What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.

What Is Critical Thinking In Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.

Brain, Decision Making and Mental Health pp 179–189 Cite as
Critical Thinking in Nursing
- Şefika Dilek Güven 3
- First Online: 02 January 2023
1066 Accesses
Part of the book series: Integrated Science ((IS,volume 12))
Critical thinking is an integral part of nursing, especially in terms of professionalization and independent clinical decision-making. It is necessary to think critically to provide adequate, creative, and effective nursing care when making the right decisions for practices and care in the clinical setting and solving various ethical issues encountered. Nurses should develop their critical thinking skills so that they can analyze the problems of the current century, keep up with new developments and changes, cope with nursing problems they encounter, identify more complex patient care needs, provide more systematic care, give the most appropriate patient care in line with the education they have received, and make clinical decisions. The present chapter briefly examines critical thinking, how it relates to nursing, and which skills nurses need to develop as critical thinkers.
Graphical Abstract/Art Performance

Critical thinking in nursing.
This painting shows a nurse and how she is thinking critically. On the right side are the stages of critical thinking and on the left side, there are challenges that a nurse might face. The entire background is also painted in several colors to represent a kind of intellectual puzzle. It is made using colored pencils and markers.
(Adapted with permission from the Association of Science and Art (ASA), Universal Scientific Education and Research Network (USERN); Painting by Mahshad Naserpour).
Unless the individuals of a nation thinkers, the masses can be drawn in any direction. Mustafa Kemal Atatürk
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Bilgiç Ş, Kurtuluş Tosun Z (2016) Birinci ve son sınıf hemşirelik öğrencilerinde eleştirel düşünme ve etkileyen faktörler. Sağlık Bilimleri ve Meslekleri Dergisi 3(1):39–47
Article Google Scholar
Kantek F, Yıldırım N (2019) The effects of nursing education on critical thinking of students: a meta-analysis. Florence Nightingale Hemşirelik Dergisi 27(1):17–25
Ennis R (1996) Critical thinking dispositions: their nature and assessability. Informal Logic 18(2):165–182
Riddell T (2007) Critical assumptions: thinking critically about critical thinking. J Nurs Educ 46(3):121–126
Cüceloğlu D (2001) İyi düşün doğru karar ver. Remzi Kitabevi, pp 242–284
Google Scholar
Kurnaz A (2019) Eleştirel düşünme öğretimi etkinlikleri Planlama-Uygulama ve Değerlendirme. Eğitim yayın evi, p 27
Doğanay A, Ünal F (2006) Eleştirel düşünmenin öğretimi. In: İçerik Türlerine Dayalı Öğretim. Ankara Nobel Yayınevi, pp 209–261
Scheffer B-K, Rubenfeld M-G (2000) A consensus statement on critical thinking in nursing. J Nurs Educ 39(8):352–359
Article CAS Google Scholar
Rubenfeld M-G, Scheffer B (2014) Critical thinking tactics for nurses. Jones & Bartlett Publishers, pp 5–6, 7, 19–20
Gobet F (2005) Chunking models of expertise: implications for education. Appl Cogn Psychol 19:183–204
Ay F-A (2008) Mesleki temel kavramlar. In: Temel hemşirelik: Kavramlar, ilkeler, uygulamalar. İstanbul Medikal Yayıncılık, pp 205–220
Birol L (2010) Hemşirelik bakımında sistematik yaklaşım. In: Hemşirelik süreci. Berke Ofset Matbaacılık, pp 35–45
Twibell R, Ryan M, Hermiz M (2005) Faculty perceptions of critical thinking in student clinical experiences. J Nurs Educ 44(2):71–79
The Importance of Critical Thinking in Nursing. 19 November 2018 by Carson-Newman University Online. https://onlinenursing.cn.edu/news/value-critical-thinking-nursing
Suzanne C, Smeltzer Brenda G, Bare Janice L, Cheever HK (2010) Definition of critical thinking, critical thinking process. Medical surgical nursing. Lippincott, Williams & Wilkins, pp 27–28
Profetto-McGrath J (2003) The relationship of critical thinking skills and critical thinking dispositions of baccalaureate nursing students. J Adv Nurs 43(6):569–577
Elaine S, Mary C (2002) Critical thinking in nursing education: literature review. Int J Nurs Pract 8(2):89–98
Brunt B-A (2005) Critical thinking in nursing: an integrated review. J Continuing Educ Nurs 36(2):60–67
Carter L-M, Rukholm E (2008) A study of critical thinking, teacher–student interaction, and discipline-specific writing in an online educational setting for registered nurses. J Continuing Educ Nurs 39(3):133–138
Daly W-M (2001) The development of an alternative method in the assessment of critical thinking as an outcome of nursing education. J Adv Nurs 36(1):120–130
Edwards S-L (2007) Critical thinking: a two-phase framework. Nurse Educ Pract 7(5):303–314
Rogal S-M, Young J (2008) Exploring critical thinking in critical care nursing education: a pilot study. J Continuing Educ Nurs 39(1):28–33
Worrell J-A, Profetto-McGrath J (2007) Critical thinking as an outcome of context-based learning among post RN students: a literature review. Nurse Educ Today 27(5):420–426
Morrall P, Goodman B (2013) Critical thinking, nurse education and universities: some thoughts on current issues and implications for nursing practice. Nurse Educ Today 33(9):935–937
Raymond-Seniuk C, Profetto-McGrath J (2011) Can one learn to think critically?—a philosophical exploration. Open Nurs J 5:45–51
Download references
Author information
Authors and affiliations.
Nevşehir Hacı Bektaş Veli University, Semra ve Vefa Küçük, Faculty of Health Sciences, Nursing Department, 2000 Evler Mah. Damat İbrahim Paşa Yerleşkesi, Nevşehir, Turkey
Şefika Dilek Güven
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Şefika Dilek Güven .
Editor information
Editors and affiliations.
Universal Scientific Education and Research Network (USERN), Stockholm, Sweden
Nima Rezaei
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter.
Güven, Ş.D. (2023). Critical Thinking in Nursing. In: Rezaei, N. (eds) Brain, Decision Making and Mental Health. Integrated Science, vol 12. Springer, Cham. https://doi.org/10.1007/978-3-031-15959-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-15959-6_10
Published : 02 January 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-15958-9
Online ISBN : 978-3-031-15959-6
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
Key aspects of critical thinking include:
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
What are the Levels of Critical Thinking in Nursing?
