations, time period and appraisal of methodological quality of included papers. In particular, the differences in key terms and words concerning methodological issues in the context of mental health research across cultures and organisational contexts may possibly have missed some relevant articles pertaining to the study. Similarly, limiting included studies to only English language articles and those published from January 2000 to July 2018 could have missed useful articles published in other languages and those published prior to 2000. The review did not assess the methodological quality of included papers using a critical appraisal tool, however, the combination of clearly articulated search methods, consultation with the research librarian, and reviewing articles with methodological experts in mental health research helped to address the limitations.
The review identified several methodological issues that need critical attention when conducting mental health research. The evidence confirms that studies that addressed methodological considerations in conducting mental health research largely focuses on qualitative studies in a transcultural setting, in addition to lessons from multi-site surveys in mental health research. Specifically, the methodological issues related to the study design, sampling, data collection processes and quality assurance are critical to the research design chosen for any particular study. The review highlighted that researchers conducting mental health research can establish early collaboration, familiarise themselves with the topic, share information on the topic, negotiate to resolve any emerging problems and seek the contribution of clinical (or researcher) team members on the ground. In addition, the recruitment of consumers of mental health services should consider the appropriateness and adequacy of sampling approaches, diversity and variety of consumers of services, their social or cultural experiences, practical and organisational skills, as well as ethical and sensitivity issues.
The evidence confirms that in an attempt to effectively recruit and collect data from consumers of mental health services, there is the need to build confidence and trust between the researcher and consumers; and to gain the confidence of mental health service providers. Furthermore, seeking ethical approval from the relevant committee, meeting with consumers of services before data collection, arranging a mutually acceptable venue for the groups, and providing transport services, are all further important considerations. The review findings establish that researchers conducting mental health research should consider several quality assurance issues. Issues such as adequate training prior to data collection, seeking informed consent from consumers of mental health services, pre-testing of tools, minimising non-response rates and monitoring of the data collection process. More specifically, quality assurance for qualitative data can be achieved by applying the principles of credibility, dependability, transferability, reflexivity, confirmability.
Based on the findings from this review, it is recommended that mental health research should adequately consider the methodological issues regarding study design, sampling, data collection procedures and quality assurance issues to effectively conduct meaningful research.
Availability of data and materials
Not applicable
Abbreviations
focus group discussions
Joanna Briggs Institute
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
National Ethics Advisory Committee. Ethical guidelines for intervention studies: revised edition. Wellington (New Zealand): Ministry of Health. 2012.
Mann C. Observational research methods. Research design II: cohort, cross sectional, and case-control studies. Emerg Med J. 2003;20(1):54–60.
Article CAS Google Scholar
DiPietro NA. Methods in epidemiology: observational study designs. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2010;30(10):973–84.
Article Google Scholar
Hong NQ, Pluyr P, Fabregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT). Canada.: Intellectual Property Office, Canada; 2018.
Creswell JW, Creswell JD. Research design: qualitative, quantitative, and mixed methods approaches: sage publications; 2017.
Google Scholar
Wisdom J, Creswell JW. Mixed methods: integrating quantitative and qualitative data collection and analysis while studying patient-centered medical home models. Rockville: Agency for Healthcare Research and Quality; 2013.
Bonita R, Beaglehole R, Kjellström T. Basic epidemiology: World Health Organization; 2006.
Centers for Disease Control Prevention [CDC]. Principles of epidemiology in public health practice: an introduction to applied epidemiology and biostatistics. Atlanta, GA: US Dept. of Health and Human Services, Centers for Disease Control and Prevention (CDC), Office of Workforce and Career Development; 2012.
Parab S, Bhalerao S. Study designs. International journal of Ayurveda research. 2010;1(2):128.
Yang W, Zilov A, Soewondo P, Bech OM, Sekkal F, Home PD. Observational studies: going beyond the boundaries of randomized controlled trials. Diabetes Res Clin Pract. 2010;88:S3–9.
Department of Family Medicine (McGill University). Mixed Methods Appraisal Tool (MMAT) – Version 2011 Canada: McGill University; 2011 [Available from: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/84371689/MMAT%202011%20criteria%20and%20tutorial%202011-06-29updated2014.08.21.pdf .
Besen J, Gan DS. A critical evaluation of clinical research study designs. J Investig Dermatol. 2014;134.
Axelrod DA, Hayward R. Nonrandomized interventional study designs (quasi-experimental designs). Clinical research methods for surgeons: Springer; 2006. p. 63–76.
Thiese MS. Observational and interventional study design types; an overview. Biochemia medica: Biochemia medica. 2014;24(2):199–210.
Velengtas P, Mohr P, Messner DA. Making informed decisions: assessing the strengths and weaknesses of study designs and analytic methods for comparative effectiveness research. National Pharmaceutical Council 2012.
Guerrera F, Renaud S, Tabbò F, Filosso PL. How to design a randomized clinical trial: tips and tricks for conduct a successful study in thoracic disease domain. Journal of thoracic disease. 2017;9(8):2692.
Bhide A, Shah PS, Acharya G. A simplified guide to randomized controlled trials. Acta Obstet Gynecol Scand. 2018;97(4):380–7.
Palinkas L, Horwitz SM, Chamberlain P, Hurlburt MS, Landsverk J. Mixed-methods designs in mental health services research: a review. Psychiatr Serv. 2011;62(3):255–63.
Palinkas L. Qualitative and mixed methods in mental health services and implementation research. J Clin Child Adolesc Psychol. 2014;43(6):851–61.
World Health Organization [WHO]. Mental health: a state of well-being 2014 [Available from: http://www.who.int/features/factfiles/mental_health/en/ .
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Hopia H, Latvala E, Liimatainen L. Reviewing the methodology of an integrative review. Scand J Caring Sci. 2016;30(4):662–9.
Pearson A, White H, Bath-Hextall F, Apostolo J, Salmond S, Kirkpatrick P. Methodology for JBI mixed methods systematic reviews. The Joanna Briggs Institute Reviewers Manual. 2014;1:5–34.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Sampling and methods of the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;109(420):8–20.
Baarnhielm S, Ekblad S. Qualitative research, culture and ethics: a case discussion. Transcultural Psychiatry. 2002;39(4):469–83.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Brown C, Lloyd K. Qualitative methods in psychiatric research. Adv Psychiatr Treat. 2001;7(5):350–6.
Davidsen AS. Phenomenological approaches in psychology and health sciences. Qual Res Psychol. 2013;10(3):318–39.
de Jong JT, Van Ommeren M. Toward a culture-informed epidemiology: combining qualitative and quantitative research in transcultural contexts. Transcultural Psychiatry. 2002;39(4):422–33.
Ekblad S, Baarnhielm S. Focus group interview research in transcultural psychiatry: reflections on research experiences. Transcultural Psychiatry. 2002;39(4):484–500.
Fossey E, Harvey C, McDermott F, Davidson L. Understanding and evaluating qualitative research. Aust N Z J Psychiatry. 2002;36(6):717–32.
Jacobi F, Wittchen H-U, Holting C, Sommer S, Lieb R, Hofler M, et al. Estimating the prevalence of mental and somatic disorders in the community: aims and methods of the German National Health Interview and examination survey. Int J Methods Psychiatr Res 2002;11(1):1–18.
Koch A, Vogel A, Holzmann M, Pfennig A, Salize HJ, Puschner B, et al. MEMENTA-‘Mental healthcare provision for adults with intellectual disability and a mental disorder’. A cross-sectional epidemiological multisite study assessing prevalence of psychiatric symptomatology, needs for care and quality of healthcare provision for adults with intellectual disability in Germany: a study protocol. BMJ Open. 2014;4(5):e004878.
Korver N, Quee PJ, Boos HB, Simons CJ, de Haan L, Investigators G. Genetic risk and outcome of psychosis (GROUP), a multi site longitudinal cohort study focused on gene–environment interaction: objectives, sample characteristics, recruitment and assessment methods. Int J Methods Psychiatr Res. 2012;21(3):205–21.
Larkin M, Watts S, Clifton E. Giving voice and making sense in interpretative phenomenological analysis. Qual Res Psychol. 2006;3(2):102–20.
Latvala E, Vuokila-Oikkonen P, Janhonen S. Videotaped recording as a method of participant observation in psychiatric nursing research. J Adv Nurs. 2000;31(5):1252–7.
Leese MN, White IR, Schene AH, Koeter MW, Ruggeri M, Gaite L. Reliability in multi-site psychiatric studies. Int J Methods Psychiatr Res. 2001;10(1):29–42.
Liu Z, Huang Y, Lv P, Zhang T, Wang H, Li Q, et al. The China mental health survey: II. Design and field procedures. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1547–57.
Montgomery P, Bailey PH. Field notes and theoretical memos in grounded theory. West J Nurs Res. 2007;29(1):65–79.
Owen S. The practical, methodological and ethical dilemmas of conducting focus groups with vulnerable clients. J Adv Nurs. 2001;36(5):652–8.
Palinkas L, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health Ment Health Serv Res. 2015;42(5):533–44.
Palinkas L, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, Landsverk J. Mixed method designs in implementation research. Adm Policy Ment Health Ment Health Serv Res. 2011;38(1):44–53.
Razafsha M, Behforuzi H, Azari H, Zhang Z, Wang KK, Kobeissy FH, et al. Qualitative versus quantitative methods in psychiatric research. Methods Mol Biol. 2012;829:49–62.
Robins CS, Ware NC, Dosreis S, Willging CE, Chung JY, Lewis-Fernández R. Dialogues on mixed-methods and mental health services research: anticipating challenges, building solutions. Psychiatr Serv. 2008;59(7):727–31.
Robinson OC. Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol. 2014;11(1):25–41.
Schilder K, Tomov T, Mladenova M, Mayeya J, Jenkins R, Gulbinat W, et al. The appropriateness and use of focus group methodology across international mental health communities. International Review of Psychiatry. 2004;16(1–2):24–30.
Schoonenboom J, Johnson RB. How to construct a mixed methods research DesignWie man ein mixed methods-Forschungs-design konstruiert. KZfSS Kölner Zeitschrift für Soziologie und Sozialpsychologie. 2017;69(2):107–31.
Yin H, Phillips MR, Wardenaar KJ, Xu G, Ormel J, Tian H, et al. The Tianjin mental health survey (TJMHS): study rationale, design and methods. Int J Methods Psychiatr Res. 2017;26(3):09.
Download references
Acknowledgements
The authors wish to thank the University of Newcastle Graduate Research and the School of Nursing and Midwifery, for the Doctoral Scholarship offered to the lead author. The authors are also grateful for the support received from Ms. Debbie Booth, the Librarian for supporting the literature search.
Author information
Authors and affiliations.
School of Nursing and Midwifery, The University of Newcastle, Callaghan, Australia
Faculty of Health and Medicine, School Nursing and Midwifery, University of Newcastle, Callaghan, Australia
Anthony Paul O’Brien
Faculty of Business and Economics, Macquarie University, North Ryde, Australia
Rebecca Mitchell
You can also search for this author in PubMed Google Scholar
Contributions
EB, APO’B, and RM conceptualized the study. EB conducted the data extraction, APO’B, and RM, conducted the second review of the extracted data. EB, working closely with APO’B and RM performed the content analysis and drafted the manuscript. EB, APO’B, and RM, reviewed and made inputs into the intellectual content and agreed on its submission for publication. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Eric Badu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Data extraction form. (DOCX 18 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Badu, E., O’Brien, A.P. & Mitchell, R. An integrative review on methodological considerations in mental health research – design, sampling, data collection procedure and quality assurance. Arch Public Health 77 , 37 (2019). https://doi.org/10.1186/s13690-019-0363-z
Download citation
Received : 13 November 2018
Accepted : 22 July 2019
Published : 10 October 2019
DOI : https://doi.org/10.1186/s13690-019-0363-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Methodological approach
- Mixed methods
- Data collection
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
New ways of working in mental health services: a qualitative, comparative case study assessing and informing the emergence of new peer worker roles in mental health services in England
Affiliations.
- 1 Division of Population Health Sciences and Education, St George’s, University of London, London, UK
- 2 Kingston Business School, Kingston University, Kingston upon Thames, UK
- 3 Joint Faculty of Health, Social Care and Education, St George’s, University of London, London, UK, and Kingston University, Kingston upon Thames, UK
- PMID: 27466663
- Bookshelf ID: NBK373837
- DOI: 10.3310/hsdr02190
Background: A variety of peer worker roles are being introduced into the mental health workforce in England, in a range of organisational contexts and service delivery settings. The evidence base demonstrating the effectiveness of peer worker-based interventions is inconclusive and largely from outside England. An emerging qualitative literature points to a range of benefits, as well as challenges to introducing the peer worker role.
Aims: In this study we aimed to test the international evidence base, and what is known generally about role adoption in public services, in a range of mental health services in England. We also aimed to develop organisational learning supporting the introduction of peer worker roles, identifying learning that was generic across mental health services and that which was specific to organisational contexts or service delivery settings.
Team: The research was undertaken by a team that comprised researchers from a range of academic and clinical disciplines, service user researchers, a peer worker, and managers and service providers in the NHS and voluntary sector. Service user researchers undertook the majority of the data collection and analysis. We adopted a coproduction approach to research, integrating the range of perspectives in the team to shape the research process and interpret our findings.
Study design: The study employed a qualitative, comparative case study design. We developed a framework, based on existing evidence and the experiential insight of the team, which conceptualised the challenges and facilitators of introducing peer worker roles into mental health services. The framework was used to inform data collection and to enable comparisons between different organisational contexts, service delivery settings and the perspectives of different stakeholders.
Settings: The study took place in 10 contrasting cases comprising mental health NHS trusts, voluntary sector service providers and partnerships between the NHS and voluntary sector or social care providers. Peer workers were employed in a variety of roles, paid and unpaid, in psychiatric inpatient settings, community mental health services and black and minority ethnic (BME)-specific services.
Participants: Participants were 89 people involved in services employing peer workers, recruited purposively in approximately equal proportion from the following stakeholder groups: service users; peer workers; (non-peer) coworkers; line managers; strategic managers; and commissioners.
Data collection: All participants completed an interview that comprised structured and open-ended questions. Structured questions addressed a number of domains identified in the existing evidence as barriers to, or facilitators of, peer worker role adoption. Open-ended questions elicited detailed data about participants’ views and experiences of peer worker roles.
Data analysis: Structured data were analysed using basic statistics to explore patterns in implementation across cases. Detailed data were analysed using a framework approach to produce a set of analytical categories. Patterns emerging in the structured analysis informed an in-depth interrogation of the detailed data set, using NVivo 9 qualitative software (QSR International Pty Ltd, Victoria, Australia) to compare data between organisational contexts, service delivery settings and stakeholder groups. Preliminary findings were refined through discussion with a range of stakeholders at feedback workshops.
Findings: Many of the facilitators of peer worker role adoption identified in the existing evidence base were also evident in mental health services in England, although there were issues around pay, leadership, shared understanding of the role, training and management where good practice was uneven. A number of examples of good practice were evident in the voluntary sector, where peer worker roles had been established for longer and organisations were more flexible. In the NHS there were a range of challenges around introducing peer worker roles into existing structures and cultures of practice. Peer workers were able to engage people with services by building relationships based on shared lived experience – the language they used was particularly important in BME-specific services – but barriers to engagement could be created where roles were overformalised.
Conclusions: Key barriers to, and facilitators of, peer worker role adoption were identified, including valuing the differential knowledge and practice that peer workers brought to the role (especially around maintaining personally, rather than professionally defined boundaries); maintaining peer identity in a role of work; changing organisational structures to support peer workers to remain well in their work; and challenging organisational cultures to empower peer workers to use their lived experience. Recommendations for future research include developing a theoretical framework articulating the change mechanisms underpinning ‘what peer workers do’, piloting and formally evaluating the effectiveness and cost-effectiveness of peer worker interventions, and mixed-method research to better understand the impact of working as a peer worker.
Funding: The National Institute for Health Research Health Services and Delivery Research programme.
Copyright © Queen’s Printer and Controller of HMSO 2014. This work was produced by Gillard et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
- Plain English summary
- Scientific summary
- Chapter 1. Introduction
- Chapter 2. Methods
- Chapter 3. Peer worker roles in mental health services in England
- Chapter 4. Peer worker roles and organisational change
- Chapter 5. Discussion and conclusions
- Acknowledgements
- Appendix 1 Part 1 interview schedule
- Appendix 2 First version of the analytical framework
- Appendix 3 Theme content tables
- Appendix 4 Part 1 analysis output
- Appendix 5 Chapter 3 analysis protocol
- Appendix 6 Part 2 interview schedules
- Appendix 7 Feedback workshop materials
- Appendix 8 Feedback workshop output
- Appendix 9 Final report: knowledge mobilisation project
- List of abbreviations
Publication types
Diane Kratt 1 *
AM J QUALITATIVE RES, Volume 2, Issue 1, pp. 22-40
https://doi.org/10.29333/ajqr/5792
OPEN ACCESS 3324 Views 6228 Downloads
Download Full Text (PDF)
Given the prevalence of children’s mental health disorders, teachers’ roles have expanded to include identifying students with mental health needs and delivering mental health interventions. However, teachers rarely receive mental health training. This study’s purpose was to explore teachers’ perspectives on an educator mental health competency framework proposed by a group of researchers using the following questions: (a) how the competencies could guide and inform their practice; (b) how the teachers would react if the competencies were adopted; and (c) what suggestions they had for improving the competencies. The participants’ responses indicated that they needed more knowledge on mental health and larger systems of support to increase their classroom effectiveness. Overall, the teachers supported the adoption of the competencies but had reservations regarding the necessary training and implementation process. Although the participants did not provide direct suggestions on revisions to the competencies, they did imply suggestions. Findings support the use of the mental health curriculum framework in the development of teacher mental health training. Several implications for practice are proposed including the addition of mental health curriculum in teacher preparation programs and the necessity for school administrators to create a school culture and infrastructure to effectively support school mental health.
Keywords: school mental health, educator competencies, teacher preparation, professional development, social emotional development
- Adelman, H. S., & Taylor, L. (2010). Mental health in schools: Engaging learners, preventing problems, and improving schools. Thousand Oaks, CA: Corwin.
- Anderson-Butcher, D. (2006). The role of the educator in early identification, referral, and linkage. In R. Waller (Ed.), Fostering child & adolescent mental health in the classroom (pp. 257-274). Thousand Oaks, CA: Sage Publications. doi:10.4135/9781452232355.n15
- Arslan, S. & Yiğit, M. F. (2016). Investigation of the Impact of Emotional Intelligence Efficacy on Teachers' Multicultural Attitudes. Journal of Education and Practice, 7(11), 147-157.
- Ball, A., Iachini, A. L., Bohnenkamp, J. H., Togno, N. M., Brown, E. L., Hoffman, J. A., & George, M. W. (2016). School mental health content in state in-service K-12 teaching standards in the United States. Teaching and Teacher Education, 60, 312-320. doi:10.1016/j.tate.2016.08.020
- Bishop, D. C., Giles, S. M., & Bryant, K. S. (2005). Teacher receptiveness toward web-based training and support. Teaching and Teacher Education, 21(1), 3-14. doi:10.1016/j.tate.2004.11.002
- Bradshaw, C. P., Bottiani, J. H., Osher, D., & Sugai, G. (2014). The integration of positive behavioral interventions and supports and social and emotional learning. In M. Weist, N. Lever, C. Bradshaw, & J. Owens (Eds.), Handbook of school mental health (pp. 101- 118). New York, NY: Springer.
- Cammack, N. L., Brandt, N. E., Slade, E., Lever, N. A., & Stephan, S. (2014). Funding expanded school mental health programs. In M. Weist, N. Lever, C. Bradshaw, & J. Owens (Eds.), Handbook of school mental health (pp. 17-30). New York, NY: Springer.
- Carothers, D. & Parfitt, C. (2017). Disability or Language Difference: How Do We Decide? American Journal of Qualitative Research, 1(1), 1-12.
- Climie, E. A. (2015). Canadian children’s mental health building capacity in school-based intervention. Intervention in School and Clinic, 51(2), 122-125.
- Creswell, J.W. (2013). Qualitative inquiry & research design: Choosing among five approaches (3rd ed.). Los Angeles, CA: Sage Publications.
- Deniz, M., & Ersoy, E. (2016). Examining the Relationship of Social Skills, Problem Solving and Bullying in Adolescents. International Online Journal of Educational Sciences, 8(1), 1 -7.
- Ekornes, S. (2017). Teacher stress related to student mental health promotion: The match between perceived demands and competence to help students with mental health problems. Scandinavian Journal of Educational Research, 61(3), 333-353. doi:10.1080/00313831.2016.1147068
- Elias, M. J., Zins J. E., Graczyk, P. A., & Weissberg, R. P. (2003). Implementation, sustainability, and scaling up of social-emotional and academic innovations in public schools. School Psychology Review, 32(3), 303-319.
- Ersoy, E. (2015). Assessment of Adolescent Perceptions on Parental Attitudes on Different Variables. Journal of Education and Training Studies, 3(5), 165-176.
- Ersoy, E., & Ugur, H. (2015). The Relationship between Students’ Self-esteem and Parental Attitudes in Turkish Society. The Anthropologist, 21(1-2), 112-119.
- Ersoy, E., & Deniz, M. E. (2016). Psychometric Properties of the Gifted Students' Coping with Anger and Decision Making Skills Scale. Journal of Education and Practice, 7(15), 121-128.
- Franklin, C. G. S., Kim, J. S., Ryan, T. N., Kelly, M. S., & Montgomery, K. L. (2012). Teacher involvement in school mental health interventions: A systematic review. Children and Youth Services Review, 34(5), 973-982. doi:10.1016/j.childyouth.2012.01.027
- Gray, D. E., Ilse, P., & Watson, S. (2011). Spanning the HRD academic-practitioner divide: Bridging the gap through mode 2 research. Journal of European Industrial Training, 35(3), 247-263. doi:10.1108/03090591111120403
- Gore, J. M. & Gitlin, A. D. (2004). [RE]visioning the academic-teacher divide: Power and knowledge in the educational community. Teachers and Teaching, 10(1), 35-58. doi:10.1080/13540600320000170918
- Graham, A., Phelps, R., Maddison, C., & Fitzgerald, R. (2011). Supporting children’s mental health in schools: Teacher views. Teachers and Teaching: Theory and Practice, 17(4), 479-496.
- Greenglass, E. R., & Burke, R. J. (2003). Teacher Stress. In M. F. Dollard, A. H. Winefield, & H. Winefield (Eds.), Occupational Stress in the Service Professions (pp. 213-236). London: Taylor & Francis. doi:10.1201/9780203422809.ch8
- Han, S. S., & Weiss B. (2005). Sustainability of teacher implementation of school-based mental health programs. Journal of Abnormal Child Psychology, 33(6), 665-679. doi:10.1007/s10802-005-7646-2 Brooks, J. G. (1999, December 30). In search of understanding: The case for constructivist classrooms. [Review of the book, by C. Halpern]. American Journal of Qualitative Research, 1(1), 32-36.
- Hoagwood, K. E., Cavaleri, M. A., Olin, S. S., Burns, B. J., Slaton, E., Gruttadaro, D. & Hughes, R. (2010). Family support in children’s mental health: A review and synthesis. Clinical Child and Family Psychology Review, 13(1), 1-45.
- Jorm, A. F., Kitchener, B. A., Sawyer, M. G., Scales, H., & Cvetkovski, S. (2010). Mental health first aid training for high school teachers: A cluster randomized trial. BMC Psychiatry, 10(51). doi:10.1186/1471-244X-10-51
- Knowles, M. S. (1984). Andragogy in action: Applying modern principles of adult learning. San Francisco, CA: Jossey-Bass.
- Koller, J. R., Osterlind, S., Paris, K., & Weston, K. J. (2004). Differences between novice and expert teachers’ undergraduate preparation and ratings of importance in the area of children’s mental health. International Journal of Mental Health Promotion, 6(2), 40-45.
- Lafee, S. (2013). The school’s role in students’ mental health. School Administrator, 7(70), 24-30.
- Mazzer, K. R. & Rickwood, D. J. (2014). Teachers’ role breadth and perceived efficacy in supporting student mental health. Advances in School Mental Health Promotion, 8(1), 29-41. doi:10.1080/1754730X.2014.978119
- McDaniel, H. L., Schiele, B. E., Taylor, L. K., Haak, J., & Weist, M. D. (2014). Strengthening components and processes of family involvement in school mental health. In M. Weist, N. Lever, C. Bradshaw, & J. Owens (Eds.), Handbook of school mental health (pp. 195-207). New York, NY: Springer. doi:10.1007/978-1-4614-7624-5_15
- McGorry, P., Bates, T., & Birchwood, M. (2013). Designing youth mental health services for the 21st century: Examples from Australia, Ireland and the UK. The British Journal of Psychiatry, 202(54), 30–35. doi:10.1192/bjp.bp.112.119214
- Meldrum, L., Venn, D., & Kutcher, S. (2009). Mental health in schools: How teachers have the power to make a difference. Health & Learning Magazine, 8, 3-5.
- National Center for Educational Statistics. (2014). Fast Facts. Washington, DC: Author. Retrieved from http://nces.ed.gov/fastfacts/display.asp?id=372
- National Research Council and Institute of Medicine. (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. M.E. O’Connell, T. Boat, & K.E. Warner (Eds.), Board of Children, Youth, and Families, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press.
- Nellis, L. M. (2012). Maximizing the effectiveness of building teams in response to intervention implementation. Psychology in the Schools, 49(3), 245-256. doi:10.1002/pits.21594
- New Freedom Commission on Mental Health. (2003). Achieving the promise: Transforming mental health care in America final report (DHHS Pub. No. SMA-03-3832). Rockville, MD: U.S. Department of Health and Human Services.
- O’Connell, M. E., Boat, T., & Warner, K. E. (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Washington, DC: Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults: Research Advances and Promising Interventions; Institute of Medicine; National Research Council, The National Academies Press.
- Paternite, C. E., & Johnston, T. C. (2005). Rationale and strategies for central involvement of educators in effective school-based mental health programs. Journal of Youth and Adolescence, 14(1), 41-49. doi:10.1007/s10964-005-1335-x
- Phillippo, K. L. & Kelly, M. S. (2014). On the fault line: A qualitative exploration of high school teachers’ involvement with student mental health issues. School Mental Health, 6(3). doi:10.1007/s12310-013-9113-5
- Rossen, E., & Cowan, K.C. (2014). Improving mental health in schools. Phi Delta Kappan, 96(4), 8-13. doi:10.1177/0031721714561438
- Rothi, D. M., Leavey, G., & Best, R. (2008). On the front-line: Teachers as active observers of pupils’ mental health. Teaching and Teacher Education, 24(5), 1217-1231. doi:10.1016/j.tate.2007.09.011
- Sawyer, M. G., Arney, F. M., Baghurst, P. A., Clark, J. J., Graetz, B. W., Kosky, R. J., Nurcombe, B., Patton, G. C., Prior, M. R., Raphael, B., Rey, J. M., Whaites, L. C., & Zubrick, S. R. (2001). The mental health of young people in Australia: key findings from the child and adolescent component of the national survey of mental health and well-being. Australian and New Zealand Journal of Psychiatry, 35(6), 806–814. doi:10.1046/j.1440-1614.2001.00964.x
- Schonert-Reichl, K. A. (2017). Social and emotional learning and teachers. The Future of Children, 27(1), 137-155.