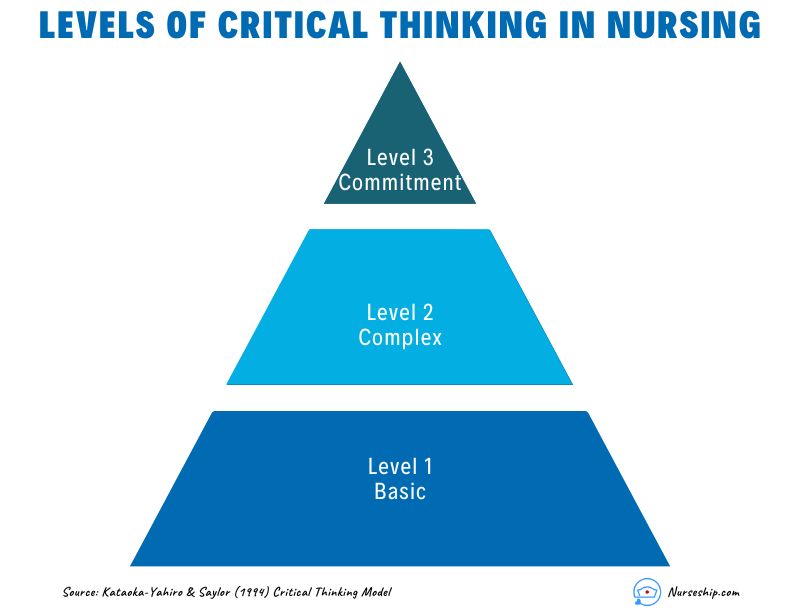
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.
Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.
Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.

What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Margaret McCartney:...
Nurses are critical thinkers
Rapid response to:
Margaret McCartney: Nurses must be allowed to exercise professional judgment
- Related content
- Article metrics
- Rapid responses
Rapid Response:
The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice. Nurses’ ability to recognize and respond to signs of patient deterioration in a timely manner plays a pivotal role in patient outcomes (Purling & King 2012). Errors in clinical judgement and decision making are said to account for more than half of adverse clinical events (Tomlinson, 2015). The focus of the nurse clinical judgement has to be on quality evidence based care delivery, therefore, observational and reasoning skills will result in sound, reliable, clinical judgements. Clinical judgement, a concept which is critical to the nursing can be complex, because the nurse is required to use observation skills, identify relevant information, to identify the relationships among given elements through reasoning and judgement. Clinical reasoning is the process by which nurses observe patients status, process the information, come to an understanding of the patient problem, plan and implement interventions, evaluate outcomes, with reflection and learning from the process (Levett-Jones et al, 2010). At all times, nurses are responsible for their actions and are accountable for nursing judgment and action or inaction.
The speed and ability by which the nurses make sound clinical judgement is affected by their experience. Novice nurses may find this process difficult, whereas the experienced nurse should rely on her intuition, followed by fast action. Therefore education must begin at the undergraduate level to develop students’ critical thinking and clinical reasoning skills. Clinical reasoning is a learnt skill requiring determination and active engagement in deliberate practice design to improve performance. In order to acquire such skills, students need to develop critical thinking ability, as well as an understanding of how judgements and decisions are reached in complex healthcare environments.
As lifelong learners, nurses are constantly accumulating more knowledge, expertise, and experience, and it’s a rare nurse indeed who chooses to not apply his or her mind towards the goal of constant learning and professional growth. Institute of Medicine (IOM) report on the Future of Nursing, stated, that nurses must continue their education and engage in lifelong learning to gain the needed competencies for practice. American Nurses Association (ANA), Scope and Standards of Practice requires a nurse to remain involved in continuous learning and strengthening individual practice (p.26)
Alfaro-LeFevre, R. (2009). Critical thinking and clinical judgement: A practical approach to outcome-focused thinking. (4th ed.). St Louis: Elsevier
The future of nursing: Leading change, advancing health, (2010). https://campaignforaction.org/resource/future-nursing-iom-report
Levett-Jones, T., Hoffman, K. Dempsey, Y. Jeong, S., Noble, D., Norton, C., Roche, J., & Hickey, N. (2010). The ‘five rights’ of clinical reasoning: an educational model to enhance nursing students’ ability to identify and manage clinically ‘at risk’ patients. Nurse Education Today. 30(6), 515-520.
NMC (2010) New Standards for Pre-Registration Nursing. London: Nursing and Midwifery Council.
Purling A. & King L. (2012). A literature review: graduate nurses’ preparedness for recognising and responding to the deteriorating patient. Journal of Clinical Nursing, 21(23–24), 3451–3465
Thompson, C., Aitken, l., Doran, D., Dowing, D. (2013). An agenda for clinical decision making and judgement in nursing research and education. International Journal of Nursing Studies, 50 (12), 1720 - 1726 Tomlinson, J. (2015). Using clinical supervision to improve the quality and safety of patient care: a response to Berwick and Francis. BMC Medical Education, 15(103)
Competing interests: No competing interests
Critical Thinking
High quality, safe patient care is dependent upon the healthcare provider’s ability to reason, think, and make judgments about care. Critical thinking, clinical reasoning and judgment are integral to quality clinical decisions and actions. Today’s healthcare landscape has transitioned towards an environment where patients are more medically complex, an aging population with chronic illness, and increased socioeconomic diversity. In order to provide quality patient-centered care, nurses need to develop CT skills in order to provide patients with expert care (Brunt, 2005).
Developing CT is an ethical responsibility of professional nursing practice, and a component for sound clinical judgments and safe decision-making. Thinking in a logical, systematic way, being open to questioning current practice, and reflecting on one’s practice regularly are some key features that strengthen nurses’ CT skills.
The quality of clinical decision-making is influenced by a number of factors, including experience, level of education, time pressures, and also the culture of the nursing unit (Johansson, Pilhammar, & Willman 2009). Developing critical thinking skills has the potential to improve personal practice and patient outcomes.
Critical thinking (CT) is a process used for problem-solving and decision-making. CT is a broad term that encompasses clinical reasoning and clinical judgment. Clinical reasoning (CR) is a process of analyzing information that is relevant to patient care. When data is analyzed, clinical judgments about care is made. The process of analyzing the data, making decisions is the result of CT—thinking critically throughout the entire patient situation, weighing all relevant options and using CT skills to make the best decision for the patient.
While many definitions have been cited for CT (see below), there is a general agreement that CT is a purposeful action that includes analysis, logical reasoning, intuition, and reflection. Making a concerted effort to critically think during patient care leads to safe, effective decisions. Developing CT skills is key for all nurses, they spend the most time with patients, and are able to recognize subtle changes in their patients and are positioned to make quick, precise decisions, often lifesaving. Using effective CT skills allows nurses to shape the outcome of a patient’s experience with the healthcare system.