- Shernoff, E.S., Frazier, S.L., Marinez-Lora, A.M., Lakind, D., Atkins, M.S., Jakobsons, L., Hamre, B.K., Bhaumik, D.K., Parker-Katz, M., Neal, J.W., Smylie, M.A., & Patel, D.A. (2016). Expanding the role of school psychologists to support early career teachers: A mixed-method study. School Psychology Review, 45(2), 226-249. doi:10.17105/SPR45-2.226-249
- Stake, R.E. (1995). The art of case study research. Thousand Oaks, CA: Sage Publications.
- Volk, A. A., Craig, W., Boyce, W., & King, M. (2006). Perceptions of parents, mental health, and school amongst Canadian adolescents from the provinces and the northern territories. Canadian Journal of School Psychology, 21(1-2), 33-46.
- Walter, H. J., Gouze, K., & Lim, K. G. (2006). Teachers’ beliefs about mental health needs in inner city elementary schools. Journal of the American Academy of Child and Adolescent Psychiatry, 45(1), 61-68.
- Waxman, R. P., Weist, M. D., & Benson, D. M. (1999). Toward collaboration in the growing education-mental health interface. Clinical Psychology Review, 19(2), 239-253. doi:10.1016/S0272-7358(98)00072-5
- Weist, M. D., & Evans, S. W. (2005). Expanded school mental health: Challenges and opportunities in an emerging field. Journal of Youth and Adolescence, 34(1), 3–6. doi:10.1007/s10964-005-1330-2
- Weist, M. D., Lever, N. A., Bradshaw, C. P., & Owens, J. S. (2014). Further advancing the field of school mental health. In M. Weist, N. Lever, C. Bradshaw, & J. Owens (Eds.), Handbook of school mental health (pp. 1-14). New York, NY: Springer. doi:10.1007/978-1-4614-7624-5_1
- Weist, M. D., Mellin, E. A., Chambers, K. L., Lever, N. A., Haber, D., & Blaber, C. (2012). Challenges to collaboration in school mental health and strategies for overcoming them. Journal of School Mental Health, 82(2), 97-105. doi:10.1111/j.1746-1561.2011.00672.x
- Weston, K. J., Anderson-Butcher, D., & Burke, R. W. (2008). Developing a comprehensive curriculum framework for teacher preparation in expanded school mental health. Advances in School Mental Health Promotion, 1(4), 25-36. doi:10.1080/1754730X.2008.9715737
- Weyns, T., Verschueren, K., Leflot, G., Onghena, P., Wouters, S., & Colpin, H. (2017). The role of teacher behavior in children's relational aggression development: A five-wave longitudinal study. Journal of School Psychology, 64, 17-27. doi:10.1016/j.jsp.2017.04.008
- Whitley, J., Smith, J. D., & Vaillancourt, T. (2012). Promoting mental health literacy among educators: Critical in school-based prevention and intervention. Canadian Journal of School Psychology, 28(1), 56-70. doi:10.1177/0829573512468852
- Williams, J. H., Horvath, V. E., Wei, H., Van Dorn, R. A., & Jonson-Reid, M. (2007). Teacher’s perspectives of children’s mental health service needs in urban elementary schools. Children & Schools, 29(2), 95-107.
- World Health Organization. (2003). Investing in mental health [Report]. Geneva, Switzerland: Author. Retrieved from www.who.int/mental_health/en/investing_in_mnh_final.pdf
- Yigit, I. H., & Tatch, A. (2017). Syrian refugees and Americans: Perceptions, attitudes and insights. American Journal of Qualitative Research, 1(1), 13-31.
- Open access
- Published: 10 April 2024
“So at least now I know how to deal with things myself, what I can do if it gets really bad again”—experiences with a long-term cross-sectoral advocacy care and case management for severe multiple sclerosis: a qualitative study
- Anne Müller ORCID: orcid.org/0000-0002-2456-2492 1 ,
- Fabian Hebben ORCID: orcid.org/0009-0003-6401-3433 1 ,
- Kim Dillen 1 ,
- Veronika Dunkl 1 ,
- Yasemin Goereci 2 ,
- Raymond Voltz 1 , 3 , 4 ,
- Peter Löcherbach 5 ,
- Clemens Warnke ORCID: orcid.org/0000-0002-3510-9255 2 &
- Heidrun Golla ORCID: orcid.org/0000-0002-4403-630X 1
on behalf of the COCOS-MS trial group represented by Martin Hellmich
BMC Health Services Research volume 24 , Article number: 453 ( 2024 ) Cite this article
159 Accesses
Metrics details
Persons with severe Multiple Sclerosis (PwsMS) face complex needs and daily limitations that make it challenging to receive optimal care. The implementation and coordination of health care, social services, and support in financial affairs can be particularly time consuming and burdensome for both PwsMS and caregivers. Care and case management (CCM) helps ensure optimal individual care as well as care at a higher-level. The goal of the current qualitative study was to determine the experiences of PwsMS, caregivers and health care specialists (HCSs) with the CCM.
In the current qualitative sub study, as part of a larger trial, in-depth semi-structured interviews with PwsMS, caregivers and HCSs who had been in contact with the CCM were conducted between 02/2022 and 01/2023. Data was transcribed, pseudonymized, tested for saturation and analyzed using structuring content analysis according to Kuckartz. Sociodemographic and interview characteristics were analyzed descriptively.
Thirteen PwsMS, 12 caregivers and 10 HCSs completed interviews. Main categories of CCM functions were derived deductively: (1) gatekeeper function, (2) broker function, (3) advocacy function, (4) outlook on CCM in standard care. Subcategories were then derived inductively from the interview material. 852 segments were coded. Participants appreciated the CCM as a continuous and objective contact person, a person of trust (92 codes), a competent source of information and advice (on MS) (68 codes) and comprehensive cross-insurance support (128 codes), relieving and supporting PwsMS, their caregivers and HCSs (67 codes).
Conclusions
Through the cross-sectoral continuous support in health-related, social, financial and everyday bureaucratic matters, the CCM provides comprehensive and overriding support and relief for PwsMS, caregivers and HCSs. This intervention bears the potential to be fine-tuned and applied to similar complex patient groups.
Trial registration
The study was approved by the Ethics Committee of the University of Cologne (#20–1436), registered at the German Register for Clinical Studies (DRKS00022771) and in accordance with the Declaration of Helsinki.
Peer Review reports
Introduction
Multiple sclerosis (MS) is the most frequent and incurable chronic inflammatory and degenerative disease of the central nervous system (CNS). Illness awareness and the number of specialized MS clinics have increased since the 1990s, paralleled by the increased availability of disease-modifying therapies [ 1 ]. There are attempts in the literature for the definition of severe MS [ 2 , 3 ]. These include a high EDSS (Expanded disability Status Scale [ 4 ]) of ≥ 6, which we took into account in our study. There are also other factors to consider, such as a highly active disease course with complex therapies that are associated with side effects. These persons are (still) less disabled, but may feel overwhelmed with regard to therapy, side effects and risk monitoring of therapies [ 5 , 6 ].
Persons with severe MS (PwsMS) develop individual disease trajectories marked by a spectrum of heterogeneous symptoms, functional limitations, and uncertainties [ 7 , 8 ] manifesting individually and unpredictably [ 9 ]. This variability can lead to irreversible physical and mental impairment culminating in complex needs and daily challenges, particularly for those with progressive and severe MS [ 5 , 10 , 11 ]. Such challenges span the spectrum from reorganizing biographical continuity and organizing care and everyday live, to monitoring disease-specific therapies and integrating palliative and hospice care [ 5 , 10 ]. Moreover, severe MS exerts a profound of social and economic impact [ 9 , 12 , 13 , 14 ]. PwsMS and their caregivers (defined in this manuscript as relatives or closely related individuals directly involved in patients’ care) often find themselves grappling with overwhelming challenges. The process of organizing and coordinating optimal care becomes demanding, as they contend with the perceived unmanageability of searching for, implementing and coordinating health care and social services [ 5 , 15 , 16 , 17 ].
Case management (CM) proved to have a positive effect on patients with neurological disorders and/or patients with palliative care needs [ 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 ]. However, a focus on severe MS has been missed so far Case managers primarily function as: (1) gatekeeper involving the allocation of necessary and available resources to a case, ensuring the equitable distribution of resources; as (2) broker assisting clients in pursuing their interests, requiring negotiation to provide individualized assistance that aligns as closely as possible with individual needs and (3) advocate working to enhance clients’ individual autonomy, to advocate for essential care offers, and to identify gaps in care [ 25 , 26 , 27 , 28 , 29 ].
Difficulties in understanding, acting, and making decisions regarding health care-related aspects (health literacy) poses a significant challenge for 54% of the German population [ 30 ]. Additionally acting on a superordinate level as an overarching link, a care and case management (CCM) tries to reduce disintegration in the social and health care system [ 31 , 32 ]. Our hypothesis is that a CCM allows PwsMS and their caregivers to regain time and resources outside of disease management and to facilitate the recovery and establishment of biographical continuity that might be disrupted due to severe MS [ 33 , 34 ].
Health care specialists (HCSs) often perceive their work with numerous time and economic constraints, especially when treating complex and severely ill individuals like PwsMS and often have concerns about being blamed by patients when expectations could not be met [ 35 , 36 ]. Our hypothesis is that the CCM will help to reduce time constraints and free up resources for specialized tasks.
To the best of our knowledge there is no long-term cross-sectoral and outreaching authority or service dedicated to assisting in the organization and coordination of the complex care concerns of PwsMS within the framework of standard care addressing needs in health, social, financial, every day and bureaucratic aspects. While some studies have attempted to design and test care programs for persons with MS (PwMS), severely affected individuals were often not included [ 37 , 38 , 39 ]. They often remain overlooked by existing health and social care structures [ 5 , 9 , 15 ].
The COCOS-MS trial developed and applied a long-term cross-sectoral CCM intervention consisting of weekly telephone contacts and monthly re-assessments with PwsMS and caregivers, aiming to provide optimal care. Their problems, resources and (unmet) needs were assessed holistically including physical health, mental health, self-sufficiency and social situation and participation. Based on assessed (unmet) needs, individual care plans with individual actions and goals were developed and constantly adapted during the CCM intervention. Contacts with HCSs were established to ensure optimal care. The CCM intervention was structured through and documented in a CCM manual designed for the trial [ 40 , 41 ].
Our aim was to find out how PwsMS, caregivers and HCSs experienced the cross-sectoral long-term, outreaching patient advocacy CCM.
This study is part of a larger phase II, randomized, controlled clinical trial “Communication, Coordination and Security for people with severe Multiple Sclerosis (COCOS-MS)” [ 41 ]. This explorative clinical trial, employing a mixed-method design, incorporates a qualitative study component with PwsMS, caregivers and HCSs to enrich the findings of the quantitative data. This manuscript focuses on the qualitative data collected between February 2022 and January 2023, following the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines [ 42 ].
Research team
Three trained authors AM, KD and FH (AM, female, research associate, M.A. degree in Rehabilitation Sciences; KD, female, researcher, Dr. rer. medic.; FH, male, research assistant, B.Sc. degree in Health Care Management), who had no prior relationship with patients, caregivers or HCSs conducted qualitative interviews. A research team, consisting of clinical experts and health services researchers, discussed the development of the interview guides and the finalized category system.
Theoretical framework
Interview data was analyzed with the structuring content analysis according to Kuckartz. This method enables a deductive structuring of interview material, as well as the integration of new aspects found in the interview material through the inductive addition of categories in an iterative analysis process [ 43 ].
Sociodemographic and interview characteristics were analyzed descriptively (mean, median, range, SD). PwsMS, caregivers and HCSs were contacted by the authors AM, KD or FH via telephone or e-mail after providing full written informed consent. Participants had the option to choose between online interviews conducted via the GoToMeeting 10.19.0® Software or face-to-face. Peasgood et al. (2023) found no significant differences in understanding questions, engagement or concentration between face-to-face and online interviews [ 44 , 45 ]. Digital assessments were familiar to participants due to pandemic-related adjustments within the trial.
Out of 14 PwsMS and 14 caregivers who were approached to participate in interviews, three declined to complete interviews, resulting in 13 PwsMS (5 male, 8 female) and 12 caregiver (7 male, 5 female) interviews, respectively (see Fig. 1 ). Thirty-one HCSs were contacted of whom ten (2 male, 8 female) agreed to be interviewed (see Fig. 2 ).
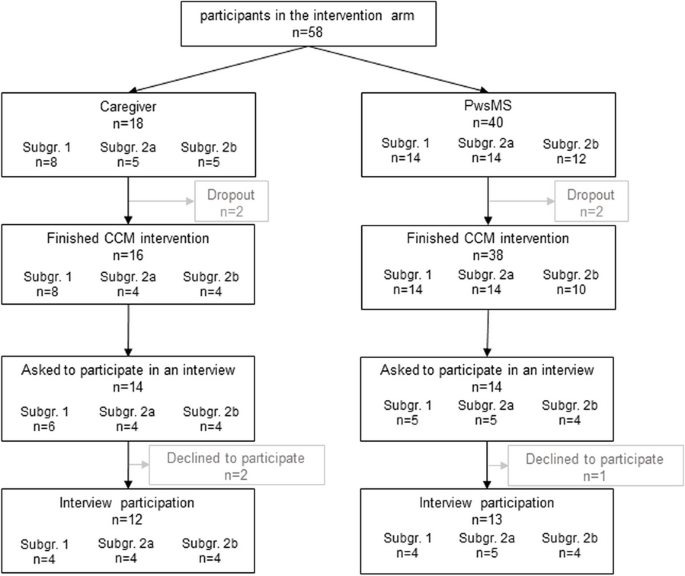
Flowchart of PwsMS and caregiver participation in the intervention group of the COCOS-MS trial. Patients could participate with and without a respective caregiver taking part in the trial. Therefore, number of caregivers does not correspond to patients. For detailed inclusion criteria see also Table 1 in Golla et al. [ 41 ]
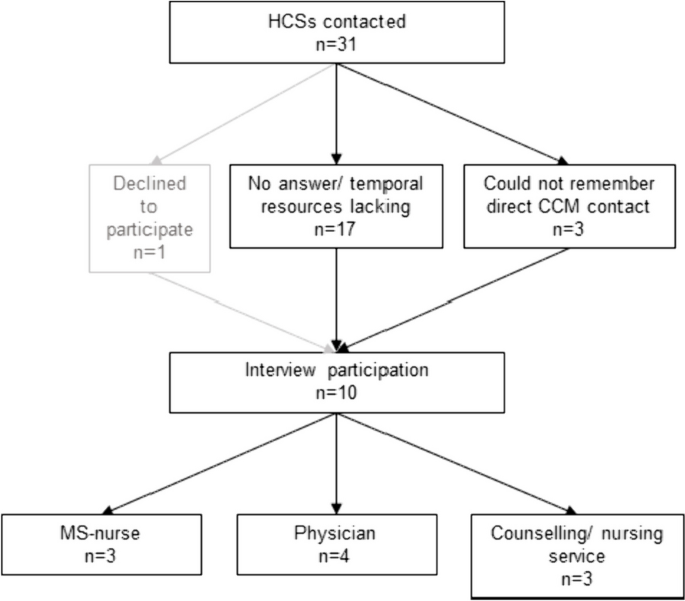
Flowchart of HCSs interview participation
Setting and data collection
Interviews were carried out where participants preferred, e.g. at home, workplace, online, and no third person being present. In total, we conducted 35 interviews whereof 7 interviews face-to-face (3 PwsMS, 3 caregivers, 1 HCS).
The research team developed a topic guide which was meticulously discussed with research and clinical staff to enhance credibility. It included relevant aspects for the evaluation of the CCM (see Tables 1 and 2 , for detailed topic guides see Supplementary Material ). Patient and caregiver characteristics (covering age, sex, marital status, living situation, EDSS (patients only), subgroup) were collected during the first assessment of the COCOS-MS trial and HCSs characteristics (age, sex, profession) as well as interview information (length and setting) were collected during the interviews. The interview guides developed for this study addressed consistent aspects both for PwsMS and caregivers (see Supplementary Material ):
For HCSs it contained the following guides:
Probing questions were asked to get more specific and in-depth information. Interviews were carried out once and recorded using a recording device or the recording function of the GoToMeeting 10.19.0® Software. Data were pseudonymized (including sensitive information, such as personal names, dates of birth, or addresses), audio files were safely stored in a data protection folder. The interview duration ranged from 11 to 56 min (mean: 23.9 min, SD: 11.1 min). Interviews were continued until we found that data saturation was reached. Audio recordings were transcribed verbatim by an external source and not returned to participants.
Data analysis
Two coders (AM, FH) coded the interviews. Initially, the first author (AM) thoroughly reviewed the transcripts to gain a sense of the interview material. Using the topic guide and literature, she deductively developed a category system based on the primary functions of CM [ 25 , 26 , 27 , 28 , 29 ]. Three interviews were coded repeatedly for piloting, and inductive subcategories were added when new themes emerged in the interview material. This category system proved suitable for the interview material. The second coder (FH) familiarized himself with the interview material and category system. Both coders (AM, FH) independently coded all interviews, engaging in discussions and adjusting codes iteratively. The finalized category system was discussed and consolidated in a research workshop and within the COCOS-MS trial group and finally we reached an intercoder agreement of 90% between the two coders AM and FH, computed by the MAXQDA Standard 2022® software.
We analyzed sociodemographic and interview characteristics using IBM SPSS Statistics 27® and Excel 2016®. Transcripts were managed and analyzed using MAXQDA Standard 2022®.
Participants were provided with oral and written information about the trial and gave written informed consent. Ethical approvals were obtained from the Ethics Committee of the University of Cologne (#20–1436). The trial is registered in the German Register for Clinical Studies (DRKS) (DRKS00022771) and is conducted under the Declaration of Helsinki.
Characteristics of participants and interviews
PwsMS participating in an interview were mainly German (84.6%), had a mean EDSS of 6.8 (range: 6–8) and MS for 13.5 years (median: 14; SD: 8.1). For detailed characteristics see Table 3 .
Most of the interviewed caregivers (9 caregivers) were the partners of the PwsMS with whom they lived in the same household. For further details see Table 3 .
HCSs involved in the study comprised various professions, including MS-nurse (3), neurologist (2), general physician with further training in palliative care (1), physician with further training in palliative care and pain therapist (1), housing counselling service (1), outpatient nursing service manager (1), participation counselling service (1).
Structuring qualitative content analysis
The experiences of PwsMS, caregivers and HCSs were a priori deductively assigned to four main categories: (1) gatekeeper function, (2) broker function, (3) advocacy function [ 25 , 26 , 27 , 28 , 29 ] and (4) Outlook on CCM in standard care, whereas the subcategories were developed inductively (see Fig. 3 ).
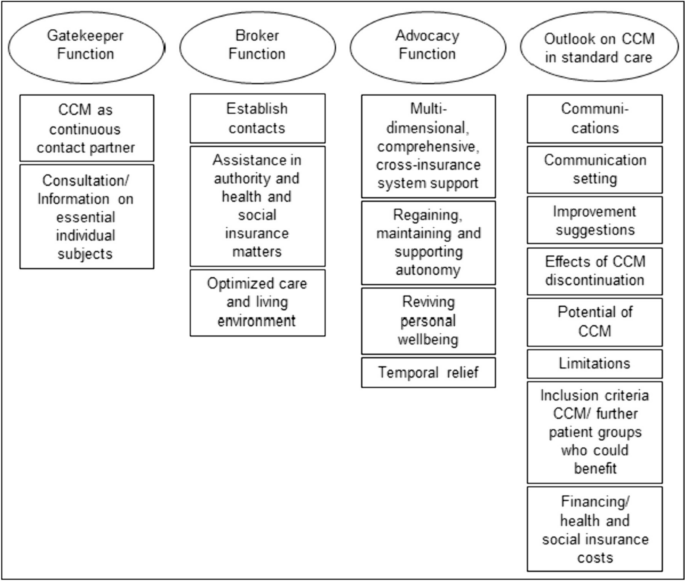
Category system including main and subcategories of the qualitative thematic content analysis
The most extensive category, housing the highest number of codes and subcodes, was the “ Outlook on CCM in standard care ” (281 codes). Following this, the category “ Advocacy Function ” contained 261 codes. The “ Broker Function ” (150 codes) and the “ Gatekeeper Function ” (160 codes) constituted two smaller categories. The majority of codes was identified in the caregivers’ interviews, followed by those of PwsMS (see Table 4 ). Illustrative quotes for each category and subcategory can be found in Table 5 .
Persons with severe multiple sclerosis
In the gatekeeper function (59 codes), PwsMS particularly valued the CCM as a continuous contact person . They appreciated the CCM as a person of trust who was reliably accessible throughout the intervention period. This aspect, with 41 codes, held significant importance for PwsMS.
Within the broker function (44 codes), establishing contact was most important for PwsMS (22 codes). This involved the CCM as successfully connecting PwsMS and caregivers with physicians and therapists, as well as coordinating and arranging medical appointments, which were highly valued. Assistance in authority and health and social insurance matters (10 codes) was another subcategory, where the CCM encompassed support in communication with health insurance companies, such as improving the level of care, assisting with retirement pension applications, and facilitating rehabilitation program applications. Optimized care (12 codes) resulted in improved living conditions and the provision of assistive devices through the CCM intervention.
The advocacy function (103 codes) emerged as the most critical aspect for PwsMS, representing the core of the category system. PwsMS experienced multidimensional, comprehensive, cross-insurance system support from the CCM. This category, with 43 statements, was the largest within all subcategories. PwsMS described the CCM as addressing their concerns, providing help, and assisting with the challenges posed by the illness in everyday life. The second-largest subcategory, regaining, maintaining and supporting autonomy (25 codes), highlighted the CCM’s role in supporting self-sufficiency and independence. Reviving personal wellbeing (17 codes) involved PwsMSs’ needs of regaining positive feelings, improved quality of life, and a sense of support and acceptance, which could be improved by the CCM. Temporal relief (18 codes) was reported, with the CCM intervention taking over or reducing tasks.
Within the outlook on CCM in standard care (84 codes), eight subcategories were identified. Communications was described as friendly and open (9 codes), with the setting of communication (29 codes) including the frequency of contacts deemed appropriate by the interviewed PwsMS, who preferred face-to-face contact over virtual or telephone interactions. Improvement suggestions for CCM (10 codes) predominantly revolved around the desire for the continuation of the CCM beyond the trial, expressing intense satisfaction with the CCM contact person and program. PwsMS rarely wished for better cooperation with the CCM. With respect to limitations (7 codes), PwsMS distinguished between individual limitations (e.g. when not feeling ready for using a wheelchair) and overriding structural limitations (e.g. unsuccessful search for an accessible apartment despite CCM support). Some PwsMS mentioned needing the CCM earlier in the course of the disease and believed it would beneficial for anyone with a chronic illness (6 codes).
In the gatekeeper function (75 codes), caregivers highly valued the CCM as a continuous contact partner (33 codes). More frequently than among the PwsMS interviewed, caregivers valued the CCM as a source of consultation/ information on essential individual subjects (42 codes). The need for basic information about the illness, its potential course, treatment and therapy options, possible supportive equipment, and basic medical advice/ information could be met by the CCM.
Within the broker function (63 codes), caregivers primarily experienced the subcategory establish contacts (24 codes). They found the CCM as helpful in establishing and managing contact with physicians, therapists and especially with health insurance companies. In the subcategory assistance in authority and health and social insurance matters (22 codes), caregivers highlighted similar aspects as the PwsMS interviewed. However, there was a particular emphasis on assistance with patients' retirement matters. Caregivers also valued the optimization of patients’ care and living environment (17 codes) in various life areas during the CCM intervention, including improved access to assistive devices, home modification, and involvement of a household support and/ or nursing services.
The advocacy function, with 115 codes, was by far the broadest category . The subcategory multidimensional, comprehensive, cross-insurance system support represented the largest subcategory of caregivers, with 70 statements. In summary, caregivers felt supported by the CCM in all domains of life. Regaining, maintaining and supporting autonomy (11 codes) and reviving personal wellbeing (8 codes) in the form of an improved quality of life played a role not only for patients but also for caregivers, albeit to a lower extend. Caregivers experienced temporal relief (26 codes) as the CCM undertook a wide range of organizational tasks, freeing up more needed resources for their own interests.
For the Outlook on CCM in standard care , caregivers provided various suggestions (81 codes). Similar to PwsMS, caregivers felt that setting (home based face-to-face, telephone, virtual) and frequency of contact were appropriate (10 codes, communication setting ) and communications (7 codes) were recognized as open and friendly. However, to avoid conflicts between caregiver and PwsMS, caregivers preferred meeting the CCM separately from the PwsMS in the future. Some caregivers wished the CCM to specify all services it might offer at the beginning, while others emphasized not wanting this. Like PwsMS, caregivers criticized the CCM intervention being (trial-related) limited to one year, regardless of whether further support was needed or processes being incomplete (13 codes, improvement suggestions ). After the CCM intervention time had expired, the continuous contact person and assistance were missed and new problems had arisen and had to be managed with their own resources again (9 codes, effects of CCM discontinuation ), which was perceived as an exhausting or unsolvable endeavor. Caregivers identified analogous limitations (8 codes), both individual and structural. However, the largest subcategory, was the experienced potential of CCM (27 codes), reflected in extremely high satisfaction with the CCM intervention. Like PwsMS, caregivers regarded severe chronically ill persons in general as target groups for a CCM (7 codes) and would implement it even earlier, starting from the time of diagnosis. They considered a CCM to be particularly helpful for patients without caregivers or for caregivers with limited (time) resources, as it was true for most caregivers.
Health care specialists
In the gatekeeper function (26 codes) HCSs particularly valued the CCM as a continuous contact partner (18 codes). They primarily described their valuable collaboration with the CCM, emphasizing professional exchange between the CCM and HCSs.
Within the broker function (43 codes), the CCM was seen as a connecting link between patients and HCSs, frequently establishing contacts (18 codes). This not only improved optimal care on an individual patient level (case management) but also at a higher, superordinate care level (care management). HCSs appreciated the optimized care and living environment (18 codes) for PwsMS, including improved medical and therapeutic access and the introduction of new assistive devices. The CCM was also recognized as providing assistance in authority and health and social matters (7 codes) for PwsMS and their caregivers.
In the advocacy function (43 codes), HCSs primarily reported temporal relief through CCM intervention (23 codes). They experienced this relief, especially as the CCM provided multidimensional, comprehensive, and cross-insurance system support (15 codes) for PwsMS and their caregivers. Through this support, HCSs felt relieved from time intensive responsibilities that may not fall within their area of expertise, freeing up more time resources for their actual professional tasks.
The largest category within the HCSs interviews was the outlook on CCM in standard care (116 codes). In the largest subcategory, HCSs made suggestions for further patient groups who could benefit (38 codes) from a CCM. Chronic neurological diseases like neurodegenerative diseases (e.g. amyotrophic lateral sclerosis), typical and atypical Parkinson syndromes were mentioned. HCSs considered the enrollment of the CCM directly after the diagnosis of these complex chronic diseases. Additionally, chronic progressive diseases in general or oncological diseases, which may also run chronically, were regarded worthwhile for this approach. HCSs also provided suggestions regarding improvement (21 codes). They wished e.g. for information or contact when patients were enrolled to the CCM, regular updates, exchange and collaborative effort. On the other hand, HCSs reported, that their suggestions for improvement would hardly be feasible due to their limited time resources. Similar to patients and caregivers, HCSs experienced structural limits (13 codes), which a CCM could not exceed due to overriding structural limitations (e.g. insufficient supply of (household) aids, lack of outreach services like psychotherapists, and long processing times on health and pension insurers' side). HCSs were also asked about their opinions on financial resources (14 codes) of a CCM in standard care. All interviewed HCSs agreed that CCM would initially cause more costs for health and social insurers, but they were convinced of cost savings in the long run. HCSs particularly perceived the potential of the CCM (20 codes) through the feedback of PwsMS, highlighting the trustful relationship enabling individualized help for PwsMS and their caregivers.
Persons with severe multiple sclerosis and their caregivers
The long-term cross-sectoral CCM intervention implemented in the COCOS-MS trial addressed significant unmet needs of PwsMS and their caregivers which previous research revealed as burdensome and hardly or even not possible to improve without assistance [ 5 , 6 , 9 , 10 , 33 , 35 , 46 ]. Notably, the CCM service met the need for a reliable, continuous contact partner, guiding patients through the complexities of regulations, authorities and the insurance system. Both, PwsMS and their caregivers highly valued the professional, objective perspective provided by the CCM, recognizing it as a source of relief, support and improved care in line with previous studies [ 37 , 47 ]. Caregivers emphasized the CCM’s competence in offering concrete assistance and information on caregiving and the fundamentals of MS, including bureaucratic, authority and insurances matters. On the other hand, PwsMS particularly appreciated the CCMs external reflective and advisory function, along with empathic social support tailored to their individual concerns. Above all, the continuous partnership of trust, available irrespective of the care sector, was a key aspect that both PwsMS and their caregivers highlighted. This consistent support was identified as one of the main components in the care of PwsMS in previous studies [ 5 , 33 , 35 ].
As the health literacy is inadequate or problematic for 54% of the German population and disintegration in the health and social care system is high [ 30 , 31 , 32 ], the CCM approach serves to enhance health literacy and reduce disintegration of PwsMS and their caregivers by providing cross-insurance navigational guidance in the German health and social insurance sector on a superordinate level. Simultaneously PwsMS and caregivers experienced relief and gained more (time) resources for all areas of life outside of the disease and its management, including own interests and establishing biographical continuity. This empowerment enables patients to find a sense of purpose beyond their illness, regain autonomy, and enhance social participation, reducing the feeling of being a burden to those closest to them. Such feelings are often experienced as burdensome and shameful by PwsMS [ 6 , 48 , 49 , 50 ]. Finding a sense of purpose beyond the illness also contributes to caregivers perceiving their loved ones not primarily as patient but as individuals outside of the disease, reinforcing valuable relationships such as partners, siblings, or children, strengthening emotional bonds. These factors are also highly relevant and well-documented in a suicide-preventive context, as the suicide rate is higher in persons diagnosed with neurological disorders [ 19 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ] and the feeling of being a burden to others, loss of autonomy, and perceived loss of dignity are significant factors in patients with severe chronic neurological diseases for suicide [ 50 , 57 ].
The temporal relief experienced by the CCM was particularly significant for HCSs and did not only improve the satisfaction of HCSs but also removed unfulfilled expectations and concerns about being blamed by patients when expectations could not be met, which previous studied elaborated [ 35 , 36 ]. Moreover, the CCM alleviated the burden on HCSs by addressing patients’ concerns, allowing them to focus on their own medical responsibilities. This aspect probably reduced the dissatisfaction that arises when HCSs are expected to address issues beyond their medical expertise, such as assistive devices, health and social insurance, and the organization and coordination of supplementary therapies, appointments, and contacts [ 35 , 36 , 61 ]. Consequently, the CCM reduced difficulties of HCSs treating persons with neurological or chronical illnesses, which previous research identified as problematic.
HCSs perceive their work as increasingly condensed with numerous time and economic constraints, especially when treating complex and severely ill individuals like PwsMS [ 36 ]. This constraint was mentioned by HCSs in the interviews and was one of the main reasons why they were hesitant to participate in interviews and may also be an explanation for a shorter interview duration than initially planned in the interview guides. The CCM’s overarching navigational competence in the health and social insurance system was particularly valued by HCSs. The complex and often small-scale specialties in the health and social care system are not easily manageable or well-known even for HCSs, and dealing with them can exceed their skills and time capacities [ 61 ]. The CCM played a crucial role in keeping (temporal) resources available for what HCSs are professionally trained and qualified to work on. However, there remains a challenge in finding solutions to the dilemma faced by HCSs regarding their wish to be informed about CCM procedures and linked with each other, while also managing the strain of additional requests and contact with the CCM due to limited (time) resources [ 62 ]. Hudon et al. (2023) suggest that optimizing time resources and improving exchange could involve meetings, information sharing via fax, e-mail, secure online platforms, or, prospectively, within the electronic patient record (EPR). The implementation of an EPR has shown promise in improving the quality of health care and time resources, when properly implemented [ 63 , 64 ]. The challenge lies ineffective information exchange between HCSs and CCM for optimal patient care. The prospect of time saving in the long run and at best for a financial incentive, e.g., when anchoring in the Social Security Code, will help best to win over the HCSs.If this crucial factor can be resolved, there is a chance that HCSs will thoroughly accept the CCM as an important pillar, benefiting not only PwsMS but also other complex patient groups, especially those with long-term neurological or complex oncological conditions that might run chronically.
Care and case management and implications for the health care system
The results of our study suggest that the cross-sectoral long-term advocacy CCM in the COCOS-MS trial, with continuous personal contacts at short intervals and constant reevaluation of needs, problems, resources and goals, is highly valued by PwsMS, caregivers, and HCSs. The trial addresses several key aspects that may have been overlooked in previous studies which have shown great potential for the integration of case management [ 17 , 47 , 62 , 65 , 66 ]. However, they often excluded the overriding care management, missed those patient groups with special severity and complexity who might struggle to reach social and health care structures independently or the interventions were not intended for long-term [ 22 , 37 ]. Our results indicate that the CCM intervention had a positive impact on PwsMS and caregivers as HCSs experienced them with benefits such as increased invigoration, reduced demands, and enhanced self-confidence. However, there was a notable loss experienced by PwsMS and caregivers after the completion of the CCM intervention, even if they had stabilized during the intervention period. The experiences of optimized social and health care for the addressed population, both at an individual and superordinate care level, support the integration of this service into standard care. Beyond the quantitatively measurable outcomes and economic considerations reported elsewhere [ 16 , 20 , 21 ], our results emphasize the importance of regaining control, self-efficacy, self-worth, dignity, autonomy, and social participation. These aspects are highlighted as preventive measures in suicidal contexts, which is particularly relevant for individuals with severe and complex illnesses [ 19 , 50 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ]. Our findings further emphasize the societal responsibilities to offer individuals with severe and complex illnesses the opportunity to regain control and meaningful aspects of life, irrespective of purely economic considerations. This underscores the need for a comprehensive evaluation that not only takes into account quantitative measures but also the qualitative aspects of well-being and quality of life when making recommendations of a CCM in standard care.
The study by J. Y. Joo and Huber (2019) highlighted that CM interventions aligned with the standards of the Case Management Society of America varied in duration, ranging from 1 month to 15.9 years, and implemented in community- or hospital-based settings. However, they noted a limitation in understanding how CM processes unfold [ 67 ]. In contrast, our trial addressed this criticism by providing transparent explanations of the CCM process, which also extends to a superordinate care management [ 40 , 41 ]. Our CCM manual [ 40 ] outlines a standardized and structured procedure for measuring and reevaluating individual resources, problems, and unmet needs on predefined dimensions. It also identifies goals and actions at reducing unmet needs and improving the individual resources of PwsMS and caregivers. Importantly, the CCM manual demonstrates that the CCM process can be structured and standardized, while accounting for the unique aspects of each individual’s serious illness, disease courses, complex needs, available resources, and environmental conditions. Furthermore, the adaptability of the CCM manual to other complex chronically ill patient groups suggests the potential for a standardized approach in various health care settings. This standardized procedure allows for consistency in assessing and addressing the individual needs of patients, ensuring that the CCM process remains flexible while maintaining a structured and goal-oriented framework.
The discussion about the disintegration in the social and health care system and the increasing specialization dates back to 2009 [ 31 , 32 ]. Three strategies were identified to address this issue: (a) “driver-minimizing” [Treiberminimierende], (b) “effect-modifying” [Effektmodifizierende] and (c) “disintegration-impact-minimizing” [Desintegrationsfolgenminimierende] strategies. “Driver-minimizing strategies” involve comprehensive and radical changes within the existing health and social care system, requiring political and social pursuit. “Disintegration-impact-minimizing strategies” are strategies like quality management or tele-monitoring, which are limited in scope and effectiveness. “Effect-modifying strategies”, to which CCM belongs, acknowledges the segmentation within the system but aims to overcome it through cooperative, communicative, and integrative measures. CCM, being an “effect-modifying strategy”, operates the “integrated segmentation model” [Integrierte Segmentierung] rather than the “general contractor model” [Generalunternehmer-Modell] or “total service provider model” [Gesamtdienstleister-Modell] [ 31 , 32 ]. In this model, the advantage lies in providing an overarching and coordinating service to link different HCSs and services cross-sectorally. The superordinate care management aspect of the CCM plays a crucial role in identifying gaps in care, which is essential for future development strategies within the health and social care system. It aims to find or develop (regional) alternatives to ensure optimal care [ 17 , 23 , 24 , 68 , 69 ], using regional services of existing health and social care structures. Therefore, superordinate care management within the CCM process is decisive for reducing disintegration in the system.
Strengths and limitations
The qualitative study results of the explorative COCOS-MS clinical trial, which employed an integrated mixed-method design, provide valuable insights into the individual experiences of three leading stakeholders: PwsMS, caregivers and HCSs with a long-term cross-sectoral CCM. In addition to in-depth interviews, patient and caregiver reported outcome measurements were utilized and will be reported elsewhere. The qualitative study’s strengths include the inclusion of patients who, due to the severity of their condition (e.g. EDSS mean: 6.8, range: 6–8, highly active MS), age (mean: 53.9 years, range: 36–73 years) family constellations, are often underrepresented in research studies and often get lost in existing social and health care structures. The study population is specific to the wider district region of Cologne, but the broad inclusion criteria make it representative of severe MS in Germany. The methodological approach of a deductive and inductive structuring content analysis made it possible to include new findings into an existing theoretical framework.
However, the study acknowledges some limitations. While efforts were made to include more HCSs, time constraints on their side limited the number of interviews conducted and might have biased the results. Some professions are underrepresented in the interviews. Complex symptoms (e.g. fatigue, ability to concentrate), medical or therapeutic appointments and organization of the everyday live may have been reasons for the patients’ and caregivers’ interviews lasting shorter than initially planned.
The provision of functions of a CCM, might have pre-structured the answers of the participants.
At current, there is no support system for PwsMS, their caregivers and HCSs that addresses their complex and unmet needs comprehensively and continuously. There are rare qualitative insights of the three important stakeholders: PwsMS, caregivers and HCSs in one analysis about a supporting service like a CCM. In response to this gap, we developed and implemented a long-term cross-sectoral advocacy CCM and analyzed it qualitatively. PwsMS, their caregivers and HCSs expressed positive experiences, perceiving the CCM as a source of relief and support that improved care across various aspects of life. For patients, the CCM intervention resulted in enhanced autonomy, reviving of personal wellbeing and new established contacts with HCSs. Caregivers reported a reduced organizational burden and felt better informed, and HCSs experienced primarily temporal relief, allowing them to concentrate on their core professional responsibilities. At a higher level of care, the study suggests that the CCM contributed to a reduction in disintegration within the social and health care system.
The feedback from participants is seen as valuable for adapting the CCM intervention and the CCM manual for follow-up studies, involving further complex patient groups such as neurological long-term diseases apart from MS and tailoring the duration of the intervention depending on the complexity of evolving demands.
Availability of data and materials
Generated and/or analyzed datasets of participants are available from the corresponding author on reasonable request to protect participants. Preliminary partial results have been presented as a poster during the EAPC World Congress in June 2023 and the abstract has been published in the corresponding abstract booklet [ 70 ].
Abbreviations
Amyotrophic lateral sclerosis
- Care and case management
Case management
Central nervous system
Communication, Coordination and security for people with multiple sclerosis
Consolidated criteria for reporting qualitative research
German register for clinical studies
Extended disability status scale
Electronic patient record
Quality of life
Multiple sclerosis
Koch-Henriksen N, Magyari M. Apparent changes in the epidemiology and severity of multiple sclerosis. Nat Rev Neurol. 2021;17:676–88. https://doi.org/10.1038/s41582-021-00556-y .
Article PubMed Google Scholar
Ellenberger D, Flachenecker P, Fneish F, Frahm N, Hellwig K, Paul F, et al. Aggressive multiple sclerosis: a matter of measurement and timing. Brain. 2020;143:e97. https://doi.org/10.1093/brain/awaa306 .
Article PubMed PubMed Central Google Scholar
Edmonds P, Vivat B, Burman R, Silber E, Higginson IJ. Loss and change: experiences of people severely affected by multiple sclerosis. Palliat Med. 2007;21:101–7. https://doi.org/10.1177/0269216307076333 .
Kurtzke JF. Rating neurologic impairment in multiple rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology. 1983;33(11):1444–52.
Article CAS PubMed Google Scholar
Galushko M, Golla H, Strupp J, Karbach U, Kaiser C, Ernstmann N, et al. Unmet needs of patients feeling severely affected by multiple sclerosis in Germany: a qualitative study. J Palliat Med. 2014;17:274–81. https://doi.org/10.1089/jpm.2013.0497 .
Borreani C, Bianchi E, Pietrolongo E, Rossi I, Cilia S, Giuntoli M, et al. Unmet needs of people with severe multiple sclerosis and their carers: qualitative findings for a home-based intervention. PLoS One. 2014:e109679. https://doi.org/10.1371/journal.pone.0109679 .
Yamout BI, Alroughani R. Multiple Sclerosis. Semin Neurol. 2018;38:212–25. https://doi.org/10.1055/s-0038-1649502 .
Nissen N, Lemche J, Reestorff CM, Schmidt M, Skjerbæk AG, Skovgaard L, et al. The lived experience of uncertainty in everyday life with MS. Disabil Rehabil. 2022;44:5957–63. https://doi.org/10.1080/09638288.2021.1955302 .
Strupp J, Hartwig A, Golla H, Galushko M, Pfaff H, Voltz R. Feeling severely affected by multiple sclerosis: what does this mean? Palliat Med. 2012;26:1001–10. https://doi.org/10.1177/0269216311425420 .
Strupp J, Voltz R, Golla H. Opening locked doors: Integrating a palliative care approach into the management of patients with severe multiple sclerosis. Mult Scler J. 2016;22:13–8.
Article CAS Google Scholar
Kraft AK, Berger K. Kernaspekte einer bedarfsgerechten Versorgung von Patienten mit Multipler Sklerose : Inanspruchnahme ambulanter Leistungen und „shared decision making“ [Core aspects of a needs-conform care of patients with multiple sclerosis : Utilization of outpatient services and shared decision making]. Nervenarzt. 2020;91:503–10. https://doi.org/10.1007/s00115-020-00906-z .
Doshi A, Chataway J. Multiple sclerosis, a treatable disease. Clin Med (Lond). 2017;17:530–6. https://doi.org/10.7861/clinmedicine.17-6-530 .
Kobelt G, Thompson A, Berg J, Gannedahl M, Eriksson J. New insights into the burden and costs of multiple sclerosis in Europe. Mult Scler. 2017;23:1123–36. https://doi.org/10.1177/1352458517694432 .
Conradsson D, Ytterberg C, Engelkes C, Johansson S, Gottberg K. Activity limitations and participation restrictions in people with multiple sclerosis: a detailed 10-year perspective. Disabil Rehabil. 2021;43:406–13. https://doi.org/10.1080/09638288.2019.1626919 .
Sorensen PS, Giovannoni G, Montalban X, Thalheim C, Zaratin P, Comi G. The Multiple Sclerosis Care Unit. Mult Scler J. 2019;5:627–36.
Article Google Scholar
Tan H, Yu J, Tabby D, Devries A, Singer J. Clinical and economic impact of a specialty care management program among patients with multiple sclerosis: a cohort study. Mult Scler. 2010;16:956–63. https://doi.org/10.1177/1352458510373487 .
Article CAS PubMed PubMed Central Google Scholar
Oeseburg B, Wynia K, Middel B, Reijneveld SA. Effects of case management for frail older people or those with chronic illness: a systematic review. Nurs Res. 2009;58:201–10.
Aiken LS, Butner J, Lockhart CA, Volk-Craft BE, Hamilton G, Williams FG. Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill. J Palliat Med. 2006;9:111–26. https://doi.org/10.1089/jpm.2006.9.111 .
Kuhn U, Düsterdiek A, Galushko M, Dose C, Montag T, Ostgathe C, Voltz R. Identifying patients suitable for palliative care—a descriptive analysis of enquiries using a Case Management Process Model approach. BMC Res Notes. 2012;5:611. https://doi.org/10.1186/1756-0500-5-611 .
Leary A, Quinn D, Bowen A. Impact of proactive case management by multiple sclerosis specialist nurses on use of unscheduled care and emergency presentation in multiple sclerosis: a case study. Int J MS Care. 2015;17:159–63. https://doi.org/10.7224/1537-2073.2014-011 .
Strupp J, Dose C, Kuhn U, Galushko M, Duesterdiek A, Ernstmann N, et al. Analysing the impact of a case management model on the specialised palliative care multi-professional team. Support Care Cancer. 2018;26:673–9. https://doi.org/10.1007/s00520-017-3893-3 .
Wynia K, Annema C, Nissen H, de Keyser J, Middel B. Design of a Randomised Controlled Trial (RCT) on the effectiveness of a Dutch patient advocacy case management intervention among severely disabled Multiple Sclerosis patients. BMC Health Serv Res. 2010;10:142. https://doi.org/10.1186/1472-6963-10-142 .
Ewers M, Schaeffer D, editors. Case Management in Theorie und Praxis. Bern: Huber; 2005.
Google Scholar
Neuffer M. Case Management: Soziale Arbeit mit Einzelnen und Familien. 5th ed. Weinheim, Basel: Beltz Juventa; 2013.
Case Management Society of America. The standards of practice for case management. 2022.
Deutsche Gesellschaft für Care und Case Management e.V., editor. Case Management Leitlinien: Rahmenempfehlung, Standards und ethische Grundlagen. 2nd ed. Heidelberg: Medhochzwei; 2020.
Monzer M. Case Management Grundlagen. 2nd ed. Heidelberg: Medhochzwei; 2018.
Wissert M. Grundfunktionen und fachliche Standards des Unterstützungsmanagements. Z Gerontol Geriat. 1998;31(5):331–7.
Wissert M. Tools und Werkzeuge beim Case Management: Die Hilfeplanung. Case Manag. 2007;1:35–7.
Schaeffer D, Berens E-M, Vogt D. Health literacy in the German population. Dtsch Arztebl Int. 2017;114:53–60. https://doi.org/10.3238/arztebl.2017.0053 .
Pfaff H, Schulte H. Der onkologische Patient der Zukunft. Onkologe. 2012;18:127–33. https://doi.org/10.1007/s00761-011-2201-y .
Pfaff H, Kowalski C, Ommen O. Modelle zur Analyse von Integration und Koordination im Versorgungssystem. In: Ameldung, Sydow, Windeler, editor. Vernetzung im Gesundheitswesen: Wettbewerb und Kooperation. Stuttgart: Kohlhammer Verlag; 2009. p. 75–90.
Golla H, Mammeas S, Galushko M, Pfaff H, Voltz R. Unmet needs of caregivers of severely affected multiple sclerosis patients: A qualitative study. Palliat Support Care. 2015;13(6):1685–93.
Golla H, Galushko M, Pfaff H, Voltz R. Multiple sclerosis and palliative care - perceptions of severely affected multiple sclerosis patients and their health professionals: a qualitative study. BMC Palliat Care. 2014;13:11. https://doi.org/10.1186/1472-684x-13-11 .
Golla H, Galushko M, Pfaff H, Voltz R. Unmet needs of severely affected multiple sclerosis patients: the health professionals’ view. Palliat Med. 2012;26:139–51. https://doi.org/10.1177/0269216311401465 .
Methley AM, Chew-Graham CA, Cheraghi-Sohi S, Campbell SM. A qualitative study of patient and professional perspectives of healthcare services for multiple sclerosis: implications for service development and policy. Health Soc Care Community. 2017;25:848–57. https://doi.org/10.1111/hsc.12369 .
Kalb R, Costello K, Guiod L. Case management services to meet the complex needs of patients with multiple sclerosis in the community—the successes and challenges of a unique program from the national multiple sclerosis society. US Neurology. 2019;15:27–31.
Krüger K, Fricke LM, Dilger E-M, Thiele A, Schaubert K, Hoekstra D, et al. How is and how should healthcare for people with multiple sclerosis in Germany be designed?-The rationale and protocol for the mixed-methods study Multiple Sclerosis-Patient-Oriented Care in Lower Saxony (MS-PoV). PLoS One. 2021;16:e0259855. https://doi.org/10.1371/journal.pone.0259855 .
Ivancevic S, Weegen L, Korff L, Jahn R, Walendzik A, Mostardt S, et al. Effektivität und Kosteneffektivät von Versorgungsmanagement-Programmen bei Multipler Sklerose in Deutschland – Eine Übersichtsarbeit. Akt Neurol. 2015;42:503–8. https://doi.org/10.1055/s-0035-1564111 .
Müller A, Dillen K, Dojan T, Ungeheuer S, Goereci Y, Dunkl V, et al. Development of a long-term cross-sectoral case and care management manual for patients with severe multiple sclerosis and their caregivers. Prof Case Manag. 2023;28:183–93. https://doi.org/10.1097/NCM.0000000000000608 .
Golla H, Dillen K, Hellmich M, Dojan T, Ungeheuer S, Schmalz P, et al. Communication, Coordination, and Security for People with Multiple Sclerosis (COCOS-MS): a randomised phase II clinical trial protocol. BMJ Open. 2022;12:e049300. https://doi.org/10.1136/bmjopen-2021-049300 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. https://doi.org/10.1093/intqhc/mzm042 .
Kuckartz U. Qualitative Inhaltsanalyse: Methoden, Praxis, Computerunterstützung. 4th ed. Weinheim: Beltz Juventa; 2018.
Akyirem S, Ekpor E, Aidoo-Frimpong GA, Salifu Y, Nelson LE. Online interviews for qualitative health research in Africa: a scoping review. Int Health. 2023. https://doi.org/10.1093/inthealth/ihad010 .
Peasgood T, Bourke M, Devlin N, Rowen D, Yang Y, Dalziel K. Randomised comparison of online interviews versus face-to-face interviews to value health states. Soc Sci Med. 2023;323:115818. https://doi.org/10.1016/j.socscimed.2023.115818 .
Giordano A, Cimino V, Campanella A, Morone G, Fusco A, Farinotti M, et al. Low quality of life and psychological wellbeing contrast with moderate perceived burden in carers of people with severe multiple sclerosis. J Neurol Sci. 2016;366:139–45. https://doi.org/10.1016/j.jns.2016.05.016 .
Joo JY, Liu MF. Experiences of case management with chronic illnesses: a qualitative systematic review. Int Nurs Rev. 2018;65(1):102–1113.
Freeman J, Gorst T, Gunn H, Robens S. “A non-person to the rest of the world”: experiences of social isolation amongst severely impaired people with multiple sclerosis. Disabil Rehabil. 2020;42:2295–303. https://doi.org/10.1080/09638288.2018.1557267 .
National Institute for Health and Care Excellence. Multiple sclerosis: Management of multiple sclerosis in primary and secondary care. 2014.
Erdmann A, Spoden C, Hirschberg I, Neitzke G. The wish to die and hastening death in amyotrophic lateral sclerosis: A scoping review. BMJ Support Palliat Care. 2021;11:271–87. https://doi.org/10.1136/bmjspcare-2020-002640 .
Erlangsen A, Stenager E, Conwell Y, Andersen PK, Hawton K, Benros ME, et al. Association between neurological disorders and death by suicide in Denmark. JAMA. 2020;323:444–54. https://doi.org/10.1001/jama.2019.21834 .
Kalb R, Feinstein A, Rohrig A, Sankary L, Willis A. Depression and suicidality in multiple sclerosis: red flags, management strategies, and ethical considerations. Curr Neurol Neurosci Rep. 2019;19:77. https://doi.org/10.1007/s11910-019-0992-1 .
Feinstein A, Pavisian B. Multiple sclerosis and suicide. Mult Scler. 2017;23:923–7. https://doi.org/10.1177/1352458517702553 .
Marrie RA, Salter A, Tyry T, Cutter GR, Cofield S, Fox RJ. High hypothetical interest in physician-assisted death in multiple sclerosis. Neurology. 2017;88:1528–34. https://doi.org/10.1212/WNL.0000000000003831 .
Gauthier S, Mausbach J, Reisch T, Bartsch C. Suicide tourism: a pilot study on the Swiss phenomenon. J Med Ethics. 2015;41:611–7. https://doi.org/10.1136/medethics-2014-102091 .
Fischer S, Huber CA, Imhof L, MahrerImhof R, Furter M, Ziegler SJ, Bosshard G. Suicide assisted by two Swiss right-to-die organisations. J Med Ethics. 2008;34:810–4. https://doi.org/10.1136/jme.2007.023887 .
Strupp J, Ehmann C, Galushko M, Bücken R, Perrar KM, Hamacher S, et al. Risk factors for suicidal ideation in patients feeling severely affected by multiple sclerosis. J Palliat Med. 2016;19:523–8. https://doi.org/10.1089/jpm.2015.0418 .
Spence RA, Blanke CD, Keating TJ, Taylor LP. Responding to patient requests for hastened death: physician aid in dying and the clinical oncologist. J Oncol Pract. 2017;13:693–9. https://doi.org/10.1200/JOP.2016.019299 .
Monforte-Royo C, Villavicencio-Chávez C, Tomás-Sábado J, Balaguer A. The wish to hasten death: a review of clinical studies. Psychooncology. 2011;20:795–804. https://doi.org/10.1002/pon.1839 .
Blanke C, LeBlanc M, Hershman D, Ellis L, Meyskens F. Characterizing 18 years of the death with dignity act in Oregon. JAMA Oncol. 2017;3:1403–6. https://doi.org/10.1001/jamaoncol.2017.0243 .
Methley A, Campbell S, Cheraghi-Sohi S, Chew-Graham C. Meeting the mental health needs of people with multiple sclerosis: a qualitative study of patients and professionals. Disabil Rehab. 2017;39(11):1097-105. https://doi.org/10.1080/09638288.2016.1180547 .