The concept of critical thinking has been an integral part of professional frameworks for generations, yet scholars still debate a universal accepted definition. Dozens of CT definitions have been published, with each of them sharing some common features, such as reflection, contemplation, holism, and intuition. The list below shares a variety of CT definitions:
“The rational examination of ideas, inferences, assumptions, principles, arguments, conclusions, ideas, statement beliefs and action” (Bandman & Bandman, 1995, p. 7)
A reflective skepticism; “reflecting on the assumptions underlying our and others’ ideas and actions and contemplative alternative ways of thinking and living” (Brookfield, 1987, p. 18)
“The process of purposeful self-regulatory judgment . . . gives reasoned consideration to evidence, context, conceptualization, methods and criteria: (Facione, 2006, p. 21)
“Reasonable and reflective thinking that is focused upon deciding what to believe or do” (Kennedy, Fisher, & Ennis, 1991, p.46)
“An investigation whose purpose is to explore a situation, phenomenon, question, or problem to arrive at a hypothesis or conclusion about it that integrates all available information and that, therefore, can be convincingly justified” (Kurfiss, 1988, p. 37)
“The propensity and skill to engage in an activity with reflective skepticism” (McPeck, 1961, p. 8)
“The deliberative nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting and evaluating information that is both factual and belief based” (National League for Nursing Accrediting Commission, 2000, p. 8)
“A unique kind of purposeful thinking in which the thinker systematically and habitually imposes criteria and intellectual standards upon the thinking, taking charge of the construction of thinking, guiding the construction of the thinking according to the standard, and assessing the effectiveness of the thinking according to the purpose, the criteria and the standards” (Paul, 1993, p. 21)
“In nursing . . . an essential component of professional accountability and quality nursing care [that exhibits] confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, open-mindedness, perseverance and reflection.” (Scheffer & Ruberfeld, 2000, p. 357)
Concepts Related to Critical Thinking
Clinical Reasoning
- A process where nurses integrate and analyze patient data to make decisions about patient care (Simmons, Lanuza, Fonteyn, & Hicks, 2003)
Clinical Decision-Making
- A process of choosing between different options or alternatives (Thompson & Stapley, 2011)
Clinical Judgment
- A cognitive process used to make judgments based on patient data and cues. Nurses interpret a patient’s concerns, needs, and health problems for proper decision-making (Tanner, 2006, p. 204)
- Outcome of critical thinking in nursing practice; judgments begin with the end goal in mind; outcomes are met, involves evidence (Pesut, 2001)
Logical Reasoning
- Arriving at a conclusion based on relatively small amounts of knowledge and/or information (Westcott, 1968)
- “Drawing inferences or conclusions that are supported in or justified by evidence (Alfaro-LeFevre, 2015, p. 232)
- A purposeful analysis of one’s current and past actions (Schon, 1987)
Experience and Clinical Reasoning
According to Benner’s (1984) novice to expert model, expert nurses have an intuitive grasp of their patients’ problems, their approach is fluid, flexible, and proficient. Compared to novice nurses, they are more task oriented and require frequent verbal and physical cues to provide care.
Novice nurses are challenged with overcoming a knowledge gap, leading to less effective decisions and actions. Compared to experienced nurses, who are challenged with traditional thinking, leading to less effective clinical judgments and decisions (Cappelletti et al., 2014). Successful CR and decision-making require a balance of intuition and evidence-based thinking to make effective clinical decisions (Simmons et al., 2003).
Andersson et al. (2012) found nurses who were specialized in their setting (more experience) used a more holistic approach to making decisions (p. 876), compared to less experienced nurses who used a “task-and action-oriented approach” (p. 873). Gaining experience and knowledge is one way to improve thinking and decision-making, though improving CT skills can close the gap. Being open-minded, self-aware, and reflective offers nurses important information that can improve CR and decision-making. Clinical judgment (akin to CR) improves over time with nurses who uses reflection as a guide for decisions and actions (Cappelletti et al., 2014).

Critical Thinking and Clinical Decision-Making
Lee et al. (2017) conducted an integrated review on nine studies to determine whether effective CT impacted clinical decision-making. Four studies found CT impacted decision-making, though five studies did not find a correlation. Due to poor study designs, Lee et al. (2017) could not come to a clear decision on whether there was as significant correlation.
CT continues to be an important factor for problem-solving, regardless if studies can confirm a correlation to decision-making. Developing CT skills, such as reflection, intuition, and logical reasoning, are essential behaviors that lead to a patient-centered approach. Nurses who stop and think about what worked for a patient in the past, may consider the same option again, or may choose an alternative. Considering all possibilities with the patient’s best interest in mind is part of CT and making clinical decisions.
Researchers will continue to study the impact of CT on nursing care. Nurse educators will continue emphasize CT in the curriculum and assist students in developing CT skills throughout all levels of education as they offer students tools and methods for problem-solving.
Rubenfeld and Scheffer (2001) explain the essence of CT in nursing practice:
Critical thinking in nursing is an essential component of professional accountability and quality nursing care. Critical thinkers exhibit these habits of the mind: confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, intuition, open-mindedness, perseverance, and reflection. Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting and transforming knowledge (2001, p. 125).
Standards of Practice
Critical thinking and clinical reasoning are weaved throughout the Nursing Scope and Standards of Practice and Code of Ethics (American Nurses Association [ANA], 2021). The nursing process itself, Standards 1-6, are essentially a tool used for clinical reasoning. The standards require core cognitive competencies and guide nurses to use patient data to make effective clinical decisions.
The Essentials
Clinical Judgement is one of the eight featured concepts within The Essentials (American Association of Colleges of Nursing [AACN], 2021, p.12). The process of clinical judgement, as earlier in this section, is the outcome of critical thinking.
The Essentials explains how a liberal arts education is critical to exposing nurses to a broad worldview, giving them a holistic perspective that engages them in promoting health equity and social justice, , and “forms the basis for clinical reasoning and subsequent clinical judgments” (AACN, 2021, p. ).
Problem-Solving A pproaches
Reflective thinking.
Reflection is a powerful tool for recognizing errors in judgment, questioning one’s response, and ultimately improving outcomes. Below are two practice examples that illustrate the power of reflective thinking with interprofessional communication and patient care:
Novice and senior nurse communication
- Problem: A novice nurse is struggling with inserting IVs just about every shift. One day, the nurse asks the same more experienced nurse for help again. The nurse listens though does not turn around to face the nurse when questioned, and responds in a swift, aggressive way, “I’m swamped, we have no aides today and I’m falling behind with everything. I’ll help you when I get time, but it’s going to be a while.”
- Impact: The nurse’s patient is at risk for injury without an IV line. The patient may be upset and unsatisfied with care knowing the IV was out for an extended period of time. The nurse feels dejected, does not feel like she is a valued team member, and loses further confidence in her abilities. She considers quitting her job or transferring to another unit.
- Reflection: The experienced nurse realizes she was not empathetic to the nurse’s needs and impatient and aggressive in her response. She realizes the nurse is new and doesn’t have much confidence in her skills yet. She also knows the nurse is probably disappointed in the lack of teamwork and camaraderie. Most of all, she feels bad about disrespecting her coworker.
- Impact of reflection : After reflection of the situation, the nurse apologizes for her poor behavior. She states she will work with her each shift they work together, she will share personal tips and review educational materials. Additionally, she will offer to have her observe her IV insertions until she has mastered the skill. She will also make sure the new nurse feels like she is part of the team, not just the new nurse.
Shift report
- Problem: The oncoming nurse enters his patient room for the first time and finds the foley bag is full and the patient is complaining of abdominal discomfort.