Hudon C, Bisson M, Chouinard M-C, Delahunty-Pike A, Lambert M, Howse D, et al. Implementation analysis of a case management intervention for people with complex care needs in primary care: a multiple case study across Canada. BMC Health Serv Res. 2023;23:377. https://doi.org/10.1186/s12913-023-09379-7 .
Beckmann M, Dittmer K, Jaschke J, Karbach U, Köberlein-Neu J, Nocon M, et al. Electronic patient record and its effects on social aspects of interprofessional collaboration and clinical workflows in hospitals (eCoCo): a mixed methods study protocol. BMC Health Serv Res. 2021;21:377. https://doi.org/10.1186/s12913-021-06377-5 .
Campanella P, Lovato E, Marone C, Fallacara L, Mancuso A, Ricciardi W, Specchia ML. The impact of electronic health records on healthcare quality: a systematic review and meta-analysis. Eur J Public Health. 2016;26:60–4. https://doi.org/10.1093/eurpub/ckv122 .
García-Hernández M, González de León B, Barreto-Cruz S, Vázquez-Díaz JR. Multicomponent, high-intensity, and patient-centered care intervention for complex patients in transitional care: SPICA program. Front Med (Lausanne). 2022;9:1033689. https://doi.org/10.3389/fmed.2022.1033689 .
Meisinger C, Stollenwerk B, Kirchberger I, Seidl H, Wende R, Kuch B, Holle R. Effects of a nurse-based case management compared to usual care among aged patients with myocardial infarction: results from the randomized controlled KORINNA study. BMC Geriatr. 2013. https://doi.org/10.1186/1471-2318-13-115 .
Joo JY, Huber DL. Case management effectiveness on health care utilization outcomes: a systematic review of reviews. West J Nurs Res. 2019;41:111–33. https://doi.org/10.1177/0193945918762135 .
Stergiopoulos V, Gozdzik A, Misir V, Skosireva A, Connelly J, Sarang A, et al. Effectiveness of housing first with intensive case management in an ethnically diverse sample of homeless adults with mental illness: a randomized controlled trial. PLoS One. 2015;10:e0130281. https://doi.org/10.1371/journal.pone.0130281 .
Löcherbach P, Wendt R, editors. Care und Case Management: Transprofessionelle Versorgungsstrukturen und Netzwerke. 1st ed. Stuttgart: Kohlhammer; 2020.
EAPC2023 Abstract Book. Palliat Med. 2023;37:1–302. https://doi.org/10.1177/02692163231172891 .
Download references
Acknowledgements
We would like to thank all the patients, caregivers and health care specialists who volunteered their time to participate in an interview and the trial, Carola Janßen for transcribing the interviews, Fiona Brown for translating the illustrative quotes and Beatrix Münzberg, Kerstin Weiß and Monika Höveler for data collection in the quantitative study part.
COCOS-MS Trial Group
Anne Müller 1 , Fabian Hebben 1 , Kim Dillen 1 , Veronika Dunkl 1 , Yasemin Goereci 2 , Raymond Voltz 1,3,4 , Peter Löcherbach 5 , Clemens Warnke 2 , Heidrun Golla 1 , Dirk Müller 6 , Dorthe Hobus 1 , Eckhard Bonmann 7 , Franziska Schwartzkopff 8 , Gereon Nelles 9 , Gundula Palmbach 8 , Herbert Temmes 10 , Isabel Franke 1 , Judith Haas 10 , Julia Strupp 1 , Kathrin Gerbershagen 7 , Laura Becker-Peters 8 , Lothar Burghaus 11 , Martin Hellmich 12 , Martin Paus 8 , Solveig Ungeheuer 1 , Sophia Kochs 1 , Stephanie Stock 6 , Thomas Joist 13 , Volker Limmroth 14
1 Department of Palliative Medicine, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
2 Department of Neurology, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
3 Center for Integrated Oncology Aachen Bonn Cologne Düsseldorf (CIO ABCD), University of Cologne, Cologne, Germany
4 Center for Health Services Research (ZVFK), University of Cologne, Cologne, Germany
5 German Society of Care and Case Management e.V. (DGCC), Münster, Germany
6 Institute for Health Economics and Clinical Epidemiology (IGKE), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
7 Department of Neurology, Klinikum Köln, Cologne, Germany
8 Clinical Trials Centre Cologne (CTCC), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
9 NeuroMed Campus, MedCampus Hohenlind, Cologne, Germany
10 German Multiple Sclerosis Society Federal Association (DMSG), Hannover, Germany
11 Department of Neurology, Heilig Geist-Krankenhaus Köln, Cologne, Germany
12 Institute of Medical Statistics and Computational Biology (IMSB), Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
13 Academic Teaching Practice, University of Cologne, Cologne, Germany
14 Department of Neurology, Klinikum Köln-Merheim, Cologne, Germany
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Innovation Funds of the Federal Joint Committee (G-BA), grant number: 01VSF19029.
Author information
Authors and affiliations.
Department of Palliative Medicine, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
Anne Müller, Fabian Hebben, Kim Dillen, Veronika Dunkl, Raymond Voltz & Heidrun Golla
Department of Neurology, Faculty of Medicine and University Hospital, University of Cologne, Cologne, Germany
Yasemin Goereci & Clemens Warnke
Center for Integrated Oncology Aachen Bonn Cologne Düsseldorf (CIO ABCD), University of Cologne, Cologne, Germany
Raymond Voltz
Center for Health Services Research, University of Cologne, Cologne, Germany
German Society of Care and Case Management E.V. (DGCC), Münster, Germany
Peter Löcherbach
You can also search for this author in PubMed Google Scholar
- Anne Müller
- , Fabian Hebben
- , Kim Dillen
- , Veronika Dunkl
- , Yasemin Goereci
- , Raymond Voltz
- , Peter Löcherbach
- , Clemens Warnke
- , Heidrun Golla
- , Dirk Müller
- , Dorthe Hobus
- , Eckhard Bonmann
- , Franziska Schwartzkopff
- , Gereon Nelles
- , Gundula Palmbach
- , Herbert Temmes
- , Isabel Franke
- , Judith Haas
- , Julia Strupp
- , Kathrin Gerbershagen
- , Laura Becker-Peters
- , Lothar Burghaus
- , Martin Hellmich
- , Martin Paus
- , Solveig Ungeheuer
- , Sophia Kochs
- , Stephanie Stock
- , Thomas Joist
- & Volker Limmroth
Contributions
HG, KD, CW designed the trial. HG, KD obtained ethical approvals. HG, KD developed the interview guidelines with help of the CCM (SU). AM was responsible for collecting qualitative data, developing the code system, coding, analysis of the data and writing the first draft of the manuscript, thoroughly revised and partly rewritten by HG. FH supported in collecting qualitative data, coding and analysis of the interviews. KD supported in collecting qualitative data. AM, FH, KD, VD, YG, RV, PL, CW, HG discussed and con-solidated the finalized category system. AM, FH, KD, VD, YG, RV, PL, CW, HG read and commented on the manuscript and agreed to the final version.
Authors’ information
Not applicable.
Corresponding author
Correspondence to Anne Müller .
Ethics declarations
Ethics approval and consent to participate.
Participants were provided with oral and written information about the trial and provided written informed consent. Ethical approval was obtained from the Ethics Committee of the University of Cologne (#20–1436). The trial is registered in the German Register for Clinical Studies (DRKS) (DRKS00022771) and is conducted under the Declaration of Helsinki.
Consent for publication
Competing interests.
Clemens Warnke has received institutional support from Novartis, Alexion, Sanofi Genzyme, Janssen, Biogen, Merck and Roche. The other authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Müller, A., Hebben, F., Dillen, K. et al. “So at least now I know how to deal with things myself, what I can do if it gets really bad again”—experiences with a long-term cross-sectoral advocacy care and case management for severe multiple sclerosis: a qualitative study. BMC Health Serv Res 24 , 453 (2024). https://doi.org/10.1186/s12913-024-10851-1
Download citation
Received : 23 November 2023
Accepted : 11 March 2024
Published : 10 April 2024
DOI : https://doi.org/10.1186/s12913-024-10851-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cross-sectoral
- Qualitative research
- Health care specialist
- Severe multiple sclerosis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 13 April 2024
Exploring mental health problems and support needs among pregnant and parenting teenagers in rural areas Of Limpopo, South Africa
- Livhuwani Muthelo 1 ,
- Masenyani Oupa Mbombi 1 ,
- Peter Mphekgwana 2 ,
- Linneth Nkateko Mabila 3 ,
- Inos Dhau 4 ,
- Joseph Tlouyamma 5 ,
- Reneilwe Given Mashaba 6 ,
- Katlego Mothapo 6 ,
- Cairo Bruce Ntimane 6 ,
- Kagiso Peace Seakamela 6 ,
- Rathani Nemuramba 6 ,
- Eric Maimela 7 &
- Tholene Sodi 8
BMC Women's Health volume 24 , Article number: 236 ( 2024 ) Cite this article
226 Accesses
7 Altmetric
Metrics details
Globally, teenage pregnancy is among the most social problems, affecting 21 million adolescents aged 15–19. Due to the increased responsibility of prenatal and postnatal care for their infants without support, pregnant and parenting teenagers, tend to experience mental health problems. Factors contributing to these problems among pregnant and parenting teenagers in rural African settings have hardly received scholarly attention and, therefore, are less understood. The purpose of the study was to explore mental health and challenges among pregnant and parenting teenagers,.
The study adopted a qualitative descriptive, exploratory, and phenomenological design. Purposive sampling was used to select 22 pregnant and parenting teenagers 18 years or older. Data were collected in ten selected clinics within the Demographic Surveillance Systems (HDSS) of DIMAMO and analysed using qualitative content analysis.
The findings reveal that pregnant and parenting teenagers in rural areas experience various mental challenges such as depression. These challenges are caused by social problems such as stigmatisation, lack of support from families and friends, as well as parenting demands that contribute to poor progress at school or dropouts. Pregnant teens expressed concerns about the lack of spousal support resulting from abandoning their partners.
Conclusions
Stress and depression were self-reported as mental problems among participants with various psychosocial implications, such as school dropout and miscarriage. There are various contributing factors to the mental health problems identified among pregnant and parenting teenagers, including inadequate family and spousal support. Access to integrated reproductive, psychosocial, and mental health services could be essential for these pregnant and parenting teenagers, to improve their mental well-being and improve the support system.
Peer Review reports
Introduction
Globally, 13 million of the 21 million teenage teenagers, who become pregnant each year between the ages of 15 and 19 give birth, and most of them are from low and middle-income countries (LMICs) [ 1 , 2 ]. In sub-Saharan Africa, 35% of pregnancies among 15 to 19 years were unintended, unwanted, or mistimed, and most of the relationships during this developmental period were considered unstable. About two thirds of these unplanned pregnancies end in live births, and the other third ends in risky abortions [ 1 , 2 , 3 ]. Since teenage pregnancy occurs during the development period, adolescents are often forced to transition from childhood to adulthood, which can result in physical, biological, emotional, social and mental health challenges [ 4 , 5 ]. During the transition process, pregnant adolescents are exposed to many health-related challenges that could negatively affect them and put their health and that of their unborn children at risk [ 5 , 6 ]. In addition, stress and anxiety are frequent during pregnancy, particularly among unmarried adolescents, because adjusting to heightened expectations can be a period of emotional and mental strain [ 7 , 8 , 9 ].
Again, during the transition to adulthood, pregnant adolescents are more likely to find it difficult to deal with pregnancy-related problems. This may result in feelings of low self-esteem and various mental health problems such as stress, anxiety, fear, depression, and suicidal thoughts [ 10 ]. Scholars have argued that depressed and anxious mothers may develop strong feelings of annoyance, which could make it difficult for them to care for their children [ 11 , 12 ]. Furthermore, several researchers have shown that teenage pregnancy and parenting are associated with an increased risk of problems during pregnancy and delivery, adverse neonatal outcomes with recurrent pregnancies, and developmental abnormalities in their children [ 10 , 11 , 13 ]. Consequently, the children tend to have negative emotions with decreased cognitive performance as young as two months. They may also have decreased cognitive performance, which is a negative consequence and a serious concern that could continue to affect them even during their college years [ 12 , 14 , 15 , 16 ]. Studies have shown that pregnant and parenting teenagers, face additional challenges in life after giving birth, including lower educational attainment, lower incomes, and higher unemployment rates [ 17 , 18 ]. Furthermore, parenting teenagers are at risk of experiencing psychiatric disorders and suicidal behaviour, with the prevalence of a higher mortality rate later in life. Research conducted in Soweto in South Africa (SA) indicates that young women between the ages of 13 and 16 had an abortion rate of 23%, while with teenagers between 17 and 19, the abortion rate was 14.9% [ 1 , 19 ].
A group of parenting teenagers, in SA were found to have a much higher incidence of possible mental illnesses than their peers who had never given birth (18.2% vs. 9.6%) [ 12 ]. Both obstetric difficulties and poor postpartum mother functioning are associated with mental disorders. These circumstances can adversely affect maternal mental health, parenting, and behavioural outcomes for their children. It is against this background that the research team aimed to explore mental health problems, contributing factors of mental health, consequences of mental problems, and support needs among pregnant teenagers residing in selected rural communities of Limpopo Province.
Material and methods
Study design.
The qualitative exploratory, descriptive, and phenomenological design was adopted. This study design uses a flexible approach that produces high-quality data that enable a deeper understanding of lived experiences [ 20 ]. About the support and mental health challenges experienced by pregnant and parenting teenagers, in selected rural communities of Limpopo province.
The study was carried out in ten clinics within the DIMAMO Population Health Research Centre (PHRC), which is one of the health and demographic surveillance sites affiliated with the South African Population Research Infrastructure Network (SAPRIN), which is hosted by the South African Medical Research Council and funded by the National Department of Science and Innovation (DSI). The site is located in the Capricorn District of Limpopo Province and covers a population of approximately 100,000 people. At the ten selected clinics, maternal and child health services are provided to women during and after pregnancy.
Population and sampling
In the context of this study, most of the participants resided in rural, underprivileged communities ravaged by poverty. The target population of the study was all pregnant and parenting teenagers, aged 15 to 19 years or under. Purposive sampling was used to select 22 participants with lived experiences of mental health problems during their adolescent pregnancy and early parenting. The selection criteria of the participants were being a teenage woman, being pregnant, including being a teenage mother. All participants were enrolled for antenatal care (ANC) or child growth monitoring in the selected clinics.
Data collection
Individual in-depth interviews were conducted with participants between the period of September 2022 to November 2022, who were recruited through the clinic managers. The project team explained the purpose and objectives of the study to managers and staff, who then identified the pregnant and parenting teenagers, who were enrolled as participants in the study. The research team then introduced itself to them and explained the purpose of the study. Arrangements for the date and time for data collection were made. Interviews were carried out in private rooms within the clinic premises by LM (Female) and MOM (Male), who are experienced qualitative researchers, MOM, RGM, CBN, KM, and RN. The interviews were conducted following the interview guide with questions asked. The researchers used audio recorders along with notepads to record the interviews that lasted approximately 45 min. Data were collected until data saturation was reached at participant number twenty-two. The sociodemographic profiles of the participants are detailed elsewhere [ 21 ].
Data analysis
Qualitative content analysis was used as recommended by Creswell and Guetterman [ 20 ] to analyse the data. A team of three authors organised the data, including the transcription of all recorded audio and filed notes. Three authors read through the transcripts to obtain a general sense of the material. Thereafter coding of data was done, which includes locating segments to assign code labels. The codes were examined to build the themes and their descriptions. A meeting was arranged with other authors to identify and refine the themes. Reporting the themes as qualitative findings. Finally, all the authors agreed on the themes and subthemes outlined in Table 1 . The adoption of content analysis assisted the research team in interpreting the content of text data through the methodical coding classification process. The research team allowed these themes and subthemes to flow from data through intense immersion in the data to allow new insights to emerge. The themes and subthemes are presented in Table 1 .
Contributory factors to mental problems among pregnant and parenting teenagers
The study findings illustrated the contributing factors to mental problems among pregnant and parenting teenagers, resulting in the following themes.
Mixed perceptions of mental illness among pregnant and parenting adolescents
We observed mixed perceptions about mental illness in rural areas, with some pregnant and parenting adolescents attributing mental illness to worries about too many things, especially when one has problems with family and friends. The adolescents argued that they experienced depression and stress during their early motherhood state. The following assertions illustrate these findings:
Ok, depression is when someone is stressed because you are pregnant, for example, like you, you are stressed at school or home because you are pregnant (Participant 10).
Community and friend stigmatisation
The study findings suggest that stigmatisation by the community and friends is a contributing factor to depression among pregnant and parenting adolescents in rural areas. The teenagers expressed fear of being judged and not having support from family and friends, who tend to discriminate against them due to their pregnancy. The following extracts illustrate this.
Fear of being judged and not having support or anyone to talk to… If you come from a family that does not support your friends who gossip about you and the community that also gossips about you, ‘stopped to overthink” (Participant 4).
Being a single parent is challenging versus lack of partner support
Pregnant and parenting teenagers expressed concern about being a single parent. They perceived this as challenging, especially when there was a lack of spousal support. Concern about the father who disappears when needed or the father abandoning the child was emphasised. This is reflected in the following quotes.
On the other hand, the father of the child has abandoned his child. As a mother, I started to feel stressed about food and clothing for both me and the child (Participant 11).
Psychosocial problems due to adolescent pregnancy
The study found that some psychosocial problems arise from teenage pregnancy. These included self-actualisation challenges, school dropout, miscarriage, and abortion. The following themes support the objective:
School dropout
In addition to poor academic performance, pregnant and parenting teenagers expressed the desire to drop out of school. The reason for this is the absence of guardians or babysitters for their newborns. These findings are supported by the following quotations.
We end up dropping out of school because we have people to babysit for us, and also when you are with your friends who have not had children, you feel like you are no longer part of them (Participant 2).
Self-actualization challenges
The findings indicate that the participants tend to fail to reach self-actualisation due to teenage pregnancy. They argued that they might not achieve their goals or dreams due to the disruption of their academic performance at school. The following quotes support the findings:
…I thought of running away from home because I thought they would be better off without me because I thought I was the problem (Participant 3).
Miscarriage and abortion
Other pregnant teenagers wish to abort their babies due to a perceived lack of support systems. Some of them were concerned about the possibility of a miscarriage due to excessive worries about their status. These findings are supported by the following quotations.
You can lose your baby by miscarriage, or your baby’s condition may not be good when you give birth… When a pregnant woman has a lot on her mind, it affects baby growth and she will give birth to a premature baby or a disabled baby. You might end up stressed out because your classmates talk about it (Participant 1).
Availability of support systems and their role in minimising mental problems among pregnant teenagers
The study findings demonstrated that the availability of support systems helps minimise mental problems among pregnant teenagers. They felt that family, school, healthcare facilities and community played a significant supportive role. The following themes demonstrate how we achieved the objective:
Role of family and community as support systems
The study findings demonstrated mixed perceptions about the role of family and community as support systems among pregnant and parenting adolescents. They acknowledged the role played by family members and the support received at home. As reflected in the following quotes, they felt that family, friends, and neighbours provided emotional support.
The people we stay with at home support us… Just for them to always talk about pregnancy and pregnancy-related issues and for community members to stop pointing fingers and gossiping about us (Participant 1).
Role of healthcare workers and clinic support systems
The pregnant teens felt that healthcare workers in clinics play an important role in their mental well-being. They found the support groups there helpful. The following quotes reflect this sentiment:
…Yes, clinics support teenage moms and pregnant teens - Yes, at the clinic, we have social workers. Therefore, you can get support from them Participant 8).
The role of culture
Teens pregnant and parenting were asked to share their views on the role of culture in their lives. They were of the view that culture plays a significant role in guiding, as shown in the following quotes:
It teaches us what kind of clothes to wear and not wear, saying that your belly does not have to show/ or the next person must not see how big your tummy is. However, it has no clear role in depression (Participant 1).
They help us to be informed of how things were done in the past e.g. consulting with your ancestors before the baby is born and therefore support us accordingly (Participant 2).
The supportive role of teachers and social workers
The findings of the study illustrated the role of teachers and social workers as valuable support systems for pregnant and parenting adolescents. The following quotations lend support to this finding.
…Yes, social workers are there to help us, but not the community. A Centre for Women and Pregnant Teenagers is opened to help and motivate teens with food parcels now and then (Participant 11).
The reported contributing factors to mental health problems among pregnant and parenting teenagersinclude inadequate support systems from partners, family, and the community, and being a single mother without financial support. It is noted that maternal and prenatal health is a concern among adolescents [ 22 ]. The findings reveal that these teenagers experience mental problems, specifically depression and stress, as most of them find themselves worrying about many things during their pregnancy or parenting journey. This is consistent with the findings of other studies that pregnancy poses a serious challenge to the mental health of pregnant and parenting adolescents [ 22 , 23 , 24 , 25 ]. In addition, adolescents indicated that the contributing factors to most of their worries include problems with their families and friends related to support and acceptance of their pregnancy. Stigmatisation from the community and friends was also described as a contributing factor to depression. The literature denotes that pregnant and parenting adolescents are stigmatised by society and this negatively impacts their willingness to seek health services [ 22 , 26 , 27 , 28 ]. Therefore, it is important to raise awareness in the community and educate them about the importance of social support for pregnant and parenting teenagers from their families, the father of the baby, friends, and the community to kerb the detrimental effects of depression among this group.
Pregnant teenagers expressed their concern about single parenthood, which is challenging, especially lack of spousal support resulting from abandonment of the pregnancy. This experience is similar to that of teenage mothers in a study by Ntshayintshayi et al. [ 25 ], who stated that parenting is hard and stressful, and therefore that parenting needs spousal support [ 29 ]. The challenges associated with teenage pregnancy and parenting affect emotions and end in somatization, with signs and symptoms that would be harmful to healthy pregnancy or child [ 24 , 30 ]. Pregnancy risks are related, among others, to psychological aspects and lack of family support, which may lead to high stress levels. In some families, teen pregnancy may be considered natural when there is a stable union between the teenager and the parents [ 31 ]. Family support is described as a fundamental need for parenting teenagers. Grandmothers are considered an important foundation of support in this regard, as they have numerous roles in the family, including advising, coaching and coordinating activities of other family members, and managing family resources [ 32 , 33 ]. Contrary to the findings [ 25 ] that demonstrated that nurses have a negative attitude toward teenage pregnancy, the participants revealed that nurses did not treat them well during clinic visits. This experience made participants’ lives difficult.
The observed support systems for pregnant teenagers include various family support systems, spousal and community support systems, and support from school and social workers in clinics. In particular, adolescents experience these support systems differently, with some satisfied and others not satisfied. Multidisciplinary healthcare is considered an essential need for adolescent mothers and their children. Holistic healthcare that combines medical and psychosocial services is necessary for teenagers. Pregnant teenagers and adolescent mothers need access to medical and psychosocial support. Support services are crucial in addressing mental health problems among pregnant teens and adolescent mothers in rural areas, who require access to mental health services, support groups, financial assistance, housing support, and educational opportunities. However, providing support to pregnant teenagers in rural settings can be challenging due to limited access to mental health services, social stigma, financial restrictions, and poor transportation. Therefore, it is important to address these challenges and to provide adequate support to pregnant teenagers to promote positive mental health outcomes. To handle the mental health challenges of pregnant and parenting teenagers,, doctors, nurses, social workers, dietitians, psychologists, therapists and even personnel of the Department of Basic Education are needed to work as a multidisciplinary team [ 34 ].
Limitations
The study was conducted in a selected surveillance area of Limpopo Province using the qualitative research approach. Thus, the findings cannot be generalised to other surveillance areas in different provinces. In terms of methods, mental problems were only self-reported without the use of the reporting scale for depression or stress. Furthermore, the sample of teenagers was based on those who were making consultations in selected primary healthcare settings.
The study concluded that pregnant and parenting adolescents experience several challenges related to mental health problems during pregnancy and motherhood. Various factors contribute to mental problems among teenagers, including being a single parent, inadequate family support, and discrimination by the community. Although socioeconomic status and cultural factors also played a significant role in the type of support received, participants acknowledged the services provided by local social workers. Therefore, we recommend the implementation of integrated support programmes, which involve community membership and a multidisciplinary healthcare approach to address the financial, health and psychosocial needs of pregnant teenagers and mothers.
Data availability
Data generated or analysed during this study are included in this published article.
Abbreviations
antenatal care
Department of Science and Innovation
Low- and middle-income countries
Population Health Research Centre
South Africa
South African Population Research Infrastructure Network
Turfloop Research Ethics Committee
Yah CS, Ndlovu S, Kutywayo A, Naidoo N, Mahuma T, Mullick S. The prevalence of pregnancy among adolescent girls and young women in the economic hub of the southern African Development Community. A systematic review and meta-analysis. Health Promot Perspect. 2020;10(4):325.
Article PubMed PubMed Central Google Scholar
Bankole A, Malarcher S. Removing barriers to adolescents’ access to contraceptive information and services. Stud Fam Plann. 2010;41(2):117–24.
Article PubMed Google Scholar
Schlyter A, Chipeta LK. Body politics and women citizens: African experiences. 2009.
Agnafors S, Bladh M, Svedin CG, Sydsjo G. (2019). Ment Health Young Mothers Single Mothers Their Child BMC Psychiatry. 2019;19(112):1–7.
Olajubu AO, Omoloye GO, Olajubu TO, Olowokere AE. Stress and resilience among pregnant teenagers in Ile-Ife, Nigeria. Eur J Midwifery. 2021;5.
Boakye-Yiadom A, Shittu SO, Dutt JB, Dapare PPM, Alhassan A. Perceived stress and anxiety among Ghanaian pregnant women. J Med Biomed Sci. 2015;4(2):29–37.
Article Google Scholar
Samsuddin SNA, Masroom MN, Wan Mohd Yunus WMA. Mental health of Muslim unwed pregnant teenagers. Malays J Med Health Sci. 2019;15(SUPP1):76–82.
Google Scholar
Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. 2013;139(1):213.
Hashmi S, Adolescence. An age of storm and stress. Rev Arts Humanit. 2013;2(1):19–33.
Traversy G, Chaput JP. Alcohol consumption and obesity: an update. Curr Obes Rep. 2015;4(1):122–30.
Elfenbein DS, Felice ME. Adolescent pregnancy. Pediatr Clin. 2003;50(4):781–800.
Dahmen B, Konrad K, Jahnen L, Herpertz-Dahlmann B, Firk C. Mental health of teenage mothers: impact on the next generation. Nervenarzt. 2019;90:243–50.
Article CAS PubMed Google Scholar
Steventon Roberts K, Smith C, Toska E, Cluver L, Haag K, Wittesaele C, et al. Risk factors for poor mental health among adolescent mothers in South Africa. Psychol Health Med. 2022;27(sup1):67–84.
Muzik M, McGinnis EW, Bocknek E, Morelen D, Rosenblum KL, Liberzon I, et al. PTSD symptoms across pregnancy and early postpartum among women with lifetime PTSD diagnosis. Depress Anxiety. 2016;33(7):584–91.
O’Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(4):388–406.
Enlow MB, Egeland B, Blood EA, Wright RO, Wright RJ. Interpersonal trauma exposure and cognitive development in children to age 8 years: a longitudinal study. J Epidemiol Community Health. 2012;66(11):1005–10.
Nkosi NN, Pretorius E. The influence of teenage pregnancy on education: perceptions of educators at a secondary school in Tembisa, Gauteng. Soc Work. 2019;55(1):108–16.
Panday S, Makiwane M, Ranchod C, Letsoala T. Teenage pregnancy in South Africa: with a specific focus on school-going learners. 2009.
Buchmann EJ, Mensah K, Pillay P. Legal termination of pregnancy among teenagers and older women in Soweto, 1999–2001. S Afr Med J. 2002;92(9):729–31.
CAS PubMed Google Scholar
Lamprecht C, Guetterman TC. Mixed methods in accounting: a field based analysis. Meditari Acc Res. 2019;27(6):921–38.
Seakamela KP, Mashaba RG, Ntimana CB, Mbombi MO, Tlouyamma J, Mphekgwana P, et al. Prevalence and associated factors of probable depression amongst pregnant and parenting young females: a comparison of adolescents and young adults in rural South Africa. Front Child Adolesc Psychiatry. 2023;2:1200759.
Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the Mental Health needs of pregnant and parenting adolescents. Pediatrics. 2014;133(1):114–22.
Patton GC, Sawyer SM, Santelli JS, Ross DA, Afifi R, Allen NB, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–78.
Osok J, Kigamwa P, Stoep AV, Huang KY, Kumar M. Depression and its psychosocial risk factors in pregnant Kenyan adolescents: a cross-sectional study in a community health centre of Nairobi. BMC Psychiatry. 2018;18(1):136.
Ntshayintshayi PN, Sehularo LA, Mokgaola IO, Sepeng NV. Exploring the psychosocial challenges faced by pregnant teenagers in Ditsobotla subdistrict. Health SA Gesondheid [Internet]. 2022 Nov 1 [cited 2023 Feb 12];27. Available from: http://www.hsag.co.za/index.php/hsag/article/view/1880 .
Van Zyl L, Van Der Merwe M, Chigeza S, ADOLESCENTS’ LIVED, EXPERIENCES OF THEIR PREGNANCY AND PARENTING IN A SEMI-RURAL COMMUNITY IN THE WESTERN CAPE. Soc Work Werk [Internet]. 2015 Jul 22 [cited 2023 Feb 12];51(2). Available from: http://socialwork.journals.ac.za/pub/article/view/439 .
Govender D, Naidoo S, Taylor M. Nurses’ perception of the multidisciplinary team approach of care for adolescent mothers and their children in Ugu, KwaZulu-Natal. Afr J Prim Health Care Fam Med [Internet]. 2019 Apr 23 [cited 2023 Feb 13];11(1). Available from: https://phcfm.org/index.php/phcfm/article/view/1936 .
Baney L, Greene A, Sherwood-Laughlin C, Beckmeyer J, Crawford BL, Jackson F, et al. “It was just really hard to be pregnant in a smaller town…”: Pregnant and parenting teenagers’ perspectives of social support in their rural communities. Int J Environ Res Public Health. 2022;19(24):16906.
Ntshayintshayi PN, Sehularo LA, Mokgaola IO, Sepeng NV. Exploring the psychosocial challenges faced by pregnant teenagers in Ditsobotla subdistrict. Health SA Gesondheid Online. 2022;27:1–8.
Istiqomah I. Positive negative affect and teen pregnancy. Proc Ser Soc Sci Humanit. 2021;2:29–34.
Chauhan. Teen Pregnancy-Physical, psychological and social aspects. Clin Pediatr. 2021;6(7 1000209).
Santos FM, Corseuil CHL. The effect of Bolsa Familia Program on mitigating adolescent school dropouts due to maternity: an area analysis. Int J Educ Dev. 2022;90:102575.
Rogers A, Obst S, Teague SJ, Rossen L, Spry EA, Macdonald JA, et al. Association between maternal perinatal depression and anxiety and child and adolescent development: a meta-analysis. JAMA Pediatr. 2020;174(11):1082–92.
Naidoo S, Taylor M, Govender D. Nurses’ perception of the multidisciplinary team approach of care for adolescent mothers and their children in Ugu, KwaZulu-Natal. Afr J Prim Health Care Fam Med. 2019;11(1):1–11.
Download references
Acknowledgements
We acknowledge the long-term financing by the South African Population Research Infrastructure Network (SAPRIN) which made it possible for the DIMAMO Population Health Research Centre to collect data in identified rural areas continuously. SAPRIN is an initiative of the South African Medical Research Council and receives long-term funding from the National Department of Science and Innovation.
The study was funded by the South African Population Research Infrastructure Network (SAPRIN) and the DSI-NRF Centre of Excellence, University of Witwatersrand, Maimela: DSI-NRF CoE.
Author information
Authors and affiliations.
Department of Nursing Science, University of Limpopo, SOVENGA, Private Bag X1106, Polokwane, 0727, South Africa
Livhuwani Muthelo & Masenyani Oupa Mbombi
Research Administration and Development, University of Limpopo, SOVENGA, Private Bag X1106, Polokwane, 0727, South Africa
Peter Mphekgwana
Department of Pharmacy, University of Limpopo, SOVENGA, Private Bag X1106, Polokwane, 0727, South Africa
Linneth Nkateko Mabila
Department of Geography and Environmental Studies, University of Limpopo, SOVENGA, Private Bag X1106, Polokwane, 0727, South Africa
Department of Computer Science, University of Limpopo, SOVENGA, Private Bag X1106, Polokwane, 0727, South Africa
Joseph Tlouyamma
DIMAMO Population Health Research Centre, University of Limpopo, SOVENGA, Private Bag X1106, Polokwane, 0727, South Africa
Reneilwe Given Mashaba, Katlego Mothapo, Cairo Bruce Ntimane, Kagiso Peace Seakamela & Rathani Nemuramba
Department of Public Health, University of Limpopo, Private Bag X1106, SOVENGA 0727, Polokwane, South Africa
Eric Maimela
Research Chair Mental Health, University of Limpopo, Private Bag X1106, Polokwane, 0727, SOVENGA, South Africa
Tholene Sodi
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: LM, MOM, PM, NLM, ID, JT, RN, RGM and KM; methodology, EM, RN, JT and PM formal analysis, PM, KM, JT and ID; investigation of MOM, LM, PM, ID, JT, RN, RGM, KM, and EM; writing—original draft preparation, MOM, LM, PM, ID, JT, RN, RGM, KM and EM writing review and editing, LM, PM, MOM, RN and TS visualization, MOM, LM, PM, ID, JT, RN, RGM, KM NLM and TS. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Livhuwani Muthelo .
Ethics declarations
Ethics approval and consent to participate.
The study was conducted following the Declaration of Helsinki guidelines. Ethical approval for this study was obtained from the Turfloop Research Ethics Committee (TREC) of the University of Limpopo (TREC/22/2022: PG) and the permission to conduct the study was sought from Department of Health Limpopo Province. The participants were informed about the aim and objectives of the study and that participation in the study was voluntary. All the participants who agreed to participate in the study were asked to sign a voluntary inform consent form. The participants who were below the age of 18 years, parents and guardians were consulted to sign the inform consent form.
Consent for publication
Not Appllicable.
Conflict of interest
The authors declare no conflict of interest
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Muthelo, L., Mbombi, M.O., Mphekgwana, P. et al. Exploring mental health problems and support needs among pregnant and parenting teenagers in rural areas Of Limpopo, South Africa. BMC Women's Health 24 , 236 (2024). https://doi.org/10.1186/s12905-024-03040-z
Download citation
Received : 04 March 2023
Accepted : 21 March 2024
Published : 13 April 2024
DOI : https://doi.org/10.1186/s12905-024-03040-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Spousal support
- Stigmatisation
- Teenage pregnancy
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Qual Stud Health Well-being
Methodology or method? A critical review of qualitative case study reports
Despite on-going debate about credibility, and reported limitations in comparison to other approaches, case study is an increasingly popular approach among qualitative researchers. We critically analysed the methodological descriptions of published case studies. Three high-impact qualitative methods journals were searched to locate case studies published in the past 5 years; 34 were selected for analysis. Articles were categorized as health and health services ( n= 12), social sciences and anthropology ( n= 7), or methods ( n= 15) case studies. The articles were reviewed using an adapted version of established criteria to determine whether adequate methodological justification was present, and if study aims, methods, and reported findings were consistent with a qualitative case study approach. Findings were grouped into five themes outlining key methodological issues: case study methodology or method, case of something particular and case selection, contextually bound case study, researcher and case interactions and triangulation, and study design inconsistent with methodology reported. Improved reporting of case studies by qualitative researchers will advance the methodology for the benefit of researchers and practitioners.
Case study research is an increasingly popular approach among qualitative researchers (Thomas, 2011 ). Several prominent authors have contributed to methodological developments, which has increased the popularity of case study approaches across disciplines (Creswell, 2013b ; Denzin & Lincoln, 2011b ; Merriam, 2009 ; Ragin & Becker, 1992 ; Stake, 1995 ; Yin, 2009 ). Current qualitative case study approaches are shaped by paradigm, study design, and selection of methods, and, as a result, case studies in the published literature vary. Differences between published case studies can make it difficult for researchers to define and understand case study as a methodology.
Experienced qualitative researchers have identified case study research as a stand-alone qualitative approach (Denzin & Lincoln, 2011b ). Case study research has a level of flexibility that is not readily offered by other qualitative approaches such as grounded theory or phenomenology. Case studies are designed to suit the case and research question and published case studies demonstrate wide diversity in study design. There are two popular case study approaches in qualitative research. The first, proposed by Stake ( 1995 ) and Merriam ( 2009 ), is situated in a social constructivist paradigm, whereas the second, by Yin ( 2012 ), Flyvbjerg ( 2011 ), and Eisenhardt ( 1989 ), approaches case study from a post-positivist viewpoint. Scholarship from both schools of inquiry has contributed to the popularity of case study and development of theoretical frameworks and principles that characterize the methodology.
The diversity of case studies reported in the published literature, and on-going debates about credibility and the use of case study in qualitative research practice, suggests that differences in perspectives on case study methodology may prevent researchers from developing a mutual understanding of practice and rigour. In addition, discussion about case study limitations has led some authors to query whether case study is indeed a methodology (Luck, Jackson, & Usher, 2006 ; Meyer, 2001 ; Thomas, 2010 ; Tight, 2010 ). Methodological discussion of qualitative case study research is timely, and a review is required to analyse and understand how this methodology is applied in the qualitative research literature. The aims of this study were to review methodological descriptions of published qualitative case studies, to review how the case study methodological approach was applied, and to identify issues that need to be addressed by researchers, editors, and reviewers. An outline of the current definitions of case study and an overview of the issues proposed in the qualitative methodological literature are provided to set the scene for the review.
Definitions of qualitative case study research
Case study research is an investigation and analysis of a single or collective case, intended to capture the complexity of the object of study (Stake, 1995 ). Qualitative case study research, as described by Stake ( 1995 ), draws together “naturalistic, holistic, ethnographic, phenomenological, and biographic research methods” in a bricoleur design, or in his words, “a palette of methods” (Stake, 1995 , pp. xi–xii). Case study methodology maintains deep connections to core values and intentions and is “particularistic, descriptive and heuristic” (Merriam, 2009 , p. 46).
As a study design, case study is defined by interest in individual cases rather than the methods of inquiry used. The selection of methods is informed by researcher and case intuition and makes use of naturally occurring sources of knowledge, such as people or observations of interactions that occur in the physical space (Stake, 1998 ). Thomas ( 2011 ) suggested that “analytical eclecticism” is a defining factor (p. 512). Multiple data collection and analysis methods are adopted to further develop and understand the case, shaped by context and emergent data (Stake, 1995 ). This qualitative approach “explores a real-life, contemporary bounded system (a case ) or multiple bounded systems (cases) over time, through detailed, in-depth data collection involving multiple sources of information … and reports a case description and case themes ” (Creswell, 2013b , p. 97). Case study research has been defined by the unit of analysis, the process of study, and the outcome or end product, all essentially the case (Merriam, 2009 ).
The case is an object to be studied for an identified reason that is peculiar or particular. Classification of the case and case selection procedures informs development of the study design and clarifies the research question. Stake ( 1995 ) proposed three types of cases and study design frameworks. These include the intrinsic case, the instrumental case, and the collective instrumental case. The intrinsic case is used to understand the particulars of a single case, rather than what it represents. An instrumental case study provides insight on an issue or is used to refine theory. The case is selected to advance understanding of the object of interest. A collective refers to an instrumental case which is studied as multiple, nested cases, observed in unison, parallel, or sequential order. More than one case can be simultaneously studied; however, each case study is a concentrated, single inquiry, studied holistically in its own entirety (Stake, 1995 , 1998 ).
Researchers who use case study are urged to seek out what is common and what is particular about the case. This involves careful and in-depth consideration of the nature of the case, historical background, physical setting, and other institutional and political contextual factors (Stake, 1998 ). An interpretive or social constructivist approach to qualitative case study research supports a transactional method of inquiry, where the researcher has a personal interaction with the case. The case is developed in a relationship between the researcher and informants, and presented to engage the reader, inviting them to join in this interaction and in case discovery (Stake, 1995 ). A postpositivist approach to case study involves developing a clear case study protocol with careful consideration of validity and potential bias, which might involve an exploratory or pilot phase, and ensures that all elements of the case are measured and adequately described (Yin, 2009 , 2012 ).
Current methodological issues in qualitative case study research
The future of qualitative research will be influenced and constructed by the way research is conducted, and by what is reviewed and published in academic journals (Morse, 2011 ). If case study research is to further develop as a principal qualitative methodological approach, and make a valued contribution to the field of qualitative inquiry, issues related to methodological credibility must be considered. Researchers are required to demonstrate rigour through adequate descriptions of methodological foundations. Case studies published without sufficient detail for the reader to understand the study design, and without rationale for key methodological decisions, may lead to research being interpreted as lacking in quality or credibility (Hallberg, 2013 ; Morse, 2011 ).
There is a level of artistic license that is embraced by qualitative researchers and distinguishes practice, which nurtures creativity, innovation, and reflexivity (Denzin & Lincoln, 2011b ; Morse, 2009 ). Qualitative research is “inherently multimethod” (Denzin & Lincoln, 2011a , p. 5); however, with this creative freedom, it is important for researchers to provide adequate description for methodological justification (Meyer, 2001 ). This includes paradigm and theoretical perspectives that have influenced study design. Without adequate description, study design might not be understood by the reader, and can appear to be dishonest or inaccurate. Reviewers and readers might be confused by the inconsistent or inappropriate terms used to describe case study research approach and methods, and be distracted from important study findings (Sandelowski, 2000 ). This issue extends beyond case study research, and others have noted inconsistencies in reporting of methodology and method by qualitative researchers. Sandelowski ( 2000 , 2010 ) argued for accurate identification of qualitative description as a research approach. She recommended that the selected methodology should be harmonious with the study design, and be reflected in methods and analysis techniques. Similarly, Webb and Kevern ( 2000 ) uncovered inconsistencies in qualitative nursing research with focus group methods, recommending that methodological procedures must cite seminal authors and be applied with respect to the selected theoretical framework. Incorrect labelling using case study might stem from the flexibility in case study design and non-directional character relative to other approaches (Rosenberg & Yates, 2007 ). Methodological integrity is required in design of qualitative studies, including case study, to ensure study rigour and to enhance credibility of the field (Morse, 2011 ).
Case study has been unnecessarily devalued by comparisons with statistical methods (Eisenhardt, 1989 ; Flyvbjerg, 2006 , 2011 ; Jensen & Rodgers, 2001 ; Piekkari, Welch, & Paavilainen, 2009 ; Tight, 2010 ; Yin, 1999 ). It is reputed to be the “the weak sibling” in comparison to other, more rigorous, approaches (Yin, 2009 , p. xiii). Case study is not an inherently comparative approach to research. The objective is not statistical research, and the aim is not to produce outcomes that are generalizable to all populations (Thomas, 2011 ). Comparisons between case study and statistical research do little to advance this qualitative approach, and fail to recognize its inherent value, which can be better understood from the interpretive or social constructionist viewpoint of other authors (Merriam, 2009 ; Stake, 1995 ). Building on discussions relating to “fuzzy” (Bassey, 2001 ), or naturalistic generalizations (Stake, 1978 ), or transference of concepts and theories (Ayres, Kavanaugh, & Knafl, 2003 ; Morse et al., 2011 ) would have more relevance.
Case study research has been used as a catch-all design to justify or add weight to fundamental qualitative descriptive studies that do not fit with other traditional frameworks (Merriam, 2009 ). A case study has been a “convenient label for our research—when we ‘can't think of anything ‘better”—in an attempt to give it [qualitative methodology] some added respectability” (Tight, 2010 , p. 337). Qualitative case study research is a pliable approach (Merriam, 2009 ; Meyer, 2001 ; Stake, 1995 ), and has been likened to a “curious methodological limbo” (Gerring, 2004 , p. 341) or “paradigmatic bridge” (Luck et al., 2006 , p. 104), that is on the borderline between postpositivist and constructionist interpretations. This has resulted in inconsistency in application, which indicates that flexibility comes with limitations (Meyer, 2001 ), and the open nature of case study research might be off-putting to novice researchers (Thomas, 2011 ). The development of a well-(in)formed theoretical framework to guide a case study should improve consistency, rigour, and trust in studies published in qualitative research journals (Meyer, 2001 ).
Assessment of rigour
The purpose of this study was to analyse the methodological descriptions of case studies published in qualitative methods journals. To do this we needed to develop a suitable framework, which used existing, established criteria for appraising qualitative case study research rigour (Creswell, 2013b ; Merriam, 2009 ; Stake, 1995 ). A number of qualitative authors have developed concepts and criteria that are used to determine whether a study is rigorous (Denzin & Lincoln, 2011b ; Lincoln, 1995 ; Sandelowski & Barroso, 2002 ). The criteria proposed by Stake ( 1995 ) provide a framework for readers and reviewers to make judgements regarding case study quality, and identify key characteristics essential for good methodological rigour. Although each of the factors listed in Stake's criteria could enhance the quality of a qualitative research report, in Table I we present an adapted criteria used in this study, which integrates more recent work by Merriam ( 2009 ) and Creswell ( 2013b ). Stake's ( 1995 ) original criteria were separated into two categories. The first list of general criteria is “relevant for all qualitative research.” The second list, “high relevance to qualitative case study research,” was the criteria that we decided had higher relevance to case study research. This second list was the main criteria used to assess the methodological descriptions of the case studies reviewed. The complete table has been preserved so that the reader can determine how the original criteria were adapted.
Framework for assessing quality in qualitative case study research.
Adapted from Stake ( 1995 , p. 131).
Study design
The critical review method described by Grant and Booth ( 2009 ) was used, which is appropriate for the assessment of research quality, and is used for literature analysis to inform research and practice. This type of review goes beyond the mapping and description of scoping or rapid reviews, to include “analysis and conceptual innovation” (Grant & Booth, 2009 , p. 93). A critical review is used to develop existing, or produce new, hypotheses or models. This is different to systematic reviews that answer clinical questions. It is used to evaluate existing research and competing ideas, to provide a “launch pad” for conceptual development and “subsequent testing” (Grant & Booth, 2009 , p. 93).
Qualitative methods journals were located by a search of the 2011 ISI Journal Citation Reports in Social Science, via the database Web of Knowledge (see m.webofknowledge.com). No “qualitative research methods” category existed in the citation reports; therefore, a search of all categories was performed using the term “qualitative.” In Table II , we present the qualitative methods journals located, ranked by impact factor. The highest ranked journals were selected for searching. We acknowledge that the impact factor ranking system might not be the best measure of journal quality (Cheek, Garnham, & Quan, 2006 ); however, this was the most appropriate and accessible method available.
International Journal of Qualitative Studies on Health and Well-being.
Search strategy
In March 2013, searches of the journals, Qualitative Health Research , Qualitative Research , and Qualitative Inquiry were completed to retrieve studies with “case study” in the abstract field. The search was limited to the past 5 years (1 January 2008 to 1 March 2013). The objective was to locate published qualitative case studies suitable for assessment using the adapted criterion. Viewpoints, commentaries, and other article types were excluded from review. Title and abstracts of the 45 retrieved articles were read by the first author, who identified 34 empirical case studies for review. All authors reviewed the 34 studies to confirm selection and categorization. In Table III , we present the 34 case studies grouped by journal, and categorized by research topic, including health sciences, social sciences and anthropology, and methods research. There was a discrepancy in categorization of one article on pedagogy and a new teaching method published in Qualitative Inquiry (Jorrín-Abellán, Rubia-Avi, Anguita-Martínez, Gómez-Sánchez, & Martínez-Mones, 2008 ). Consensus was to allocate to the methods category.
Outcomes of search of qualitative methods journals.
In Table III , the number of studies located, and final numbers selected for review have been reported. Qualitative Health Research published the most empirical case studies ( n= 16). In the health category, there were 12 case studies of health conditions, health services, and health policy issues, all published in Qualitative Health Research . Seven case studies were categorized as social sciences and anthropology research, which combined case study with biography and ethnography methodologies. All three journals published case studies on methods research to illustrate a data collection or analysis technique, methodological procedure, or related issue.
The methodological descriptions of 34 case studies were critically reviewed using the adapted criteria. All articles reviewed contained a description of study methods; however, the length, amount of detail, and position of the description in the article varied. Few studies provided an accurate description and rationale for using a qualitative case study approach. In the 34 case studies reviewed, three described a theoretical framework informed by Stake ( 1995 ), two by Yin ( 2009 ), and three provided a mixed framework informed by various authors, which might have included both Yin and Stake. Few studies described their case study design, or included a rationale that explained why they excluded or added further procedures, and whether this was to enhance the study design, or to better suit the research question. In 26 of the studies no reference was provided to principal case study authors. From reviewing the description of methods, few authors provided a description or justification of case study methodology that demonstrated how their study was informed by the methodological literature that exists on this approach.
The methodological descriptions of each study were reviewed using the adapted criteria, and the following issues were identified: case study methodology or method; case of something particular and case selection; contextually bound case study; researcher and case interactions and triangulation; and, study design inconsistent with methodology. An outline of how the issues were developed from the critical review is provided, followed by a discussion of how these relate to the current methodological literature.
Case study methodology or method
A third of the case studies reviewed appeared to use a case report method, not case study methodology as described by principal authors (Creswell, 2013b ; Merriam, 2009 ; Stake, 1995 ; Yin, 2009 ). Case studies were identified as a case report because of missing methodological detail and by review of the study aims and purpose. These reports presented data for small samples of no more than three people, places or phenomenon. Four studies, or “case reports” were single cases selected retrospectively from larger studies (Bronken, Kirkevold, Martinsen, & Kvigne, 2012 ; Coltart & Henwood, 2012 ; Hooghe, Neimeyer, & Rober, 2012 ; Roscigno et al., 2012 ). Case reports were not a case of something, instead were a case demonstration or an example presented in a report. These reports presented outcomes, and reported on how the case could be generalized. Descriptions focussed on the phenomena, rather than the case itself, and did not appear to study the case in its entirety.
Case reports had minimal in-text references to case study methodology, and were informed by other qualitative traditions or secondary sources (Adamson & Holloway, 2012 ; Buzzanell & D'Enbeau, 2009 ; Nagar-Ron & Motzafi-Haller, 2011 ). This does not suggest that case study methodology cannot be multimethod, however, methodology should be consistent in design, be clearly described (Meyer, 2001 ; Stake, 1995 ), and maintain focus on the case (Creswell, 2013b ).
To demonstrate how case reports were identified, three examples are provided. The first, Yeh ( 2013 ) described their study as, “the examination of the emergence of vegetarianism in Victorian England serves as a case study to reveal the relationships between boundaries and entities” (p. 306). The findings were a historical case report, which resulted from an ethnographic study of vegetarianism. Cunsolo Willox, Harper, Edge, ‘My Word’: Storytelling and Digital Media Lab, and Rigolet Inuit Community Government (2013) used “a case study that illustrates the usage of digital storytelling within an Inuit community” (p. 130). This case study reported how digital storytelling can be used with indigenous communities as a participatory method to illuminate the benefits of this method for other studies. This “case study was conducted in the Inuit community” but did not include the Inuit community in case analysis (Cunsolo Willox et al., 2013 , p. 130). Bronken et al. ( 2012 ) provided a single case report to demonstrate issues observed in a larger clinical study of aphasia and stroke, without adequate case description or analysis.
Case study of something particular and case selection
Case selection is a precursor to case analysis, which needs to be presented as a convincing argument (Merriam, 2009 ). Descriptions of the case were often not adequate to ascertain why the case was selected, or whether it was a particular exemplar or outlier (Thomas, 2011 ). In a number of case studies in the health and social science categories, it was not explicit whether the case was of something particular, or peculiar to their discipline or field (Adamson & Holloway, 2012 ; Bronken et al., 2012 ; Colón-Emeric et al., 2010 ; Jackson, Botelho, Welch, Joseph, & Tennstedt, 2012 ; Mawn et al., 2010 ; Snyder-Young, 2011 ). There were exceptions in the methods category ( Table III ), where cases were selected by researchers to report on a new or innovative method. The cases emerged through heuristic study, and were reported to be particular, relative to the existing methods literature (Ajodhia-Andrews & Berman, 2009 ; Buckley & Waring, 2013 ; Cunsolo Willox et al., 2013 ; De Haene, Grietens, & Verschueren, 2010 ; Gratton & O'Donnell, 2011 ; Sumsion, 2013 ; Wimpenny & Savin-Baden, 2012 ).
Case selection processes were sometimes insufficient to understand why the case was selected from the global population of cases, or what study of this case would contribute to knowledge as compared with other possible cases (Adamson & Holloway, 2012 ; Bronken et al., 2012 ; Colón-Emeric et al., 2010 ; Jackson et al., 2012 ; Mawn et al., 2010 ). In two studies, local cases were selected (Barone, 2010 ; Fourie & Theron, 2012 ) because the researcher was familiar with and had access to the case. Possible limitations of a convenience sample were not acknowledged. Purposeful sampling was used to recruit participants within the case of one study, but not of the case itself (Gallagher et al., 2013 ). Random sampling was completed for case selection in two studies (Colón-Emeric et al., 2010 ; Jackson et al., 2012 ), which has limited meaning in interpretive qualitative research.
To demonstrate how researchers provided a good justification for the selection of case study approaches, four examples are provided. The first, cases of residential care homes, were selected because of reported occurrences of mistreatment, which included residents being locked in rooms at night (Rytterström, Unosson, & Arman, 2013 ). Roscigno et al. ( 2012 ) selected cases of parents who were admitted for early hospitalization in neonatal intensive care with a threatened preterm delivery before 26 weeks. Hooghe et al. ( 2012 ) used random sampling to select 20 couples that had experienced the death of a child; however, the case study was of one couple and a particular metaphor described only by them. The final example, Coltart and Henwood ( 2012 ), provided a detailed account of how they selected two cases from a sample of 46 fathers based on personal characteristics and beliefs. They described how the analysis of the two cases would contribute to their larger study on first time fathers and parenting.