- Impact: The patient is at risk for infection and may be disappointed with the quality of nursing care.
- Reflection: The oncoming nurse realizes there is always one or two problems or inconsistencies when he assesses his patients for the first time. He knows the outgoing nurses are skilled and provide quality care and considers another reason for the errors. After thinking about this for a while, he believes the process for shift report can help reduce change of shift errors. The nurse realizes there needs to be a better way for sharing patient information during change of shift.
- Impact of reflection: The nurse researches evidence-based practices to improve safety and quality during shift change. The nurse shares a copy of the review article on bedside report with his manager. The nurse offers to be a change champion on the unit to implement a new process for shift report.
L ong-term impact of reflection :
- Improved team cohesiveness, nurse retention and job satisfaction
- Improved patient satisfaction experience and quality of care, leading to higher insurance reimbursement

Glynn (2012) states reflective thinking enhances clinical judgment and gives nurses the opportunity to learn from actual or perceived errors. In regard to the communication scenario, it’s through reflection that nurses can think about their behaviors and responses. Reflect on the message for clarity, and whether it was shared in an empathetic and respective way.
As discussed in the communication chapter, poor communication is the number one reason for medication errors and sentinel events. Through reflection, miscommunication can be identified, solutions found, and implemented. In order for this process to come to fruition, nurses must take the initiative to reflect on their practice.
Creative Thinking
Creative thinking helps nurses generate alternative approaches to clinical decision-making. This type of thinking works especially well with medically complex patients, where care needs to be individualized to reach desired outcomes.
Akin to the concept of “thinking outside the box”, finding a novel approach to patient care prevents traditional, stagnant thinking. Choosing alternatives based solely on creative thinking can negatively impact outcomes unless it is paired with the skill of critical thinking. Critical thinking requires the nurse to view the patient holistically,
Nurses access knowledge unconsciously and trust this information as fact. Often referred to as a “gut feeling”, intuition comes naturally. Intuition is not a tool that is sought out at will, instead the knowledge emerges naturally during a care experience, resulting in firm actions and decisions. Intuition is a measure of professional expertise (Smith, Thurkettle, & Cruz, 2004), a type of clinical judgement that develops over time (Benner, 1984). Since this knowledge is considered intangible or irrelevant, some disregard it, though many studies have shown its positive influence in making accurate decisions and improving the quality of care (Robert, Tilley & Petersen, 2014).
- Nurses will recognize something about their patient that they can’t explain, and will make decisions on care without concrete evidence to back up their actions. Such actions can be lifesaving (Billay, Myrick, Luhanga & Yonge 2007). Each clinical experience acts as a learning experience for which lessons are learned and applied to the next experience (McCutcheon & Pincombe, 2001).
- Holtslander (2008) states Carper’s (1978) seminal work on the fundamental ways of knowing was published as a reaction to the overemphasis of empirical (scientific) knowledge in nursing practice. One of the four ways of knowing , called aesthetic knowing , explains the component of art within nursing practice, an, awareness of the patient, viewing the patient as unique. This viewpoint allows nurses to consider more than just empirical knowledge to guide practice.
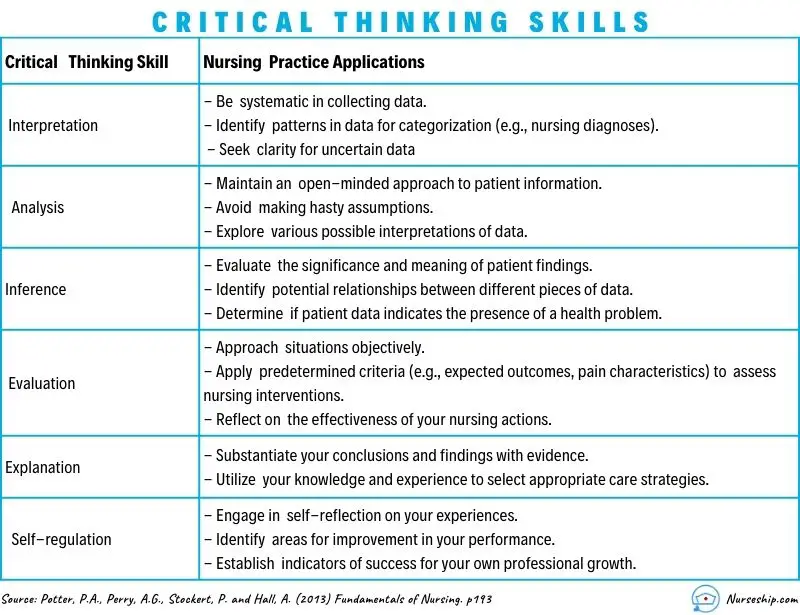
Critical Thinking Skills
As discussed earlier, CT encompasses a broad range of reasoning skills that lead to effective decision-making. Through the process of clinical reasoning and judgment, nurses make best choice after assembling and analyzing patient data.