Contextually bound case study
The limits or boundaries of the case are a defining factor of case study methodology (Merriam, 2009 ; Ragin & Becker, 1992 ; Stake, 1995 ; Yin, 2009 ). Adequate contextual description is required to understand the setting or context in which the case is revealed. In the health category, case studies were used to illustrate a clinical phenomenon or issue such as compliance and health behaviour (Colón-Emeric et al., 2010 ; D'Enbeau, Buzzanell, & Duckworth, 2010 ; Gallagher et al., 2013 ; Hooghe et al., 2012 ; Jackson et al., 2012 ; Roscigno et al., 2012 ). In these case studies, contextual boundaries, such as physical and institutional descriptions, were not sufficient to understand the case as a holistic system, for example, the general practitioner (GP) clinic in Gallagher et al. ( 2013 ), or the nursing home in Colón-Emeric et al. ( 2010 ). Similarly, in the social science and methods categories, attention was paid to some components of the case context, but not others, missing important information required to understand the case as a holistic system (Alexander, Moreira, & Kumar, 2012 ; Buzzanell & D'Enbeau, 2009 ; Nairn & Panelli, 2009 ; Wimpenny & Savin-Baden, 2012 ).
In two studies, vicarious experience or vignettes (Nairn & Panelli, 2009 ) and images (Jorrín-Abellán et al., 2008 ) were effective to support description of context, and might have been a useful addition for other case studies. Missing contextual boundaries suggests that the case might not be adequately defined. Additional information, such as the physical, institutional, political, and community context, would improve understanding of the case (Stake, 1998 ). In Boxes 1 and 2 , we present brief synopses of two studies that were reviewed, which demonstrated a well bounded case. In Box 1 , Ledderer ( 2011 ) used a qualitative case study design informed by Stake's tradition. In Box 2 , Gillard, Witt, and Watts ( 2011 ) were informed by Yin's tradition. By providing a brief outline of the case studies in Boxes 1 and 2 , we demonstrate how effective case boundaries can be constructed and reported, which may be of particular interest to prospective case study researchers.
Article synopsis of case study research using Stake's tradition
Ledderer ( 2011 ) used a qualitative case study research design, informed by modern ethnography. The study is bounded to 10 general practice clinics in Denmark, who had received federal funding to implement preventative care services based on a Motivational Interviewing intervention. The researcher question focussed on “why is it so difficult to create change in medical practice?” (Ledderer, 2011 , p. 27). The study context was adequately described, providing detail on the general practitioner (GP) clinics and relevant political and economic influences. Methodological decisions are described in first person narrative, providing insight on researcher perspectives and interaction with the case. Forty-four interviews were conducted, which focussed on how GPs conducted consultations, and the form, nature and content, rather than asking their opinion or experience (Ledderer, 2011 , p. 30). The duration and intensity of researcher immersion in the case enhanced depth of description and trustworthiness of study findings. Analysis was consistent with Stake's tradition, and the researcher provided examples of inquiry techniques used to challenge assumptions about emerging themes. Several other seminal qualitative works were cited. The themes and typology constructed are rich in narrative data and storytelling by clinic staff, demonstrating individual clinic experiences as well as shared meanings and understandings about changing from a biomedical to psychological approach to preventative health intervention. Conclusions make note of social and cultural meanings and lessons learned, which might not have been uncovered using a different methodology.
Article synopsis of case study research using Yin's tradition
Gillard et al. ( 2011 ) study of camps for adolescents living with HIV/AIDs provided a good example of Yin's interpretive case study approach. The context of the case is bounded by the three summer camps of which the researchers had prior professional involvement. A case study protocol was developed that used multiple methods to gather information at three data collection points coinciding with three youth camps (Teen Forum, Discover Camp, and Camp Strong). Gillard and colleagues followed Yin's ( 2009 ) principles, using a consistent data protocol that enhanced cross-case analysis. Data described the young people, the camp physical environment, camp schedule, objectives and outcomes, and the staff of three youth camps. The findings provided a detailed description of the context, with less detail of individual participants, including insight into researcher's interpretations and methodological decisions throughout the data collection and analysis process. Findings provided the reader with a sense of “being there,” and are discovered through constant comparison of the case with the research issues; the case is the unit of analysis. There is evidence of researcher immersion in the case, and Gillard reports spending significant time in the field in a naturalistic and integrated youth mentor role.
This case study is not intended to have a significant impact on broader health policy, although does have implications for health professionals working with adolescents. Study conclusions will inform future camps for young people with chronic disease, and practitioners are able to compare similarities between this case and their own practice (for knowledge translation). No limitations of this article were reported. Limitations related to publication of this case study were that it was 20 pages long and used three tables to provide sufficient description of the camp and program components, and relationships with the research issue.
Researcher and case interactions and triangulation
Researcher and case interactions and transactions are a defining feature of case study methodology (Stake, 1995 ). Narrative stories, vignettes, and thick description are used to provoke vicarious experience and a sense of being there with the researcher in their interaction with the case. Few of the case studies reviewed provided details of the researcher's relationship with the case, researcher–case interactions, and how these influenced the development of the case study (Buzzanell & D'Enbeau, 2009 ; D'Enbeau et al., 2010 ; Gallagher et al., 2013 ; Gillard et al., 2011 ; Ledderer, 2011 ; Nagar-Ron & Motzafi-Haller, 2011 ). The role and position of the researcher needed to be self-examined and understood by readers, to understand how this influenced interactions with participants, and to determine what triangulation is needed (Merriam, 2009 ; Stake, 1995 ).
Gillard et al. ( 2011 ) provided a good example of triangulation, comparing data sources in a table (p. 1513). Triangulation of sources was used to reveal as much depth as possible in the study by Nagar-Ron and Motzafi-Haller ( 2011 ), while also enhancing confirmation validity. There were several case studies that would have benefited from improved range and use of data sources, and descriptions of researcher–case interactions (Ajodhia-Andrews & Berman, 2009 ; Bronken et al., 2012 ; Fincham, Scourfield, & Langer, 2008 ; Fourie & Theron, 2012 ; Hooghe et al., 2012 ; Snyder-Young, 2011 ; Yeh, 2013 ).
Study design inconsistent with methodology
Good, rigorous case studies require a strong methodological justification (Meyer, 2001 ) and a logical and coherent argument that defines paradigm, methodological position, and selection of study methods (Denzin & Lincoln, 2011b ). Methodological justification was insufficient in several of the studies reviewed (Barone, 2010 ; Bronken et al., 2012 ; Hooghe et al., 2012 ; Mawn et al., 2010 ; Roscigno et al., 2012 ; Yeh, 2013 ). This was judged by the absence, or inadequate or inconsistent reference to case study methodology in-text.
In six studies, the methodological justification provided did not relate to case study. There were common issues identified. Secondary sources were used as primary methodological references indicating that study design might not have been theoretically sound (Colón-Emeric et al., 2010 ; Coltart & Henwood, 2012 ; Roscigno et al., 2012 ; Snyder-Young, 2011 ). Authors and sources cited in methodological descriptions were inconsistent with the actual study design and practices used (Fourie & Theron, 2012 ; Hooghe et al., 2012 ; Jorrín-Abellán et al., 2008 ; Mawn et al., 2010 ; Rytterström et al., 2013 ; Wimpenny & Savin-Baden, 2012 ). This occurred when researchers cited Stake or Yin, or both (Mawn et al., 2010 ; Rytterström et al., 2013 ), although did not follow their paradigmatic or methodological approach. In 26 studies there were no citations for a case study methodological approach.
The findings of this study have highlighted a number of issues for researchers. A considerable number of case studies reviewed were missing key elements that define qualitative case study methodology and the tradition cited. A significant number of studies did not provide a clear methodological description or justification relevant to case study. Case studies in health and social sciences did not provide sufficient information for the reader to understand case selection, and why this case was chosen above others. The context of the cases were not described in adequate detail to understand all relevant elements of the case context, which indicated that cases may have not been contextually bounded. There were inconsistencies between reported methodology, study design, and paradigmatic approach in case studies reviewed, which made it difficult to understand the study methodology and theoretical foundations. These issues have implications for methodological integrity and honesty when reporting study design, which are values of the qualitative research tradition and are ethical requirements (Wager & Kleinert, 2010a ). Poorly described methodological descriptions may lead the reader to misinterpret or discredit study findings, which limits the impact of the study, and, as a collective, hinders advancements in the broader qualitative research field.
The issues highlighted in our review build on current debates in the case study literature, and queries about the value of this methodology. Case study research can be situated within different paradigms or designed with an array of methods. In order to maintain the creativity and flexibility that is valued in this methodology, clearer descriptions of paradigm and theoretical position and methods should be provided so that study findings are not undervalued or discredited. Case study research is an interdisciplinary practice, which means that clear methodological descriptions might be more important for this approach than other methodologies that are predominantly driven by fewer disciplines (Creswell, 2013b ).
Authors frequently omit elements of methodologies and include others to strengthen study design, and we do not propose a rigid or purist ideology in this paper. On the contrary, we encourage new ideas about using case study, together with adequate reporting, which will advance the value and practice of case study. The implications of unclear methodological descriptions in the studies reviewed were that study design appeared to be inconsistent with reported methodology, and key elements required for making judgements of rigour were missing. It was not clear whether the deviations from methodological tradition were made by researchers to strengthen the study design, or because of misinterpretations. Morse ( 2011 ) recommended that innovations and deviations from practice are best made by experienced researchers, and that a novice might be unaware of the issues involved with making these changes. To perpetuate the tradition of case study research, applications in the published literature should have consistencies with traditional methodological constructions, and deviations should be described with a rationale that is inherent in study conduct and findings. Providing methodological descriptions that demonstrate a strong theoretical foundation and coherent study design will add credibility to the study, while ensuring the intrinsic meaning of case study is maintained.
The value of this review is that it contributes to discussion of whether case study is a methodology or method. We propose possible reasons why researchers might make this misinterpretation. Researchers may interchange the terms methods and methodology, and conduct research without adequate attention to epistemology and historical tradition (Carter & Little, 2007 ; Sandelowski, 2010 ). If the rich meaning that naming a qualitative methodology brings to the study is not recognized, a case study might appear to be inconsistent with the traditional approaches described by principal authors (Creswell, 2013a ; Merriam, 2009 ; Stake, 1995 ; Yin, 2009 ). If case studies are not methodologically and theoretically situated, then they might appear to be a case report.
Case reports are promoted by university and medical journals as a method of reporting on medical or scientific cases; guidelines for case reports are publicly available on websites ( http://www.hopkinsmedicine.org/institutional_review_board/guidelines_policies/guidelines/case_report.html ). The various case report guidelines provide a general criteria for case reports, which describes that this form of report does not meet the criteria of research, is used for retrospective analysis of up to three clinical cases, and is primarily illustrative and for educational purposes. Case reports can be published in academic journals, but do not require approval from a human research ethics committee. Traditionally, case reports describe a single case, to explain how and what occurred in a selected setting, for example, to illustrate a new phenomenon that has emerged from a larger study. A case report is not necessarily particular or the study of a case in its entirety, and the larger study would usually be guided by a different research methodology.
This description of a case report is similar to what was provided in some studies reviewed. This form of report lacks methodological grounding and qualities of research rigour. The case report has publication value in demonstrating an example and for dissemination of knowledge (Flanagan, 1999 ). However, case reports have different meaning and purpose to case study, which needs to be distinguished. Findings of our review suggest that the medical understanding of a case report has been confused with qualitative case study approaches.
In this review, a number of case studies did not have methodological descriptions that included key characteristics of case study listed in the adapted criteria, and several issues have been discussed. There have been calls for improvements in publication quality of qualitative research (Morse, 2011 ), and for improvements in peer review of submitted manuscripts (Carter & Little, 2007 ; Jasper, Vaismoradi, Bondas, & Turunen, 2013 ). The challenging nature of editor and reviewers responsibilities are acknowledged in the literature (Hames, 2013 ; Wager & Kleinert, 2010b ); however, review of case study methodology should be prioritized because of disputes on methodological value.
Authors using case study approaches are recommended to describe their theoretical framework and methods clearly, and to seek and follow specialist methodological advice when needed (Wager & Kleinert, 2010a ). Adequate page space for case study description would contribute to better publications (Gillard et al., 2011 ). Capitalizing on the ability to publish complementary resources should be considered.
Limitations of the review
There is a level of subjectivity involved in this type of review and this should be considered when interpreting study findings. Qualitative methods journals were selected because the aims and scope of these journals are to publish studies that contribute to methodological discussion and development of qualitative research. Generalist health and social science journals were excluded that might have contained good quality case studies. Journals in business or education were also excluded, although a review of case studies in international business journals has been published elsewhere (Piekkari et al., 2009 ).
The criteria used to assess the quality of the case studies were a set of qualitative indicators. A numerical or ranking system might have resulted in different results. Stake's ( 1995 ) criteria have been referenced elsewhere, and was deemed the best available (Creswell, 2013b ; Crowe et al., 2011 ). Not all qualitative studies are reported in a consistent way and some authors choose to report findings in a narrative form in comparison to a typical biomedical report style (Sandelowski & Barroso, 2002 ), if misinterpretations were made this may have affected the review.
Case study research is an increasingly popular approach among qualitative researchers, which provides methodological flexibility through the incorporation of different paradigmatic positions, study designs, and methods. However, whereas flexibility can be an advantage, a myriad of different interpretations has resulted in critics questioning the use of case study as a methodology. Using an adaptation of established criteria, we aimed to identify and assess the methodological descriptions of case studies in high impact, qualitative methods journals. Few articles were identified that applied qualitative case study approaches as described by experts in case study design. There were inconsistencies in methodology and study design, which indicated that researchers were confused whether case study was a methodology or a method. Commonly, there appeared to be confusion between case studies and case reports. Without clear understanding and application of the principles and key elements of case study methodology, there is a risk that the flexibility of the approach will result in haphazard reporting, and will limit its global application as a valuable, theoretically supported methodology that can be rigorously applied across disciplines and fields.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
- Adamson S, Holloway M. Negotiating sensitivities and grappling with intangibles: Experiences from a study of spirituality and funerals. Qualitative Research. 2012; 12 (6):735–752. doi: 10.1177/1468794112439008. [ CrossRef ] [ Google Scholar ]
- Ajodhia-Andrews A, Berman R. Exploring school life from the lens of a child who does not use speech to communicate. Qualitative Inquiry. 2009; 15 (5):931–951. doi: 10.1177/1077800408322789. [ CrossRef ] [ Google Scholar ]
- Alexander B. K, Moreira C, Kumar H. S. Resisting (resistance) stories: A tri-autoethnographic exploration of father narratives across shades of difference. Qualitative Inquiry. 2012; 18 (2):121–133. doi: 10.1177/1077800411429087. [ CrossRef ] [ Google Scholar ]
- Austin W, Park C, Goble E. From interdisciplinary to transdisciplinary research: A case study. Qualitative Health Research. 2008; 18 (4):557–564. doi: 10.1177/1049732307308514. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ayres L, Kavanaugh K, Knafl K. A. Within-case and across-case approaches to qualitative data analysis. Qualitative Health Research. 2003; 13 (6):871–883. doi: 10.1177/1049732303013006008. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barone T. L. Culturally sensitive care 1969–2000: The Indian Chicano Health Center. Qualitative Health Research. 2010; 20 (4):453–464. doi: 10.1177/1049732310361893. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bassey M. A solution to the problem of generalisation in educational research: Fuzzy prediction. Oxford Review of Education. 2001; 27 (1):5–22. doi: 10.1080/03054980123773. [ CrossRef ] [ Google Scholar ]
- Bronken B. A, Kirkevold M, Martinsen R, Kvigne K. The aphasic storyteller: Coconstructing stories to promote psychosocial well-being after stroke. Qualitative Health Research. 2012; 22 (10):1303–1316. doi: 10.1177/1049732312450366. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Broyles L. M, Rodriguez K. L, Price P. A, Bayliss N. K, Sevick M. A. Overcoming barriers to the recruitment of nurses as participants in health care research. Qualitative Health Research. 2011; 21 (12):1705–1718. doi: 10.1177/1049732311417727. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Buckley C. A, Waring M. J. Using diagrams to support the research process: Examples from grounded theory. Qualitative Research. 2013; 13 (2):148–172. doi: 10.1177/1468794112472280. [ CrossRef ] [ Google Scholar ]
- Buzzanell P. M, D'Enbeau S. Stories of caregiving: Intersections of academic research and women's everyday experiences. Qualitative Inquiry. 2009; 15 (7):1199–1224. doi: 10.1177/1077800409338025. [ CrossRef ] [ Google Scholar ]
- Carter S. M, Little M. Justifying knowledge, justifying method, taking action: Epistemologies, methodologies, and methods in qualitative research. Qualitative Health Research. 2007; 17 (10):1316–1328. doi: 10.1177/1049732307306927. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cheek J, Garnham B, Quan J. What's in a number? Issues in providing evidence of impact and quality of research(ers) Qualitative Health Research. 2006; 16 (3):423–435. doi: 10.1177/1049732305285701. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Colón-Emeric C. S, Plowman D, Bailey D, Corazzini K, Utley-Smith Q, Ammarell N, et al. Regulation and mindful resident care in nursing homes. Qualitative Health Research. 2010; 20 (9):1283–1294. doi: 10.1177/1049732310369337. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coltart C, Henwood K. On paternal subjectivity: A qualitative longitudinal and psychosocial case analysis of men's classed positions and transitions to first-time fatherhood. Qualitative Research. 2012; 12 (1):35–52. doi: 10.1177/1468794111426224. [ CrossRef ] [ Google Scholar ]
- Creswell J. W. Five qualitative approaches to inquiry. In: Creswell J. W, editor. Qualitative inquiry and research design: Choosing among five approaches. 3rd ed. Thousand Oaks, CA: Sage; 2013a. pp. 53–84. [ Google Scholar ]
- Creswell J. W. Qualitative inquiry and research design: Choosing among five approaches. 3rd ed. Thousand Oaks, CA: Sage; 2013b. [ Google Scholar ]
- Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach. BMC Medical Research Methodology. 2011; 11 (1):1–9. doi: 10.1186/1471-2288-11-100. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cunsolo Willox A, Harper S. L, Edge V. L, ‘My Word’: Storytelling and Digital Media Lab, & Rigolet Inuit Community Government Storytelling in a digital age: Digital storytelling as an emerging narrative method for preserving and promoting indigenous oral wisdom. Qualitative Research. 2013; 13 (2):127–147. doi: 10.1177/1468794112446105. [ CrossRef ] [ Google Scholar ]
- De Haene L, Grietens H, Verschueren K. Holding harm: Narrative methods in mental health research on refugee trauma. Qualitative Health Research. 2010; 20 (12):1664–1676. doi: 10.1177/1049732310376521. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- D'Enbeau S, Buzzanell P. M, Duckworth J. Problematizing classed identities in fatherhood: Development of integrative case studies for analysis and praxis. Qualitative Inquiry. 2010; 16 (9):709–720. doi: 10.1177/1077800410374183. [ CrossRef ] [ Google Scholar ]
- Denzin N. K, Lincoln Y. S. Introduction: Disciplining the practice of qualitative research. In: Denzin N. K, Lincoln Y. S, editors. The SAGE handbook of qualitative research. 4th ed. Thousand Oaks, CA: Sage; 2011a. pp. 1–6. [ Google Scholar ]
- Denzin N. K, Lincoln Y. S, editors. The SAGE handbook of qualitative research. 4th ed. Thousand Oaks, CA: Sage; 2011b. [ Google Scholar ]
- Edwards R, Weller S. Shifting analytic ontology: Using I-poems in qualitative longitudinal research. Qualitative Research. 2012; 12 (2):202–217. doi: 10.1177/1468794111422040. [ CrossRef ] [ Google Scholar ]
- Eisenhardt K. M. Building theories from case study research. The Academy of Management Review. 1989; 14 (4):532–550. doi: 10.2307/258557. [ CrossRef ] [ Google Scholar ]
- Fincham B, Scourfield J, Langer S. The impact of working with disturbing secondary data: Reading suicide files in a coroner's office. Qualitative Health Research. 2008; 18 (6):853–862. doi: 10.1177/1049732307308945. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flanagan J. Public participation in the design of educational programmes for cancer nurses: A case report. European Journal of Cancer Care. 1999; 8 (2):107–112. doi: 10.1046/j.1365-2354.1999.00141.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Flyvbjerg B. Five misunderstandings about case-study research. Qualitative Inquiry. 2006; 12 (2):219–245. doi: 10.1177/1077800405284.363. [ CrossRef ] [ Google Scholar ]
- Flyvbjerg B. Case study. In: Denzin N. K, Lincoln Y. S, editors. The SAGE handbook of qualitative research. 4th ed. Thousand Oaks, CA: Sage; 2011. pp. 301–316. [ Google Scholar ]
- Fourie C. L, Theron L. C. Resilience in the face of fragile X syndrome. Qualitative Health Research. 2012; 22 (10):1355–1368. doi: 10.1177/1049732312451871. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gallagher N, MacFarlane A, Murphy A. W, Freeman G. K, Glynn L. G, Bradley C. P. Service users’ and caregivers’ perspectives on continuity of care in out-of-hours primary care. Qualitative Health Research. 2013; 23 (3):407–421. doi: 10.1177/1049732312470521. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gerring J. What is a case study and what is it good for? American Political Science Review. 2004; 98 (2):341–354. doi: 10.1017/S0003055404001182. [ CrossRef ] [ Google Scholar ]
- Gillard A, Witt P. A, Watts C. E. Outcomes and processes at a camp for youth with HIV/AIDS. Qualitative Health Research. 2011; 21 (11):1508–1526. doi: 10.1177/1049732311413907. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Grant M, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information and Libraries Journal. 2009; 26 :91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gratton M.-F, O'Donnell S. Communication technologies for focus groups with remote communities: A case study of research with First Nations in Canada. Qualitative Research. 2011; 11 (2):159–175. doi: 10.1177/1468794110394068. [ CrossRef ] [ Google Scholar ]
- Hallberg L. Quality criteria and generalization of results from qualitative studies. International Journal of Qualitative Studies on Health and Wellbeing. 2013; 8 :1. doi: 10.3402/qhw.v8i0.20647. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hames I. Committee on Publication Ethics, 1. 2013, March. COPE Ethical guidelines for peer reviewers. Retrieved April 7, 2013, from http://publicationethics.org/resources/guidelines . [ Google Scholar ]
- Hooghe A, Neimeyer R. A, Rober P. “Cycling around an emotional core of sadness”: Emotion regulation in a couple after the loss of a child. Qualitative Health Research. 2012; 22 (9):1220–1231. doi: 10.1177/1049732312449209. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jackson C. B, Botelho E. M, Welch L. C, Joseph J, Tennstedt S. L. Talking with others about stigmatized health conditions: Implications for managing symptoms. Qualitative Health Research. 2012; 22 (11):1468–1475. doi: 10.1177/1049732312450323. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jasper M, Vaismoradi M, Bondas T, Turunen H. Validity and reliability of the scientific review process in nursing journals—time for a rethink? Nursing Inquiry. 2013 doi: 10.1111/nin.12030. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jensen J. L, Rodgers R. Cumulating the intellectual gold of case study research. Public Administration Review. 2001; 61 (2):235–246. doi: 10.1111/0033-3352.00025. [ CrossRef ] [ Google Scholar ]
- Jorrín-Abellán I. M, Rubia-Avi B, Anguita-Martínez R, Gómez-Sánchez E, Martínez-Mones A. Bouncing between the dark and bright sides: Can technology help qualitative research? Qualitative Inquiry. 2008; 14 (7):1187–1204. doi: 10.1177/1077800408318435. [ CrossRef ] [ Google Scholar ]
- Ledderer L. Understanding change in medical practice: The role of shared meaning in preventive treatment. Qualitative Health Research. 2011; 21 (1):27–40. doi: 10.1177/1049732310377451. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lincoln Y. S. Emerging criteria for quality in qualitative and interpretive research. Qualitative Inquiry. 1995; 1 (3):275–289. doi: 10.1177/107780049500100301. [ CrossRef ] [ Google Scholar ]
- Luck L, Jackson D, Usher K. Case study: A bridge across the paradigms. Nursing Inquiry. 2006; 13 (2):103–109. doi: 10.1111/j.1440-1800.2006.00309.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mawn B, Siqueira E, Koren A, Slatin C, Devereaux Melillo K, Pearce C, et al. Health disparities among health care workers. Qualitative Health Research. 2010; 20 (1):68–80. doi: 10.1177/1049732309355590. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Merriam S. B. Qualitative research: A guide to design and implementation. 3rd ed. San Francisco, CA: Jossey-Bass; 2009. [ Google Scholar ]
- Meyer C. B. A case in case study methodology. Field Methods. 2001; 13 (4):329–352. doi: 10.1177/1525822x0101300402. [ CrossRef ] [ Google Scholar ]
- Morse J. M. Mixing qualitative methods. Qualitative Health Research. 2009; 19 (11):1523–1524. doi: 10.1177/1049732309349360. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morse J. M. Molding qualitative health research. Qualitative Health Research. 2011; 21 (8):1019–1021. doi: 10.1177/1049732311404706. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morse J. M, Dimitroff L. J, Harper R, Koontz A, Kumra S, Matthew-Maich N, et al. Considering the qualitative–quantitative language divide. Qualitative Health Research. 2011; 21 (9):1302–1303. doi: 10.1177/1049732310392386. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nagar-Ron S, Motzafi-Haller P. “My life? There is not much to tell”: On voice, silence and agency in interviews with first-generation Mizrahi Jewish women immigrants to Israel. Qualitative Inquiry. 2011; 17 (7):653–663. doi: 10.1177/1077800411414007. [ CrossRef ] [ Google Scholar ]
- Nairn K, Panelli R. Using fiction to make meaning in research with young people in rural New Zealand. Qualitative Inquiry. 2009; 15 (1):96–112. doi: 10.1177/1077800408318314. [ CrossRef ] [ Google Scholar ]
- Nespor J. The afterlife of “teachers’ beliefs”: Qualitative methodology and the textline. Qualitative Inquiry. 2012; 18 (5):449–460. doi: 10.1177/1077800412439530. [ CrossRef ] [ Google Scholar ]
- Piekkari R, Welch C, Paavilainen E. The case study as disciplinary convention: Evidence from international business journals. Organizational Research Methods. 2009; 12 (3):567–589. doi: 10.1177/1094428108319905. [ CrossRef ] [ Google Scholar ]
- Ragin C. C, Becker H. S. What is a case?: Exploring the foundations of social inquiry. Cambridge: Cambridge University Press; 1992. [ Google Scholar ]
- Roscigno C. I, Savage T. A, Kavanaugh K, Moro T. T, Kilpatrick S. J, Strassner H. T, et al. Divergent views of hope influencing communications between parents and hospital providers. Qualitative Health Research. 2012; 22 (9):1232–1246. doi: 10.1177/1049732312449210. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rosenberg J. P, Yates P. M. Schematic representation of case study research designs. Journal of Advanced Nursing. 2007; 60 (4):447–452. doi: 10.1111/j.1365-2648.2007.04385.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rytterström P, Unosson M, Arman M. Care culture as a meaning- making process: A study of a mistreatment investigation. Qualitative Health Research. 2013; 23 :1179–1187. doi: 10.1177/1049732312470760. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sandelowski M. Whatever happened to qualitative description? Research in Nursing & Health. 2000; 23 (4):334–340. doi: 10.1002/1098-240X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sandelowski M. What's in a name? Qualitative description revisited. Research in Nursing & Health. 2010; 33 (1):77–84. doi: 10.1002/nur.20362. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sandelowski M, Barroso J. Reading qualitative studies. International Journal of Qualitative Methods. 2002; 1 (1):74–108. [ Google Scholar ]
- Snyder-Young D. “Here to tell her story”: Analyzing the autoethnographic performances of others. Qualitative Inquiry. 2011; 17 (10):943–951. doi: 10.1177/1077800411425149. [ CrossRef ] [ Google Scholar ]
- Stake R. E. The case study method in social inquiry. Educational Researcher. 1978; 7 (2):5–8. [ Google Scholar ]
- Stake R. E. The art of case study research. Thousand Oaks, CA: Sage; 1995. [ Google Scholar ]
- Stake R. E. Case studies. In: Denzin N. K, Lincoln Y. S, editors. Strategies of qualitative inquiry. Thousand Oaks, CA: Sage; 1998. pp. 86–109. [ Google Scholar ]
- Sumsion J. Opening up possibilities through team research: Investigating infants’ experiences of early childhood education and care. Qualitative Research. 2013; 14 (2):149–165. doi: 10.1177/1468794112468471.. [ CrossRef ] [ Google Scholar ]
- Thomas G. Doing case study: Abduction not induction, phronesis not theory. Qualitative Inquiry. 2010; 16 (7):575–582. doi: 10.1177/1077800410372601. [ CrossRef ] [ Google Scholar ]
- Thomas G. A typology for the case study in social science following a review of definition, discourse, and structure. Qualitative Inquiry. 2011; 17 (6):511–521. doi: 10.1177/1077800411409884. [ CrossRef ] [ Google Scholar ]
- Tight M. The curious case of case study: A viewpoint. International Journal of Social Research Methodology. 2010; 13 (4):329–339. doi: 10.1080/13645570903187181. [ CrossRef ] [ Google Scholar ]
- Wager E, Kleinert S. Responsible research publication: International standards for authors. A position statement developed at the 2nd World Conference on Research Integrity, Singapore, July 22–24, 2010. In: Mayer T, Steneck N, editors. Promoting research integrity in a global environment. Singapore: Imperial College Press/World Scientific; 2010a. pp. 309–316. [ Google Scholar ]
- Wager E, Kleinert S. Responsible research publication: International standards for editors. A position statement developed at the 2nd World Conference on Research Integrity, Singapore, July 22–24, 2010. In: Mayer T, Steneck N, editors. Promoting research integrity in a global environment. Singapore: Imperial College Press/World Scientific; 2010b. pp. 317–328. [ Google Scholar ]
- Webb C, Kevern J. Focus groups as a research method: A critique of some aspects of their use in nursing research. Journal of Advanced Nursing. 2000; 33 (6):798–805. doi: 10.1046/j.1365-2648.2001.01720.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wimpenny K, Savin-Baden M. Exploring and implementing participatory action synthesis. Qualitative Inquiry. 2012; 18 (8):689–698. doi: 10.1177/1077800412452854. [ CrossRef ] [ Google Scholar ]
- Yeh H.-Y. Boundaries, entities, and modern vegetarianism: Examining the emergence of the first vegetarian organization. Qualitative Inquiry. 2013; 19 (4):298–309. doi: 10.1177/1077800412471516. [ CrossRef ] [ Google Scholar ]
- Yin R. K. Enhancing the quality of case studies in health services research. Health Services Research. 1999; 34 (5 Pt 2):1209–1224. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yin R. K. Case study research: Design and methods. 4th ed. Thousand Oaks, CA: Sage; 2009. [ Google Scholar ]
- Yin R. K. Applications of case study research. 3rd ed. Thousand Oaks, CA: Sage; 2012. [ Google Scholar ]
ORIGINAL RESEARCH article
Identification of factors associated with hospitalization in an outpatient population with mental health conditions: a case–control study.