White (2003) studied senior baccalaureate nurses and found the following five themes were essential to developing clinical decision-making skills:
- Gaining confidence in clinical skills
- Building relationships with staff
- Connecting with patients
- Gaining comfort in self as a nurse
- Understanding the clinical picture
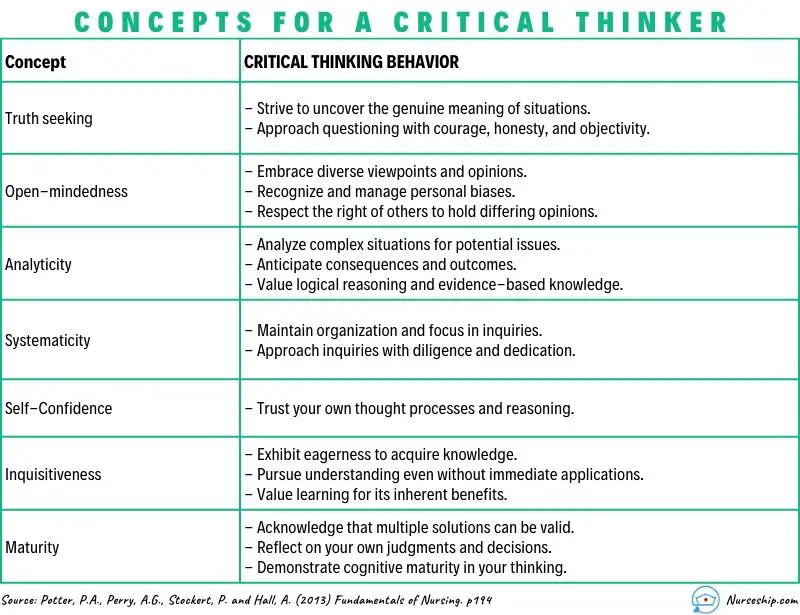
Scheffer and Rubenfeld (2000) found CT is comprised of affective and cognitive components. Affective components refer to an individual’s feelings and attitudes, and cognitive components refer to thought processes. The CT components include 10 habits of the mind (affective components) and seven skills (cognitive components), as follows:
Habits of the mind
- Confidence : assurance of one’s reasoning abilities
- C ontextual perspective : considerate of the whole situation, including relationships, background and environment relevant to some happening
- C re a tivity : intellectual inventiveness used to generate, discover, or restructure ideas; imagining alternatives
- F lexibility : capacity to adapt, accommodate, modify or change thoughts, ideas, and behaviors
- I nquisitiveness : an eagerness to know by seeking knowledge and understanding through observation and thoughtful questioning in order to explore possibilities and alternatives
- I ntellectual integrity : seeking the truth through sincere, honest processes, even if the results are contrary to one’s assumptions and beliefs
- I ntuition : insightful sense of knowing without conscious use of reason
- O pen-mindedness : a viewpoint characterized by being receptive to divergent views and sensitive to one’s biases
- P erseverance : pursuit of a course with determination to overcome obstacles
- R eflection : contemplation upon a subject, especially one’s assumptions and thinking for the purposes of deeper understanding and self-evaluation (Scheffer & Rubenfeld, 2000, p. 358)
- Analyzing : separating or breaking a whole into parts to discover their nature, function and relationships
- A pplying standards : judging according to established personal, professional or social rules or criteria
- D iscriminating : recognizing differences and similarities among things or situations and distinguishing carefully as to category or rank
- I nformation seeking : searching for evidence, facts or knowledge by identifying relevant sources and gathering objective, subjective, historical, and current data from those sources
- L ogical reasoning : drawing inferences or conclusions that are supported in or justified by evidence
- P redicting : envisioning a plan and its consequences
- T ransforming knowledge : changing or converting the condition, nature, form, or function of concepts among contexts (Scheffer & Rubenfeld, 2000, p. 358)
Development of CT is a lifelong process that requires nurses to be self-aware, and to use knowledge and experience as a tool to become a critical thinker. As nurses move along the continuum from novice to expert, one’s competence and ability to critically think will expand (Brunt, 2005).
- Transitions to Professional Nursing Practice. Authored by : Jamie Murphy. Provided by : SUNY Delhi. Located at : https://courses.lumenlearning.com/suny-delhi-professionalnursing . License : CC BY: Attribution

Privacy Policy
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
CPD Previous Next
Applying critical thinking to nursing, bob price healthcare education and practice development consultant, surrey, england.
Critical thinking and writing are skills that are not easy to acquire. The term ‘critical’ is used differently in social and clinical contexts. Nursing students need time to master the inquisitive and ruminative aspects of critical thinking that are required in academic environments. This article outlines what is meant by critical thinking in academic settings, in relation to both theory and reflective practice. It explains how the focus of a question affects the sort of critical thinking required and offers two taxonomies of learning, to which students can refer when analysing essay requirements. The article concludes with examples of analytical writing in reference to theory and reflective practice.
Nursing Standard . 29, 51, 49-60. doi: 10.7748/ns.29.51.49.e10005
All articles are subject to external double-blind peer review and checked for plagiarism using automated software.
Received: 23 February 2015
Accepted: 10 April 2015
education - students - study skills - studying - academic assignments - continuing professional development - CPD - clinical reasoning - critical appraisal - learning outcomes - reflection - reflective practice
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

19 August 2015 / Vol 29 issue 51
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Applying critical thinking to nursing
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Applying critical thinking to nursing
Affiliation.
- 1 Surrey, England.
- PMID: 26285997
- DOI: 10.7748/ns.29.51.49.e10005
Critical thinking and writing are skills that are not easy to acquire. The term 'critical' is used differently in social and clinical contexts. Nursing students need time to master the inquisitive and ruminative aspects of critical thinking that are required in academic environments. This article outlines what is meant by critical thinking in academic settings, in relation to both theory and reflective practice. It explains how the focus of a question affects the sort of critical thinking required and offers two taxonomies of learning, to which students can refer when analysing essay requirements. The article concludes with examples of analytical writing in reference to theory and reflective practice.
Keywords: Course assignment work; critical reflection; critical thinking; learning; nurse assessment; nurse education; reflection; reflective practice.
Publication types
- Education, Nursing*
- Problem Solving*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Improving nurses’ readiness for evidence-based practice in critical care units: results of an information literacy training program
Jamileh farokhzadian.
1 Nursing Research Center, Kerman University of Medical Sciences, Kerman, Iran
2 Department of Community Health Nursing, Razi Faculty of Nursing and Midwifery, Kerman University of Medical Sciences, Kerman, Iran
Somayeh Jouparinejad
3 Health in Disasters and Emergencies Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran
Farhad Fatehi
4 School of Psychological Sciences, Monash University, Melbourne, Australia
5 Centre for Online Health, The University of Queensland, Brisbane, Australia
Fatemeh Falahati-Marvast
6 Health Information Sciences Department, Faculty of Management and Medical Information Sciences, Kerman University of Medical Sciences, Kerman, Iran
Associated Data
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
One of the most important prerequisites for nurses’ readiness to implement Evidence-Based Practice (EBP) is to improve their information literacy skills. This study aimed to evaluate the impact of a training program on nurses’ information literacy skills for EBP in critical care units.
In this interventional study, 60 nurses working in critical care units of hospitals affiliated to Kerman University of Medical Sciences were randomly assigned into the intervention or control groups. The intervention group was provided with information literacy training in three eight-hour sessions over 3 weeks. Data were collected using demographic and information literacy skills for EBP questionnaires before and 1 month after the intervention.
At baseline, the intervention and control groups were similar in terms of demographic characteristics and information literacy skills for EBP. The training program significantly improved all dimensions of information literacy skills of the nurses in the intervention group, including the use of different information resources (3.43 ± 0.48, p < 0.001), information searching skills and the use of different search features (3.85 ± 0.67, p < 0.001), knowledge about search operators (3.74 ± 0.14, p < 0.001), and selection of more appropriate search statement ( x 2 = 50.63, p = 0.001) compared with the control group.
Conclusions
Nurses can learn EBP skills and apply research findings in their nursing practice in order to provide high-quality, safe nursing care in clinical settings. Practical workshops and regular training courses are effective interventional strategies to equip nurses with information literacy skills so that they can apply these skills to their future nursing practice.
The Institute of Medicine (IOM) has recommended that Evidence-Based Practice (EBP) be used in 90% of clinical decisions by 2020 [ 1 ]. EBP has become a popular buzzword in the healthcare industry [ 1 , 2 ]. This concept is defined as a problem-solving process in clinical decision making, which combines best research evidence with clinical expertise, patient preference, and clinical guidelines. EBP is required to improve quality of care, patient outcomes, and cost effectiveness of care [ 2 , 3 ]. It is a gold standard that provides a framework for delivery of safe and compassionate care. EBP is not only the use of research results but also includes all aspects of nursing knowledge, attitudes, skills and self-efficacy. It is considered as an essential skill for nurses to use the best scientific evidence when designing and implementing healthcare programs as well as when applying the available research evidence in decision-making process [ 2 ].
Critical care nurses are responsible for the assessment of patients and provision of care in critical care units. Critical care nurses need expertise and evidence to recognize clinical changes and prevent complications in patients. EBP should be applied to provide better care for patients in critical care units [ 4 ]. Policymakers expect nurses to make decisions based on the most recent evidence [ 5 ]. Therefore, nurses must be equipped with information literacy skills to obtain research findings and up-to-date information [ 6 , 7 ]. Information literacy is fundamental for successful implementation of EBP, and nurses should learn and improve their search and retrieval skills in order to obtain best evidence and information for providing sympathetic, safe and ethical care [ 7 – 11 ].
Despite the emphasis on EBP being applied in nurses’ daily practice, a significant number of nurses and other clinicians have not get involved in EBP and are not fully aware of the concept of EBP. Nurses are unprepared to implement EBP due to a lack of information literacy skills in information searching and retrieval. Therefore, there is a gap between nurses’ ability and implementation of EBP [ 2 , 3 , 12 – 14 ]. According to the nursing and medical literatures, nurses are facing difficulties with EBP and their most difficult task is to find the best evidence, identify the right sources, use optimal search methods, and critically appraise the evidence in general [ 15 ]. In recent years, health care policymakers have focused on the EBP as a means of improving health services and quality of care [ 16 ].
Several studies have been conducted to determine the significance of information literacy in the implementation of EBP. The New York University Division of Nursing, for example, used components of information literacy in core courses of a master’s program to provide nursing professionals with the skills [ 17 ]. One study addressed the importance of searching for, evaluating, synthesizing and applying documented information and found that more than 80% of the nurses did not receive any training related to EBP [ 10 ]. A number of other studies investigated the importance of information literacy and the need for education programs to enhance nursing search and retrieval skills [ 18 – 20 ]. Moreover, nurses’ readiness for EBP was measured by predictors of EBP, including nurse’s informational needs and skills in using EBP, attitudes, knowledge and workplace culture in order to identify desired interventions to make EBP more practical [ 21 , 22 ]. Concerning the importance of decision-making in critical care units, this study investigated the impact of a training program on nurses’ information literacy skills for EBP in critical care units.
The following hypotheses were tested:
- Hypothesis 1: Intervention group’s mean scores on the use of different information resources would improve after a training program compared with the control group.
- Hypothesis 2: Intervention group’s mean scores of information searching skills and use of different search features would increase after a training program compared with the control group.
- Hypothesis 3: Intervention group’s mean scores of knowledge about search operators would increase after a training program compared with the control group.
- Hypothesis 4: Intervention group’s mean scores of frequency of selecting more appropriate search strategy would increase after a training program compared with the control group.
Study design and settings
This interventional study with pretest-posttest design and two intervention and control groups was conducted from March to April 2019. Nurses working in critical care units (ICUs, CCUs, and Dialysis) were selected from three educational hospitals affiliated with Kerman University of Medical Sciences in the southeast of Iran. All methods were performed in accordance with the relevant guidelines and regulations of this university.
Participants and sampling
All nurses ( N = 330) working in critical care units at the time of data collection were included in the study. A sample size of 27 participants was calculated for each group (54 participants for the two groups) using a previous study and the sample size formula. By taking into account α = 0.05, test power of 80%, and large effect size (Cohen d = 0.7) and 10% dropout probability, 60 nurses were recruited in the study using the stratified random sampling method (30 nurses in each group). Three separate lists were created from nurses working in critical care settings of the three hospitals. Owing to the fact that the number of nurses in the three hospitals was almost equal, the random number table was used to select 20 nurses equally from each hospital (10 nurses for the intervention group and 10 nurses for the control group). Finally, these nurses were divided into the intervention ( n = 30) and control groups ( n = 30).
The inclusion criteria were nurses with a bachelor’s degree or higher, as well as at least 6 months of work experience in critical care units. Participants who missed more than one session and did not complete questionnaires were excluded from the study.
Instruments
Two questionnaires were used in this study. The first one concerned the nurses’ demographic information, including gender, age, work experience, organizational position, type of shift, level of education, marital status, and history of participation in research and information literacy courses (Table 2 ). The second questionnaire assessed information literacy skills for EBP, indicating EBP readiness. This questionnaire was developed by a professional team of faculty members and nurses [ 10 , 23 ]. The information literacy skills for EBP questionnaire comprised two sections. The first section covered the use of different information resources — print, electronic and human with 19 items on a 5-point Likert scale ranging from “never” to “always”. The second section collected data on information searching skills and the use of different search features of online databases and web search engines such as subject headings and search operators, and included 10 items on a 5-point Likert scale ranging from “never” to “always”. Nurses’ knowledge about Boolean/Connectors (‘OR’, ‘AND’, ‘NOT’ or ‘AND NOT’) and Proximity (e.g. W/nn; PRE/nn) operators was assessed using 4 items with yes (one score), no (zero score), and not sure options (zero score). Finally, to assess the nurses’ database searching skills and actual skills in developing an effective search statement, they were given a hypothetical searching topic (Effect of cigarettes on lung Cancer) along with five possible search statements on MEDLINE. They were asked to choose the most appropriate search statement.
Comparison of demographic and professional information of nurses in the intervention and control groups
The cross-cultural adaptation, validity and reliability (α = 0.87) of this questionnaire has been established by Farokhzadian et al. [ 24 ].
Data collection
The self-reported questionnaires were distributed among nurses of the intervention and control groups in the pretest (before workshop) and posttest stages (one month after the workshop). Except for the intervention group that received additional material derived from workshop and the control group that received no educational program during this period, all participants completed questionnaires simultaneously and attended the routine or traditional programs in hospitals. In other words, the two study groups were subjected to the same job descriptions. However, in order to improve internal validity of the study, researchers monitored the study conditions thoroughly to ensure that the intervention and control groups were similar in all aspects, except attendance at the training program. All participants completed the survey.
Intervention procedure
The training workshops were conducted in three eight-hour sessions over 3 weeks. The intervention group was divided into two groups to increase the members’ chances of participating in the workshop. Using lectures, questions and answers, slide presentations, hands-on and online exercises, homework, and educational CDs, one Ph.D. nurse and three experts in the field of medical informatics conducted the educational course. They have entered interactive computer-based search engines with the participants during the training.
Table 1 shows the content presented in this workshop.
Topics presented in the workshop
Statistical analysis
The data were analyzed in SPSS 21 by using descriptive statistics (frequency, percentage, mean and standard deviation) and inferential statistics (independent samples t -test, paired t -test, McNemar-test, chi square, and Fisher’s exact test). The Kolmogorov-Smirnov test showed that the data were normally distributed. The significance level was considered ≤0.05.