- 1 Pôle Centre Rive Gauche, CH Le Vinatier, Bron, France
- 2 Université Claude Bernard Lyon 1, Villeurbanne, France
- 3 Pôle Santé Publique, Hospices Civils de Lyon, Lyon, France
- 4 UMR 5992 CNRS, U1028 INSERM, Centre de Recherche en Neurosciences de Lyon, Bron, France
- 5 Hospices Civils de Lyon, Lyon, France
- 6 UMR 5229 CNRS, Centre Ressource de Réhabilitation psychosociale, Le Vinatier, Bron, France
Introduction: Addressing relevant determinants for preserved person-centered rehabilitation in mental health is still a major challenge. Little research focuses on factors associated with psychiatric hospitalization in exclusive outpatient settings. Some variables have been identified, but evidence across studies is inconsistent. This study aimed to identify and confirm factors associated with hospitalization in a specific outpatient population.
Methods: A retrospective monocentric case-control study with 617 adult outpatients (216 cases and 401 controls) from a French community-based care facility was conducted. Participants had an index outpatient consultation between June 2021 and February 2023. All cases, who were patients with a psychiatric hospitalization from the day after the index outpatient consultation and up to 1 year later, have been included. Controls have been randomly selected from the same facility and did not experience a psychiatric hospitalization in the 12 months following the index outpatient consultation. Data collection was performed from electronic medical records. Sociodemographic, psychiatric diagnosis, historical issues, lifestyle, and follow-up-related variables were collected retrospectively. Uni- and bivariate analyses were performed, followed by a multivariable logistic regression.
Results: Visit to a psychiatric emergency within a year (adjusted odds ratio (aOR): 13.02, 95% confidence interval (CI): 7.32–23.97), drug treatment discontinuation within a year (aOR: 6.43, 95% CI: 3.52–12.03), history of mental healthcare without consent (aOR: 5.48, 95% CI: 3.10–10.06), medical follow-up discontinuation within a year (aOR: 3.17, 95% CI: 1.70–5.95), history of attempted suicide (aOR: 2.50, 95% CI: 1.48–4.30) and unskilled job (aOR: 0.26, 95% CI: 0.10–0.65) are the independent variables found associated with hospitalization for followed up outpatients.
Conclusions: Public health policies and tools at the local and national levels should be adapted to target the identified individual determinants in order to prevent outpatients from being hospitalized.
1 Introduction
The deinstitutionalization process in psychiatry began in the late twentieth century. This shift, especially seen in high-income countries, consists of a decrease in specialized psychiatric hospital beds for an increase of patients with a mental health condition, followed up in general medical hospitals, community-based care, and various outpatient settings ( 1 ). Between the mid-twentieth century and the 1990s, the number of psychiatric beds dropped to more than 80% in most western regions around the world ( 1 ).
However, the transition from an inpatient setting paradigm to an outpatient one needs to be carefully organized, with the necessary and appropriate structures and funding. Indeed, patients who suffer from a mental health disease need a deep consideration of the multifaceted world in which they live, to integrate and adapt their rehabilitation process for the outside world. The strengthening of community services has been heterogenous around the world ( 1 ). This deinstitutionalization failed, for example, in many places in the USA, leading to an increase in homelessness and crime among people with psychiatric diseases in the 1990s ( 2 ). More recently, there are still concerns about the good transitioning process that have been raised in central and eastern Europe, with a large body of evidence showing failures in deinstitutionalization and reinstitutionalization outcomes. Some of the causes found are lack of personal assistance, development and adaptation of social housing, and cuts to social support ( 3 ). The limited scaling up of community-based and primary care mental health services has also been identified as a failure factor of deinstitutionalization, along with fundamental concerns with the model. A deeper work on addressing social determinants is indeed also evoked, which are known to be fundamental structural drivers of mental illness ( 1 ). A relatively recent dramatic event that has to be remembered regarding the deinstitutionalization failure has been the “Life Esidimeni scandal” in 2016 in South Africa. Qualified as a humanitarian crisis, this event caused the deaths of a thousand psychiatric patients (94 according to an official report issued in 2017 ( 4 )) following their transfer from an inpatient setting to multiple outpatient settings without the appropriate care and follow-up required. Indeed, the cut in this 2,000-bed facility budget led to patients’ discharge regardless of individual autonomy and psychosocial disability into inadequately resourced nongovernmental facilities ( 5 ).
Deinstitutionalization requires strong, continuous efforts and should always stay person-centered. In this approach, the multidisciplinary team caring for the patient must bear in mind the individual factors that can predict the maintained recovery of the patient in the outpatient setting ( 6 ). Few settings succeed yet to address all structural determinants, even in high-income countries ( 1 ). Indeed, the Lancet Commission on Global Mental Health and Sustainable Development reminded us that regarding mental health, all countries are “developing” due to the relative underfunding of mental health services in relation to the burden of the condition ( 7 ). Ways to achieve success with deinstitutionalization may involve legislation with a mandate to establish community-based services (like in Italy ( 8 )) and to adapt them to a local context. Improvements will probably require a multitude of paradigm shifts within these structures, considering factors enabling their enhancement. If no adequate care is provided during deinstitutionalization or after it, patients may relapse after being discharged from the hospital and consequently readmitted. Many studies therefore considered readmission rate to be an indicator for intervention studies ( 1 ) and to identify protective and risk factors of relapses ( 9 ) ( 10 , 11 ).
A rich scientific literature is available on the study of risk factors of hospitalization in patients suffering from mental health pathologies. Nonexhaustively, for depression ( 12 ), the type of illness diagnosis, psychiatric comorbidity, treatment-related factors, and sociodemographic factors were associated with hospitalization. For bipolar disorders ( 13 ), characteristics of the index hospitalization (transfer, discharge disposition, length of stay), all-cause acute health service utilization in the year prior to it, and comorbidity were identified. For schizophrenia ( 14 , 15 ), recent medical follow-up discontinuation, medication nonadherence, life events, comorbidity, sex, age, and medication type were variables associated with hospitalization. Finally, for other psychiatric conditions ( 16 ) ( 9 , 10 ) ( 17 ) ( 11 ) ( 18 ), factors associated with hospitalization were shown to be recent medical follow-up discontinuation, multiple psychiatric hospitalization history, history of mental healthcare without consent, social isolation, socioeconomic status, violence history, psychiatric diagnosis, and patient’s satisfaction with treatment. A suicide attempt was found to be a risk factor for hospitalization in some studies and a protective factor at 1 year in others.
Nonetheless, the studies cited above only evaluate risk factors for readmission, i.e., for patients that are originally coming from an inpatient hospital setting. Literature focusing on an exclusive outpatient setting is scarce ( 19 , 20 ). It confirmed some previously identified risk factors in studies with an inpatient setting, such as alcohol/substance use, family history of mental health disease, and marital status, but have also diverging results for negative attitude/poor compliance with medication, identified by Antonio Ciudad et al. ( 20 ) as lowering the hazard of relapse during outpatient follow-up.
A systematic review of the literature carried out by Donisi et al. ( 11 ) additionally underlined some inhomogeneous results for identified risk factors associated with readmissions regarding sociodemographic variables, and a literature weakness for social support, considered only in a few papers. Furthermore, the authors emphasized that some factors were only identified in uni- or bivariate analyses and not in multiple regression.
More people are followed up in outpatient settings, and the minimal use of hospitalization remains a challenge in mental health. This study is of interest to mental health professionals and policymakers because more data on factors associated with hospitalization in followed up outpatients could help tailor appropriate follow-up care and adapt existing tools to reduce the need for hospitalization. Our study, therefore, aimed to identify and confirm risk factors of hospitalization in a specific outpatient population.
2.1 Study design
We conducted an observational, retrospective, monocentric case-control study based on hospitalization in one of the largest university-affiliated public psychiatric hospitals in France, with around 500 beds and 26,500 patients followed up on an outpatient basis, the Centre Hospitalier le Vinatier (CHV) in Bron. The CHV has several community-based care facilities called “Centre Médico-Psychologique” or “CMP”, providing medical–psychological and social consultations to anyone experiencing psychological difficulties. The present study was made in one of them. We reported this case-control study according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). For details, see Supplementary File 1 .
This retrospective study investigated the data from patients followed up in an outpatient setting from June 2021 to February 2023. This study period has been chosen in order not to have repercussions of the health restrictions due to the COVID-19 pandemic on our variables. The studied sample comes from the Centre Médico-Psychologique Centre Rive Gauche facility, administratively attached to the CHV but which has an independent operation for outpatients requiring mental healthcare in a defined geographic area (third, sixth, and eighth districts of Lyon).
In this facility, participants were eligible if they were aged 18 or older and had at least one outpatient psychiatric medical consultation between June 2021 and February 2023 (defined as the index consultation).
The sample size for this study was determined considering an odds ratio of 1.5 to 3 clinically meaningful based on previous literature. With a significance level of 0.05, a type I error of 0.025, and a power of 0.9, the required sample size was calculated using R and its Epicalc package 2.9.0.1. An estimate was then made with the lowest and highest expected frequencies for the studied variables. An ideal sample size was calculated and ranged between 807 and 423, with an approximate 1:2 case/control ratio.
2.3 Outcome
The studied outcome was full psychiatric hospitalization from the day after the index outpatient consultation and up to 1 year later. Full psychiatric hospitalization was defined in this study as more than 24 h of hospitalization in a psychiatric hospital. Thus, participants who had this outcome of interest were referred to as cases, whereas others who did not have the outcome of interest were referred to as controls.
2.4 Selection of cases and controls
Cases were patients who had a full psychiatric hospitalization from the day after the index outpatient consultation and up to 1 year later.
Controls were patients who did not experience full psychiatric hospitalization in the 12 months following the index outpatient consultation (therefore, controls have an index outpatient consultation before February 2022 to have at least a 1-year psychiatric hospitalization-free period).
All cases in the sample responding to the case definition were included ( n = 216).
Controls ( n = 401) were then randomly selected from the sample list of patients who met the definition of controls in order to approximately respect a 1:2 case/control ratio and the sample size determination. The random selection was performed with simple random sampling using computer-generated random numbers to ensure an unbiased selection process.
All the detailed characteristics of cases and controls can be found in Table 1 .
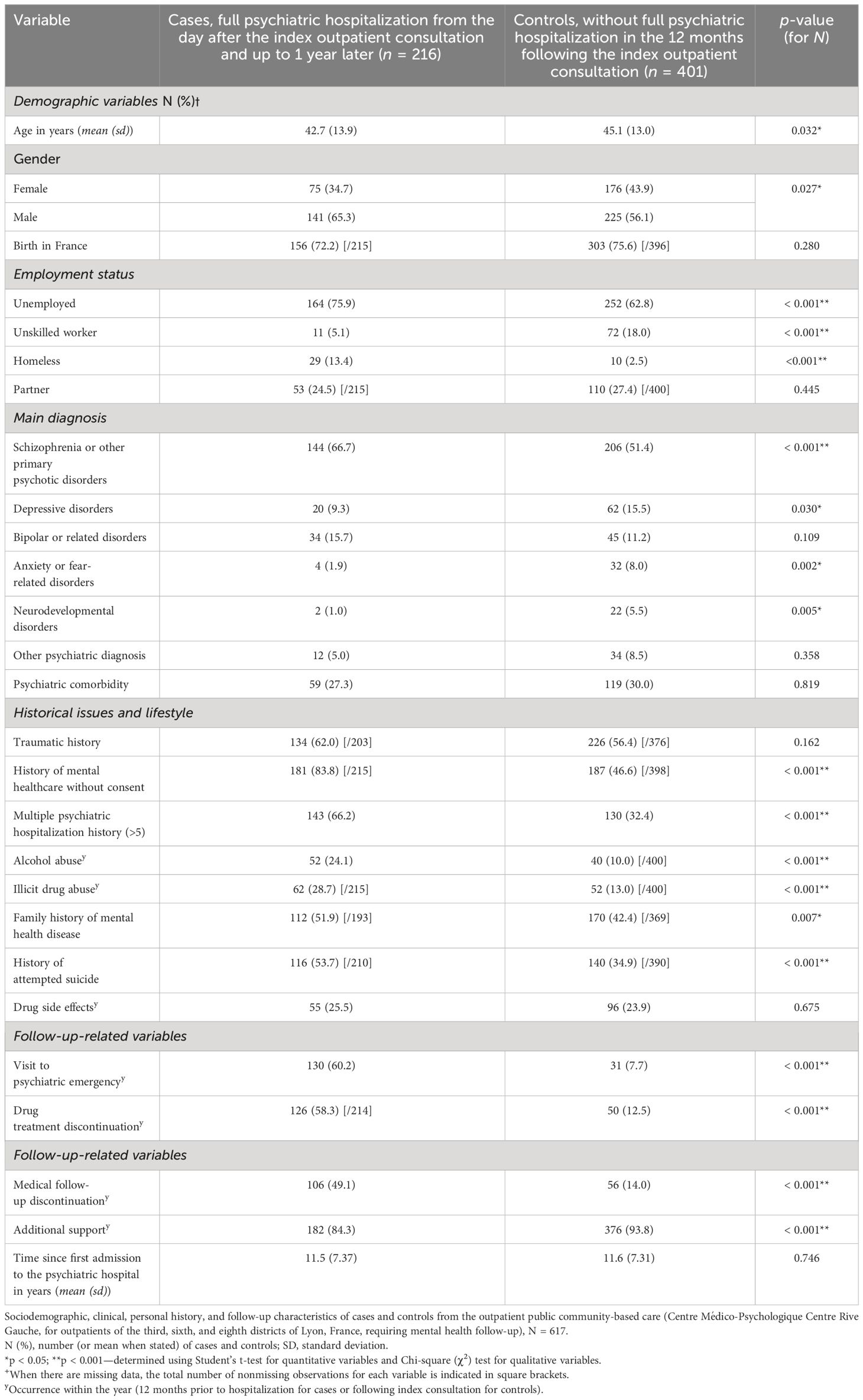
Table 1 Descriptive analysis.
2.5 Variables
The following exposure or potential confounder variables were collected retrospectively from patients’ medical records (collected in a binary yes/no format for qualitative variables):
I. Sociodemographic variables: age (in years, quantitative variable), gender, birth in France, unemployed (including patients on sick leave but not retired patients), unskilled worker (i.e., job accessible without special qualifications, only job category collected), homeless, partner of life (in a relationship).
II. Main psychiatric diagnosis (1 only), according to the ICD-11: depressive disorders, schizophrenia or other primary psychotic disorders, bipolar or related disorders, anxiety or fear-related disorders, neurodevelopmental disorders, another psychiatric diagnosis (other diagnosis belonging to the ICD-11 category 6: mental, behavioral, or neurodevelopmental disorders).
III. Psychiatric comorbidity: the presence of a psychiatric comorbidity (in addition to the main diagnosis, the presence of another psychiatric disorder falling under category 6 of the ICD-11).
IV. Historical issues and lifestyle: traumatic history (exhaustively: rape and/or sexual assault and/or loss of first-degree relative before the patient’s age of 18 and/or torture and/or major physical assault and/or loss of a child by suicide and/or violent death of a first-degree relative in front of the patient and/or patient placed in foster care during childhood, and/or direct witness to a homicide), history of mental healthcare without consent (medical treatment undertaken without the consent of the patient being treated, as permitted by law), multiple psychiatric hospitalization history (> 5 full psychiatric hospitalization), alcohol abuse within the year (diagnosed by the psychiatrist as pathologic, and corresponding to the ICD-11 codes 6C40.0, 6C40.1, 6C40.20, 6C40.21, and 6C40.3), illicit drug abuse within the year (regular consumption of an illicit substance greater than 1/week), family history of mental health disease (known psychiatric disorder within the patient’s biological family), history of attempted suicide, and drug side effect reported within the year (presence of a side effect documented on the patient’s medical record).
V. Follow-up-related variables: visit to psychiatric emergency within the year (excluding the one that led to full psychiatric hospitalization of the case definition), drug treatment discontinuation within the year (discontinuation by the patient, without medical agreement, of a psychiatric background treatment regimen over a period of more than 1 week), medical follow-up discontinuation within the year, additional support within the year (follow-up by a psychiatrist at least twice a year and/or regular follow-up by a medical mobile team (> 1/trimester) and/or included in a psychoeducation care program with a total hourly volume > 15 h/year), and time since first admission to the psychiatric hospital in outpatient or inpatient setting (in years, quantitative variable).
The term “within the year” refers to the variable being present 12 months prior to hospitalization for cases or 12 months following the index consultation for controls.
These variables were chosen because they have already been identified in the literature as factors associated with psychiatric hospitalization or suggested to be potential risk factors or confounders.
We hypothesized that all variables might be potential confounders and were indiscriminately tested to include them in the regression model (see Section 2.6) and to control for potential confounders.
2.6 Analysis
Statistical analysis was conducted using R software version 4.2.1 (23 June 2022) (R Core Team, 2022). Collected variables in case and control groups have been compared using a bivariate analysis ( Table 1 ). For quantitative variables, the Student’s t -test was used. For qualitative variables (dichotomous variables collected in a yes/no format), a Chi-square ( χ 2 ) test was performed.
Multivariable logistic regression was used to study the relationship between the outcome and the assessed covariables (listed in Section 2.2) with adjusted odds ratios (aORs) and 95% confidence intervals (CIs). In the analysis and to interpret its results, control group variables were considered baseline/reference category and case variables were compared to them. Based on the significant factors identified in the univariate analysis, variables were added to the model when p < 0.10. The model was built using a forward, stepwise selection procedure. It involves iteratively adding variables to the model one at a time, based on their individual contribution to improving the model’s fit. The fitness of the models was compared with a likelihood-ratio test. The choice was made to work on a subset of patients without missing data (complete case analysis). Interactions between variables included in the model were tested. They were considered when they appeared significant ( p -value < 0.01 to avoid multiple testing problems) and had an interpretable clinical meaning. The multiple logistic regression model was adjusted for all the risk factor variables included in the full model ( Table 2 ). The data normality of residuals for this multiple logistic regression was assessed by the Shapiro–Wilk normality test.
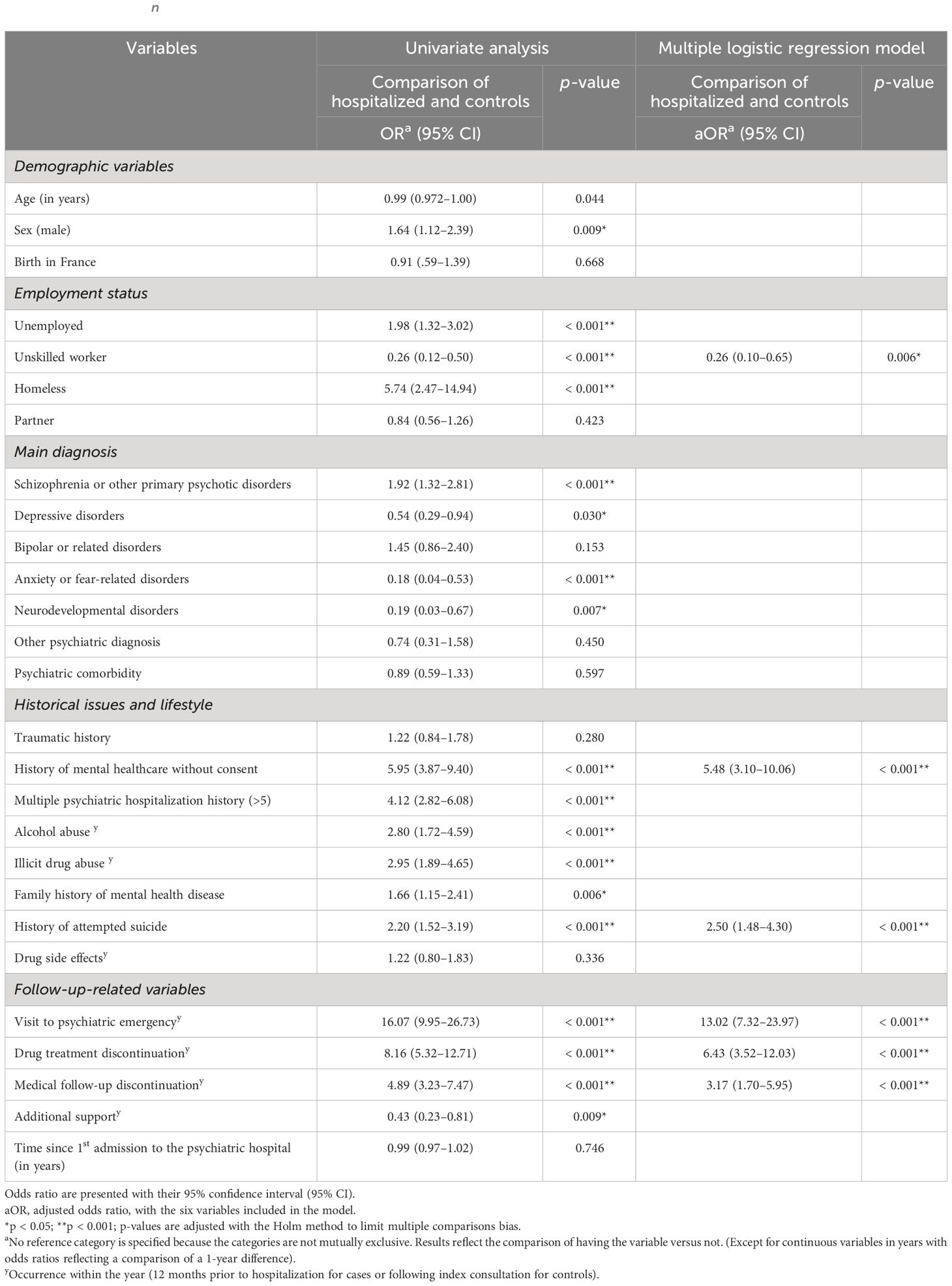
Table 2 Univariate analysis and results of a multiple logistic regression model predicting psychiatric hospital admission of outpatients (on a no missing values dataset, n = 521).
2.7 Data collection and ethical approval
Data were retrieved from the CHV’s electronic medical record system by reading through each medical record one by one. It was collected anonymously and entered directly into a secure document to ensure the confidentiality and privacy of participants. Personal identifying information such as names, addresses, and contact details were not recorded. Instead, each participant was assigned a unique identification code, which was used to perform the analyses with the studied variables. All data were stored securely and accessible only to authorized research personnel. Only the first author acquired data to guarantee reproducibility. Only the selected variables cited above were collected in the binary format “yes” or “no”, except for the two quantitative variables “age” and “time since first admission to the psychiatric hospital in outpatient or inpatient setting” collected in years (whole number).
To ensure data reliability, data were directly collected during the reading of each medical record.
Ethical approval was obtained by the Ethics Committee of the CHV with the registration number CEREVI/2023/003 on 27 February 2023. The study was conducted in accordance with the Declaration of Helsinki.
3.1 Participants and missing data investigation
All eligible cases have been included in the study (216 cases). Based on the number of cases and the predetermined targeted sample size, 401 controls were included out of a total eligible population of 1,044. The included controls were randomly selected from the sample list of eligible controls.
No missing data were observed for n = 521 patients out of the 617 included in the study.
When considering the mechanism underlying these missing data, it is important to note that they predominantly pertain to variables that necessitate investigating past events. Specifically, these pertain to the presence or absence of a family history of mental health diseases ( n = 55 missing data points out of 617, i.e., 8.9%), the presence or not of personal traumatic history ( n = 38 missing data points out of 617, i.e., 6.2%), and whether or not there was a history of suicide attempt ( n = 17 missing data out of 617, i.e., 2.8%). The other variables have less than 10 missing data points each. The details regarding missing data points for each of the variables within cases and controls are available in Table 1 .
3.2 Sociodemographic characteristics and descriptive analysis
Data from N = 617 patients followed up in an outpatient setting from June 2021 to February 2023 have been investigated for descriptive analysis (216 cases and 401 controls). Men were a higher proportion of cases (65.3%) than controls (56.1%). Cases were slightly younger than controls, with a mean age of 42.7 years old versus 45.1 years, respectively. Unemployment was higher among cases than controls (75.9% of unemployment for cases versus 62.8% for controls), and in parallel, more people had unskilled work in the control group (18.0% versus 5.1% in the case group ( p < 0.001)). Homelessness was much more prevalent among cases than controls, with 13.4% of homeless individuals among cases versus 2.5% for controls ( p < 0.001).
There was a difference in proportion for the main psychiatric diagnosis between groups for depression, schizophrenia or other primary psychotic disorders, anxiety or fear-related disorders, and neurodevelopmental disorders. Schizophrenia, or other primary psychotic disorders, was the main diagnosed psychiatric disease in our population (66.7% and 51.4% for cases and controls, respectively, p < 0.001).
For historical issues and lifestyle variables: case and control groups significantly differed in proportion for history of mental healthcare without consent, multiple psychiatric hospitalization history (> 5), alcohol or illicit drug abuse within the year, family history of mental health disease, and history of attempted suicide ( p < 0.001 except for family history of mental health disease with p = 0.007).
Finally, considering follow-up-related variables, strong significant proportion differences between groups for the following variables were observed ( p < 0.001): visit to a psychiatric emergency, drug treatment discontinuation, medical follow-up discontinuation, and additional support (all within the year). For the variables: visit to psychiatric emergency, drug treatment discontinuation, and medical follow-up discontinuation, the rates were all higher among cases than controls with respectively 60.2%, 58.3%, and 49.1% (cases) versus 7.7%, 12.5%, and 14.0% (controls). Conversely, additional support had a higher proportion in controls (93.8%) than in cases (84.3%) ( p < 0.001).
Table 1 describes the detailed sociodemographic, clinical, personal history, and follow-up characteristics of cases and controls ( N = 617).
3.3 Analytic statistics: multivariable modeling using multiple logistic regression
For the analytic statistics, modeling was conducted using a subset of patients without missing data (complete case analysis) with n = 521. According to our model, we found that six independent variables are significantly associated with full psychiatric hospitalization for patients being followed up in an outpatient setting. Indeed, in multivariable analysis, psychiatric hospitalization of outpatients remained strongly associated with a visit to a psychiatric emergency within a year (aOR: 13.02 [95% CI: 7.32–23.97]), a drug treatment or medical follow-up discontinuation within a year (aOR: 6.43 [95% CI: 3.52–12.03] and aOR: 3.17 [95% CI: 1.70–5.95], respectively), a history of mental healthcare without consent (aOR: 5.48 [95% CI: 3.10–10.06]), and a history of attempted suicide (aOR: 2.50 [95% CI: 1.48–4.30]). Finally, having a work (unskilled work) was conversely associated with a smaller risk of psychiatric hospitalization (aOR: 0.26 [95% CI: 0.10–0.65]). Estimates of adjusted odds ratio were calculated using logistic regression adjusted for the variables included in the model: “visit to a psychiatric emergency within a year”, “drug treatment discontinuation within a year”, “history of mental healthcare without consent”, “medical follow-up discontinuation within a year”, “history of attempted suicide”, and “unskilled job”.
Table 2 presents these identified variables with their respective odds ratios and confidence intervals.
4 Discussion
This study aimed to identify and confirm variables associated with hospitalization, including both protective and risk factors. This information aims to guide and establish appropriate vigilance and follow-up care for mental health in an outpatient setting.
According to our multivariable logistic regression model, six variables have been independently found to be significantly associated with full hospitalization in psychiatry for patients followed up in an outpatient setting: visit to a psychiatric emergency within a year, drug treatment discontinuation within a year, history of mental healthcare without consent, medical follow-up discontinuation within a year, history of attempted suicide, and unskilled job. These findings highlight the importance of considering follow-up-related, historical issues and sociodemographic determinants for successful outpatient rehabilitation and, by extension, deinstitutionalization.
Visit to a psychiatric emergency within the year was the most strongly associated variable with hospitalization and had an aOR of 13.02 (95% CI: 7.32–23.97) in our model. This result is in line with literature that identified emergency visits associated with hospitalization, but to a lesser extent and not in an exclusive outpatient setting like in our study ( 21 ) ( 10 ). Drug treatment discontinuation within the year was associated with an aOR of 6.43 (95% CI: 3.52–12.03). A systematic literature review by Donisi et al. ( 11 ) identified medication compliance as a factor associated with readmissions of psychiatric patients, but Antonio Ciudad et al. ( 20 ) found conflicting results for schizophrenic outpatients. A recent study on early psychiatric rehospitalization also found mental health prescription adherence as a predictor of rehospitalization with a random forest analysis ( 10 ). Medication compliance is known to be an important and challenging factor in the care of psychiatric patients ( 22 ). Our study identified and confirmed the importance of medication compliance in an outpatient setting. History of mental healthcare without consent was also associated with hospitalization (aOR: 5.48, 95% CI: 3.10–10.06). We can assume that patients with a history of care without consent are the ones with bad insight into their illness and are therefore more complex patients, requiring more frequent hospitalization. This risk factor has already been identified, particularly in schizophrenic patients ( 23 ). In another study, conducted without distinction of psychiatric pathology and still in an inpatient setting, no statistical association was found ( 18 ). Medical follow-up discontinuation in psychiatry has also already been studied in the literature. Anne Nelson et al. examined whether patients discharged from inpatient psychiatric care (and not originated from outpatient care like in our study) would have lower rehospitalization rates if they kept an outpatient follow-up appointment after discharge ( 17 ). The authors showed a greater rate of rehospitalization for patients who did not keep an appointment after discharge. The same conclusions have been drawn on a general psychiatric inpatient population ( 10 ) and on a study focused on schizophrenia ( 14 ). In our study, where patients come from an outpatient setting, we also found that medical follow-up discontinuation is a risk factor for hospitalization (aOR: 3.17, 95% CI: 1.70–5.95). A history of attempted suicide also appeared to be a risk factor for psychiatric hospitalization for patients followed up in an outpatient mental health setting, with a 2.50 aOR (95% CI: 1.48–4.30). However, the literature shows conflicting results. Some studies also confirm this risk factor, which has previously been identified in studies conducted in inpatient settings ( 18 , 24 ); in other studies, this risk factor was unclear, with nonsignificant results ( 11 , 21 , 25 ). The ability to have a job, which has been collected in our study with the variable “unskilled worker”, has been identified as a protective factor in the multivariable logistic regression model ( p -value: 0.006) adjusted for potential confounders, as illustrated in Table 2 : aOR of 0.26 (95% CI: 0.10–0.65). We explain this protective effect by assuming that controls, supposed to be clinically less severe than cases, with fewer symptoms, are more likely to get and keep a work. Having a job is indeed linked with cognitive remediation and the recovery process ( 26 ). “Unskilled worker” has been the only job category collected because other job categories were almost nonexistent in our population.
The community-based outpatient setting of the present study is particularly interesting regarding its population characteristics. Indeed, it offers multi-professional monitoring, which is valuable for patients with severe illnesses. With 75.9% of cases and 62.8% of controls unemployed in our study, this strongly suggests that mental disability significantly impacts psychosocial determinants, highlighting its importance. As with other chronic illnesses, psychological disability is a barrier to employment, and the severity of the condition is related to the ability to work ( 26 ). This might also explain the protective effect found in the association of the variable “unskilled worker”. Patients followed up regularly in this setting are also considered “severe” for other reasons. They often cannot follow a liberal mental health specialist due to poor socioeconomic conditions and may have a too severe psychiatric disorder requiring hospital practitioners (due to complex pharmacotherapeutics or illness) to reach a stable medical state. From a clinical point of view, most patients having a main diagnosis of schizophrenia or other primary psychotic disorders (66.7% among cases and 51.4% among controls) is another argument for the population severity, with patients who cannot be adequately followed up by general practitioners and/or private psychiatrists. Interestingly, this does not represent the psychiatric diseases distribution of general population and is even the opposite. Indeed, in France, anxiety disorders have the highest prevalence, followed by depression, bipolar disorders, and finally, psychotic disorders ( 27 ). Regarding historical issues and lifestyle, the prevalence of traumatic history was notably high in both groups, with around 60% prevalence. Mental health conditions are well-known to have multifactorial origins ( 28 ). Nevertheless, it is noteworthy to observe the prevalence of traumatic exposure within our study population. The high proportions of patients with mental healthcare without consent history and multiple psychiatric hospitalization histories (> 5) also underline the specificities of our outpatient population, which have a certain severity. Multidisciplinary community-based care has the potential to address the specific needs of the population within the framework of deinstitutionalization when considering the identified determinants.
The case–control design and the multivariable logistic regression utilized have, however, their limitations. Firstly, the population selection has been made through “hospital recruitment” (outpatient service attached to the CHV public psychiatric hospital). It can therefore introduce a selection bias regarding the admission probability of participants to that public outpatient service (e.g., patients with poorest socioeconomic conditions). Nonetheless, as the probability of admission to that service relies on the geographical sectorization (population originating from a defined geographic urban area: third, sixth, and eighth districts of Lyon) and has few equivalents in the private sector, we consider this bias to be existent but limited. To limit classification bias, classification was made on electronical medical records identically for cases and controls. Sectorization also prevents the risk of missing a hospitalization in another facility by ensuring the patient is ultimately hospitalized in his or her local hospital. Confusion bias has been considered via modeling with multivariable logistic regression. We assessed interactions in our model with one being significant (variable history of mental healthcare without consent with variable history of attempted suicide, adjusted p -value of 0.004). We, however, decided not to include this interaction in the model because (i) the clinical relevance of this interaction was not key in our exploratory investigation, and we do not seek a predictive model; (ii) considering that this interaction barely improves our overall model significance (residual deviance of 361 when considered versus 370, p -value: 0.003). Lastly, a limitation of our model is the absence of residuals normality for this multiple logistic regression. Indeed, residuals do not seem independent of the predicted values. Some explanatory variables would thus be lacking and not exhaustively listed in this study, such as variables on education level or on patient’s attitude and perception.
The highlights of this study are, however, its overall consistency with literature data on previously identified risk factors associated with hospitalization and the confirmation of these factors in an exclusive outpatient setting. The recruitment method used in this study with the sectorization principle of the service is also a robust point because it allowed to limit selection bias and consider all the patients followed up in this special outpatient setting.
5 Conclusion
Our study identified several independent risk and protective factors for hospitalization among patients with a mental health condition who are being treated in an outpatient setting. These factors include variables related to follow-up, such as a recent visit to a psychiatric emergency and recent discontinuation of drug treatment or medical follow-up (within the year), as well as historical issues or lifestyle-related factors.
To our knowledge, this is the first time that these factors are assessed statistically together in a specific outpatient setting, with patients not originating exclusively from a hospital. That is of great interest in the deinstitutionalization era. Public health policies at local and to a bigger extent, at the national scale, should consider these new data to target and tailor appropriate follow-up of care in outpatient settings. Tools to distinguish patients with the identified risk factors and prevent them from being hospitalized should also be created and adapted.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Medical information that cannot be shared according to the ethical approval obtained by the Ethics Committee of the CHV with the registration number CEREVI/2023/003 on 02/27/2023. Requests to access these datasets should be directed to [email protected].
Ethics statement
The studies involving humans were approved by Ethics Committee of the CHV with the registration number CEREVI/2023/003 on 02/27/2023. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the data were obtained in routine care practice with patient information and possible retraction. The study was carried out in accordance with current legislations.
Author contributions
ML: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Resources, Project administration, Methodology, Investigation, Formal Analysis, Data curation, Conceptualization. RM: Writing – review & editing, Supervision, Resources, Project administration, Funding acquisition, Conceptualization. CD: Writing – review & editing, Visualization, Validation, Supervision, Methodology. LZ: Writing – review & editing, Validation, Supervision, Project administration. JP: Writing – review & editing, Software, Data curation. NF: Writing – review & editing, Validation, Supervision, Resources, Project administration, Funding acquisition.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1341160/full#supplementary-material
1. Stein DJ, Shoptaw SJ, Vigo DV, Lund C, Cuijpers P, Bantjes J, et al. Psychiatric diagnosis and treatment in the 21st century: paradigm shifts versus incremental integration. World Psychiatry . (2022) 21:393–414. doi: 10.1002/wps.20998
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Torrey Fuller E. Out of the Shadows: Confronting America’s Mental Illness Crisis. Revised edition . New York Weinheim: Wiley (1997). 257 p.
Google Scholar
3. Mladenov T, Petri G. Critique of deinstitutionalisation in postsocialist Central and Eastern Europe. Disability Soc . (2020) 35:1203–26. doi: 10.1080/09687599.2019.1680341
CrossRef Full Text | Google Scholar
4. Makgoba MW. The report into the circumstances surrounding the deaths of mentally ill patients: Gauteng Province (2017). South Africa: Office of the Health Ombud. Available online at: https://ohsc.org.za/wp-content/uploads/2017/09/FINALREPORT.pdf (Accessed March 30, 2023).
5. Lund C. Mental health and human rights in South Africa: the hidden humanitarian crisis. South Afr J Hum Rights . (2016) 32:403–5. doi: 10.1080/02587203.2016.1266799
6. Killaspy H, Harvey C, Brasier C, Brophy L, Ennals P, Fletcher J, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry . (2022) 21:96–123. doi: 10.1002/wps.20940
7. Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The Lancet Commission on global mental health and sustainable development. Lancet . (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
8. Lora A. An overview of the mental health system in Italy. Ann Ist Super Sanita . (2009) 45:5–16.
PubMed Abstract | Google Scholar
9. Boyer CA, McAlpine DD, Pottick KJ, Olfson M. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry . (2000) 157:1592–8. doi: 10.1176/appi.ajp.157.10.1592
10. Zhao Y, Hoenig JM, Protacio A, Lim S, Norman CC. Identification of risk factors for early psychiatric rehospitalization. Psychiatry Res . (2020) 285:112803. doi: 10.1016/j.psychres.2020.112803
11. Donisi V, Tedeschi F, Wahlbeck K, Haaramo P, Amaddeo F. Pre-discharge factors predicting readmissions of psychiatric patients: a systematic review of the literature. BMC Psychiatry . (2016) 16:449. doi: 10.1186/s12888-016-1114-0
12. Wiegand HF, Saam J, Marschall U, Chmitorz A, Kriston L, Berger M, et al. Challenges in the transition from in-patient to out-patient treatment in depression. Dtsch Arztebl Int . (2020) 117:472–9. doi: 10.3238/arztebl.2020.0472
13. Juliet E, Trevor S, Gerhard H, John B. High-risk phenotypes of early psychiatric readmission in bipolar disorder with comorbid medical illness. Psychosomatics . (2019) 60:563–73. doi: 10.1016/j.psym.2019.05.002
14. Lin H-C, Lee H-C. The association between timely outpatient visits and the likelihood of rehospitalization for schizophrenia patients. Am J Orthopsychiatry . (2008) 78:494–7. doi: 10.1037/a0014515
15. Lee SY, Kim KH, Kim T, Kim SM, Kim J-W, Han C, et al. Outpatient follow-up visit after hospital discharge lowers risk of rehospitalization in patients with schizophrenia: A nationwide population-based study. Psychiatry Investig . (2015) 12:425–33. doi: 10.4306/pi.2015.12.4.425
16. Grinshpoon A, Lerner Y, Hornik-Lurie T, Zilber N, Ponizovsky AM. Post-discharge contact with mental health clinics and psychiatric readmission: A 6-month follow-up study. Israel J Psych Relat Sci . (2011) 48(4):262–67.
17. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv . (2000) 51:885–9. doi: 10.1176/appi.ps.51.7.885
18. Berardelli I, Sarubbi S, Rogante E, Erbuto D, Cifrodelli M, Giuliani C, et al. Exploring risk factors for re-hospitalization in a psychiatric inpatient setting: a retrospective naturalistic study. BMC Psychiatry . (2022) 22:821. doi: 10.1186/s12888-022-04472-3
19. Costa M, Plant RW, Feyerharm R, Ringer L, Florence AC, Davidson L. Intensive outpatient treatment (IOP) of behavioral health (BH) problems: engagement factors predicting subsequent service utilization. Psychiatr Q . (2020) 91:533–45. doi: 10.1007/s11126-019-09681-w
20. Ciudad A, San L, Bernardo M, Olivares JM, Polavieja P, Valladares A, et al. Relapse and therapeutic interventions in a 1-year observational cohort study of nonadherent outpatients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry . (2012) 36:245–50. doi: 10.1016/j.pnpbp.2011.10.014
21. Gentil L, Grenier G, Fleury M-J. Factors Related to 30-day Readmission following Hospitalization for Any Medical Reason among Patients with Mental Disorders: Facteurs liés à la réhospitalisation à 30 jours suivant une hospitalisation pour une raison médicale chez des patients souffrant de troubles mentaux. Can J Psychiatry . (2021) 66:43–55. doi: 10.1177/0706743720963905
22. Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Syst Rev . (2020) 9:17. doi: 10.1186/s13643-020-1274-3
23. Lin C-E, Chung C-H, Chen L-F, Chen P-C, Cheng H-Y, Chien W-C. Compulsory admission is associated with an increased risk of readmission in patients with schizophrenia: a 7-year, population-based, retrospective cohort study. Soc Psychiatry Psychiatr Epidemiol . (2019) 54:243–53. doi: 10.1007/s00127-018-1606-y
24. Hull JW, Yeomans F, Clarkin J, Li C, Goodman G. Factors associated with multiple hospitalizations of patients with borderline personality disorder. Psychiatr Serv . (1996) 47:638–41. doi: 10.1176/ps.47.6.638
25. Li D-J, Lin C-H, Wu H-C. Factors predicting re-hospitalization for inpatients with bipolar mania–A naturalistic cohort. Psychiatry Res . (2018) 270:749–54. doi: 10.1016/j.psychres.2018.10.073
26. Franck N. [Cognitive remediation and work outcome in schizophrenia]. Encephale . (2014) 40 Suppl 2:S75–80. doi: 10.1016/j.encep.2014.04.004
27. Micoulaud-Franchi J-A, Quiles C. Psychiatrie-Addictologie . Paris: Ellipses (2021). 203 p.
28. Crocq M-A. Histoire des traitements antipsychotiques à action prolongée dans la schizophrénie. L’Encéphale . (2015) 41:84–92. doi: 10.1016/j.encep.2014.12.002
Keywords: mental health system, outpatient clinic, deinstitutionalization, epidemiology, public health
Citation: Lebrat M, Megard R, Dananché C, Zimmer L, Plasse J and Franck N (2024) Identification of factors associated with hospitalization in an outpatient population with mental health conditions: a case–control study. Front. Psychiatry 15:1341160. doi: 10.3389/fpsyt.2024.1341160
Received: 19 November 2023; Accepted: 28 March 2024; Published: 18 April 2024.
Reviewed by:
Copyright © 2024 Lebrat, Megard, Dananché, Zimmer, Plasse and Franck. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthieu Lebrat, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.

IMAGES
VIDEO
COMMENTS
This qualitative study explores the lived experience of mental distress within college. student identity. The purposes of this study is to: (1) address a gap in extant literature on mental. health as an aspect of college identity from students' own voice, (2) add to literature that.
As the evidence base for the study of mental health problems develops, there is a need for increasingly rigorous and systematic research methodologies. Complex questions require complex methodological approaches. Recognising this, the MRC guidelines for developing and testing complex interventions place qualitative methods as integral to each stage of intervention development and ...
Study design. This study used qualitative pre- and post-intervention data from an evaluation of the batyr@school intervention [] delivered to YP, teachers and parents in drought affected communities in Australia [].Semi-structured interviews (group and individual) were conducted to enable an in-depth exploration of participants' views, experiences and needs about this sensitive topic [29, 30].
Qualitative mental health services research are often iterative in nature in which there is a constant back and forth between data ... Norman I, Redfern S, Jones R. Exposing the key functions of a complex intervention for share care in mental health: Case study of a process evaluation. BMC Health Services Research. 2008; 8:274. doi: 10. ...
The well-being of university students is an international concern. 1, 2 Although university settings could provide important opportunities to prevent and treat mental health problems, 3 current evidence suggests that this is not the case. A UK study reported that overall psychological distress does not fall below pre-admission levels at any point during university, 4 and similar distress ...
Qualitative case study, semi-structured interviews. 10 paramedics. 9 out of 10: Rees et al 101 AND Rees et al 102: UK: ... Paramedics managing patients experiencing mental health issues. Qualitative. Observations and interviews. 21 paramedics and 20 patients with mental illness. 10 out of 10: Ross et al 57: Australia:
Introduction. Growing numbers of university students are seeking mental health support, in part due to increasing levels of mental health problems in the general population, widening participation policies, and greater levels of awareness (Bould et al. Citation 2019; Hubble and Bolton Citation 2020; Lipson et al. Citation 2022).Research suggests more than a third (35%) of students both ...
Qualitative case studies, interviews, and observational studies form the foundation of many theoretical and practice approaches in mental health and psychiatry. For example, Freud's approach to psychoanalysis was grounded in qualitative case studies with his patients (Rothgeb 1971 ; Streiner 2008 ).
Objectives The objective of this study was to examine factors that threatened and protected the wellbeing of older adults living in the UK during social distancing restrictions due to the COVID-19 pandemic. Methods Semi-structured telephone or video interviews with 20 adults aged over 70. Purposive sampling methods were used to increase diversity within the group. Transcripts were analysed ...
The embedded case study design and the pattern matching analysis allowed us to gain insights into clients' mental health journey and the identification of three pathways into mental health recovery that were facilitated by the use of iCASS. According to interviewed patients, iCCAS facilitated detection of previously unknown mental health ...
Design: An in-depth qualitative study was conducted using thematic analysis to investigate the experiences of stigma in people with mental health problems. Methods: Eligible participants were recruited through a local mental health charity in the North West of England. The topic of stigma was examined using two focus groups of thirteen people ...
Making sense of mental health: a qualitative study of student counsellors. ... More and more people in the UK have poor mental health. Consequently, there is a growing demand for mental health professionals such as counsellors and psychotherapists. ... Five misunderstandings about case-study research. Qualitative Inquiry, 12, 219-245. doi:10. ...
Mental healthcare is an important component in societies' response to mental health problems. Although the World Health Organization highlights availability, accessibility, acceptability and quality of healthcare as important cornerstones, many Europeans lack access to mental healthcare of high quality. Qualitative studies exploring mental healthcare from the perspective of people with lived ...
However, studies have not previously investigated the subjective experiences of mental health stigma by those affected in a non-statutory treatment-seeking population. Design. An in-depth qualitative study was conducted using thematic analysis to investigate the experiences of stigma in people with mental health problems. Methods
Research suggests that teachers remain willing to support students in navigating their mental health, but continue to express a need for further training and guidance about how to do so in a way ...
Despite progress made under California's Mental Health Services Act, limited access to care for cultural and linguistic minority groups remains a serious issue in community mental health. In this qualitative study we report findings from a large-scale community-level assessment that explored barriers to accessing care from the perspectives of multiple stakeholders including county advisors ...
Background Stigma towards people with mental health problems (PMHP) is known to have substantial negative impacts on their lives. More in-depth exploration of the stigma and discrimination experienced by PMHP in low- and middle-income countries is needed. Previous research suggests that negative attitudes towards PMHP are widespread among the Filipino general public. However, no study has ...
1. Introduction. Discourse and policies around COVID-19 disproportionately focus on the adverse effects of the public health crisis on adults. Research shows that depression, anxiety, and post-traumatic stress are the most common psychological reactions to the pandemic in adults []; however, the impact of COVID-19 on young people is not fully understood.
An instrumental case-study approach was used to gather information (Creswell, 2013; Stake, 2005; Yazan, 2015; Yin, 2014) in an attempt to shed light on the issue of mental health in teacher preparation and how student teachers live with a mental health condition. This type of study was supported in the literature to
Furthermore, the observational study has been categorized into five types, namely cross-sectional design, case-control studies, cohort studies, case report and case series studies ... It was found that the credibility of qualitative research in mental health is achieved through methodological and interpretive rigour [32, 37]. The methodological ...
Study design: The study employed a qualitative, comparative case study design. We developed a framework, based on existing evidence and the experiential insight of the team, which conceptualised the challenges and facilitators of introducing peer worker roles into mental health services.
Given the prevalence of children's mental health disorders, teachers' roles have expanded to include identifying students with mental health needs and delivering mental health interventions. ... Teachers' perspectives on educator mental health competencies: A qualitative case study. American Journal of Qualitative Research, 2(1), 22-40 ...
To identify and describe the ethical considerations in qualitative health research for physical therapy: Case study—46 interviews patients: The authors suggest reflexivity as a way to recognize ethical moments throughout qualitative research and to help build methodological and ethical rigor: Yardley SJ et al. United Kingdom. 2014: II, III
Public health nurseś perceptions on promotive and risk factors for childreńs mental health: A qualitative interview study: To describe health-promoting factors as well as risk factors for children's mental health on the individual, interpersonal, organizational, municipal and political levels of the socio-ecological environment.
This study is part of a larger phase II, randomized, controlled clinical trial "Communication, Coordination and Security for people with severe Multiple Sclerosis (COCOS-MS)" [].This explorative clinical trial, employing a mixed-method design, incorporates a qualitative study component with PwsMS, caregivers and HCSs to enrich the findings of the quantitative data.
Keywords: arts, health policy, mental health, health promotion, knowledge mobilization, translation. Citation: Davies C, Pescud M, Maury S and Sullivan D (2024) A new perspective to an old problem - Mobilizing research into policy and practice using an arts and health case study. Front. Public Health 12:1392146. doi: 10.3389/fpubh.2024.1392146
Study Design. The qualitative exploratory, descriptive, and phenomenological design was adopted. This study design uses a flexible approach that produces high-quality data that enable a deeper understanding of lived experiences [].About the support and mental health challenges experienced by pregnant and parenting teenagers, in selected rural communities of Limpopo province.
Elite athletes' help-seeking on mental health might be influenced by their mental health literacy (MHL) and mental health experiences. The current study aimed to explore the MHL, experiences and help-seeking behaviours among elite athletes using a qualitative approach.
Case studies are designed to suit the case and research question and published case studies demonstrate wide diversity in study design. There are two popular case study approaches in qualitative research. The first, proposed by Stake ( 1995) and Merriam ( 2009 ), is situated in a social constructivist paradigm, whereas the second, by Yin ( 2012 ...
Keywords: mental health system, outpatient clinic, deinstitutionalization, epidemiology, public health. Citation: Lebrat M, Megard R, Dananché C, Zimmer L, Plasse J and Franck N (2024) Identification of factors associated with hospitalization in an outpatient population with mental health conditions: a case-control study. Front.