Demographic and professional information
All nurses (intervention and control groups) participated in the study and completed questionnaire (response rate = 100%). The nurses were asked to provide their demographic and professional characteristics. No significant difference was found between the intervention and control groups in terms of demographic and professional information (Table (Table2 2 ).
Use of different information resources
No significant difference was found between the intervention (2.66 ± 0.70) and control (2.67 ± 0.66) groups in the pretest mean scores of use of different information resources ( t = 0.10, P = 0.92). However, a significant difference was observed between the intervention (3.43 ± 0.48) and control (2.76 ± 0.60) groups in terms of use of different information resources in the posttest ( t = 4.90, p < 0.001), showing that the training program significantly improved the use of different information resources in the intervention group. In addition, results showed that the training program had the highest impact on the use of different electronic resources (1.11) and the lowest impact on the use of human resources (0.26) (Table 3 ).
Comparison of mean scores of the use of different information resources in intervention and control groups
*Paired t-test
**Independent t-test
As shown in Table Table3, 3 , the use of different information resources in the control group had no significant difference in the pretest and posttest.
Information searching skills and use of different search features
No significant difference was found between the intervention (2.06 ± 0.76) and control (2.19 ± 0.83) groups in the pretest mean scores of the information searching skills and the use of different search features ( t = − 0.59, P = 0.55). However, a significant difference was observed between the intervention (3.85 ± 0.67) and control (1.93 ± 0.70) groups in terms of information searching skills and the use of different search features in posttest ( t = 10.92, p < 0.001), showing that the training program significantly improved information searching skills and the use of different search features in the intervention group. In addition, result showed that the searching skills and use of different search features in the control group had no significant difference at pretest and posttest (Table 4 ).
Comparison of mean scores of the information searching skills and use of different search features
Knowledge about search operators
No significant difference was found between the intervention (0.61 ± 0.23) and control (0.56 ± 0.21) groups in the pretest mean scores of knowledge about search operators ( t = − 0.14, p = 0.88). However, a significant difference was observed between the intervention (3.74 ± 0.14) and control (0.33 ± 0.12) groups in terms of knowledge about search operators in the posttest ( t = 17.37, p < 0.001), showing that the training program improved significantly knowledge about search operators in the intervention group. In addition, result showed that the control group’s knowledge about search operators had no significant difference in the pretest and posttest (Table 5 ).
Comparison of mean scores of knowledge about search operators in intervention and control groups
Assessment of developing search strategy
In the pretest phase, no significant difference was found between the intervention (25.80%, n = 8) and control (3.2%, n = 1) groups in frequency of selecting more appropriate search statement ( x 2 = 6.36, P = 0.01). In addition, frequency of selecting more appropriate search statement increased significantly in the intervention group (93.50%, n = 29) compared with the control (3.2%, n = 1) group in the posttest ( x 2 = 50.63, p = 0.001). In addition, frequency of selecting more appropriate search statement in the control group had no significant difference in the pretest and posttest (Table (Table6 6 ).
Comparison of frequency of selecting more appropriate search statement in intervention and control groups
*McNemar-test
**chi square-test
The present study investigated the impact of a training program on nurse’s information literacy skills for EBP in the critical care units of three hospitals affiliated to an Iranian university. The findings showed that the training program significantly improved the use of different information resources in the intervention group. Furthermore, the nurses in intervention group sought information more from electronic resources than from human and printed resources at posttest. In agreement with our findings, Tannery et al. [ 25 ] designed a pre/post-intervention study and provided access to a collection of online knowledge-based resources. After the intervention, nurses began to use various information resources as well as electronic resources instead of colleagues and print textbooks or journals. In a 4-year longitudinal study, Weng et al. [ 26 ] examined information seeking behaviors for EBP in the physicians and nurses through implementing an EBM multifaceted program that included access to websites, databases, libraries, and workshops. They found that the use of print resources remained unchanged while the use of electronic resources increased. Fiander et al. [ 27 ] in a review study reported that the use of electronic information increased in the intervention groups participating in training programs. The present study finding disagrees with the cross-sectional study conducted by Thiel et al. [ 21 ], which found that the majority of nurses obtained informational needs from peers or colleagues rather than journals, books and electronic databases. According to Patelarou et al. [ 22 ], nurses use electronic databases infrequently, with young nurses and university graduates being more likely to use them. A descriptive study was done by Farokhzadian et al. [ 24 ] who showed that nurses used different information resources, including more human and printed resources than electronic ones to search information. One of the main reasons for nurses’ poor use of electronic resources is their unfamiliarity with online databases and insufficient search skills.
The results showed that our training program improved significantly information searching skills and the use of different search features in intervention group at posttest. Kratochvíl [ 28 ] also showed positive impact of an information literacy course on students in the post-test stage, which improved their knowledge about search skills such as subject heading, defining keywords and wildcards. Carlock and Anderson [ 29 ] assessed information literacy skills of student nurses in two groups after teaching them the instructions and holding sessions. Then, for further investigation, one group was followed up while the other was not. Students in the follow-up group improved their search skills, while students in the non-follow-up group made more mistakes in their searches. Using valid and reliable nurse’s readiness tool for EBP with four specific domains including “EBP-attitude”, “EBP-knowledge”, “informational needs” and “workplace culture” [ 30 ], Patelarou et al. [ 22 ]reported an average level of nurse’s skill to conduct a search in CINAHL or MEDLINE databases based on informational needs domain. They also found “EBP knowledge” domain was positively correlated with both “informational needs” and “workplace culture” domains, implying that a nurse can learn EBP knowledge by developing necessary skills in an EBP-friendly workplace.
The findings indicated that the educational program improved significantly knowledge about search operators and frequency of selecting more appropriate search statement in the intervention group at the posttest. Therefore, the educational program improved significantly the database searching skills and actual skills in developing an effective search statement in nurses of the intervention group.
Thiel and Ghosh [ 21 ] discovered that the perceived nurse’s EBP knowledge was at a moderate level and significantly correlated with the nurse’s education level and years of nursing experiences. They described perceived EBP knowledge as different from actual knowledge and suggested that providing various resources for EBP teaching–learning plans was a helpful tool to evaluate actual knowledge of EBP over time. In addition, Kratochvíl [ 28 ] showed that students’ knowledge about search statement and Boolean operators increased after educational intervention. In a randomized controlled trial, Brettle et al. [ 31 ] evaluated the effectiveness of an online information literacy tutorial and a face-to-face session for teaching information literacy skills to nurses. The searching skills, including developing search strategy and using search operators, improved after intervention and remained unchanged in both methods 1 month later, but no improvement in any of the methods was observed after one month. El-sayed et al. [ 32 ] showed improvement in the search of information resources and search strategy among master nursing students through a training program. Ruzafa-Martínez et al. [ 33 ] conducted a 15-week educational course on EBP for the undergraduate nursing students, covering topics such as search strategies, Boolean operators, and limit function, and showed that knowledge and skill for EBP improved in the interventional group. In their pretest-posttest research, Hsieh et al. [ 34 ] employed an EBP program for search strategy and electronic literature search and evaluated learning outcomes before, immediately after, and 3 months after the intervention. They found that knowledge and skill increased immediately after the intervention, but then decreased in the final follow-up. Therefore, continuous training is essential for the stability and durability of the learned skills through follow-up courses in the previous studies. In contrast, Farokhzadian et al. [ 24 ] reported in a descriptive study that most of the nurses knew nothing or very little about information literacy skills like advanced searching techniques, Boolean and proximity operators, search features such as truncations, wildcards, MeSH terms, and search limits. Majid et al. [ 23 ]investigated nurses’ literature searching skills and discovered that they used basic search features and that less than one-quarter were familiar with Boolean and proximity operators. They also reported that nurses who had previously attended EBP training programs had more knowledge than those who had not. Hirt et al. [ 35 ] conducted a review study of educational interventions on health-related literature searching skills. They indicated that participants in the included studies were students and physicians from various health professions. The study findings were divided into two categories: search strategy development and database searching skills. Some interventional studies included in this review reported significant improvements in the development of search strategies and database searching skills, while others showed no changes in these two categories. Therefore, nurses must have sufficient knowledge to improve their information literacy skills in order to retrieve information related to clinical practice, improve the quality of care and make better decisions.
Diverse and efficient methods are recommended to empower nurses in information literacy, including integrating computer and search skills training program into the nursing curriculum in different semesters, ongoing education through holding practical workshops and sessions, following seeking behaviors among nurses and presenting feedback to them, easy access to online databases in clinical wards, updating nurses’ information about changes in search features and user interfaces of online database such as launch of the “new PubMed”, continuous encouragement to turn EBP into a routine activity, development of an information center and educational spaces equipped with IT facilities, and provision of 24/7 online trainings. Further research on the efficacy of these interventions is also suggested by using controlled study designs and long-term follow-up. According to the findings of a review study [ 35 ], few educational interventional studies on search skills have been conducted in the last 10 years. Therefore, more emphasis must be placed on nurses' education.
Limitations
We did not evaluate the effectiveness of follow-up courses in this study because nurses working in the critical care units did not have enough time and motivation to participate in these courses due to heavy shift works. This study investigated the effect of training program on nurses in critical care units and similar interventions could be performed on nurses in other wards to ensure the results are generalizable.
The results of this study show that the training program can effectively improve nurses’ information literacy skills. Information literacy is one of the key components of EBP for identifying and evaluating available scientific evidence. Nurses need search skills in order to find and use evidence in their nursing practice and provide positive patient outcomes. Therefore, it is critical to develop educational programs to help nurses improve their information literacy skills. Our findings provide health planners and policymakers with the opportunity to design an educational model that is effective, practical, and continuous in order to strengthen the nurses’ skills and make EBP more practical in the clinical setting. Extensive developments in EBP will eventually lead to improvement in healthcare and health services quality.
Acknowledgements
The researchers appreciate all nurses who spent their time so generously to participate in this study.
Abbreviations
Authors’ contributions.
JF, SJ and FFM contributed to conceiving and designing the research. The data were collected, analyzed, and interpreted by JF, SJ, FF and FFM. JF, SJ, FF and FFM contributed equally to writing and revising the manuscript and approved the final manuscript.
This research received no financial support from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
Declarations.
This study was approved by the Ethics Committee of Kerman University of Medical Science with the code of ethics No. IR.KMU.REC.1397.373. At the request of the Ethical committee, the study was conducted in accordance with the Declaration of Helsinki and Ethics Publication on Committee (COPE). There was no ethical issue during the study and data collection. Furthermore, the participants were informed that they could withdraw from the study at any time. Moreover, they were ensured about confidentiality of information. Informed consent was obtained from all nurses. For the participations’ information confidentiality to be ensured special codes were allocated to each questionnaire and the data were analyzed using these codes. Following the completion of the intervention and collection of the second phase data, participants of the control group were provided with an educational package consisting of a CD and a handbook.
Not applicable.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

CPD modules
Applying critical thinking to nursing
Author: Bob Price
Share module
Course description.
The aim of this module is to enable one to have a better understanding of the different types and levels of critical thinking that relate to both theoretical and reflective forms of analytical writing. The module provides a classification of levels of critical thinking and gives examples of analytical writing in the contexts of theory and reflective practice.
Don't forget that you do not have to complete our two-hour learning modules all in one go. Tailor your learning to fit into your busy schedule by undertaking one or two sections at a time. You can stop and save your learning at any point and pick up where you left off when you return.
Learning aims and intended outcomes
- Define the term ?critical' as used in clinical practice
- Outline the differences between ?being critical' when analysing theories or concepts and reviewing your experience in nursing
- Use your enhanced understanding of critical thinking to clarify with your tutors what is required in your coursework assignments
- Describe different levels of critical thinking and the purpose of each
- Introduction
- Critical thinking
- Differentiating theory and experience-centred critical thinking
- Foci for critical thinking
- Levels in theory-related critical thinking
- Levels of critical thinking in reflective writing
- Critical thinking in assignments
- Conclusions
Please note that information provided by RCNi Learning is not sufficient to ensure competence in the skill. Assessment of competence should take place in line with local practice. Practice should always align with local protocols and procedures, latest guidelines and any regulatory code. All modules should currently be viewed together with available national and local Covid-19 guidelines. For advice, go to www.rcn.org.uk/covid-19
Why use RCNi Learning
Document your learning.
Save certificates to your RCNi Revalidation Portfolio to use for CPD and revalidation
Engaging learning
Interactive quizzes, imagery and videos make learning an enjoyable experience
RCNi quality assurance
Double-blind peer-reviewed and updated in-line with changing practice
Learn on demand
Bitesize learning or an in-depth course that can be paused and resumed at any time.
RCNi Learning is available to individuals with an RCNi Plus subscription
Save over 50% on your first 3 months and gain access to:
Learning Modules
Earn CPD with RCNi Learning, giving you access to over 170 CPD modules
RCNi Journals
Unlimited access to all 10 RCNi journals and their archives
Revalidation Portfolio
Quick, easy access to build, track and save evidance for revalidation
CPD Quizzes
Over 400 CPD Quizzes taken from evidence-based and peer-reviewed clinical articles
RCNi Plus Dashboard
Customise your dashboard with topics most relevant to you
For organisations
RCNi provides learning resources to organisations who want to support their staff in delivering high quality, person-centred care by offering CPD and a revalidation portfolio
All modules undergo a double-blind peer-review process and are updated in-line with changing practice and current guidelines
Download RCNi Learning from the app store today
Use RCNi Learning to earn CPD hours for revalidation and stay up-to-date with the latest clinical guidance
Share the module to your friend
Rcni learning feedback.
Please provide your feedback below. Fields marked as ( * ) are mandatory
On a scale of 1 to 5, please rate your overall experience
* What part/parts of the course did you find rewarding?
* Can you suggest any improvements/additions to the course?
Timeout activities

A Crash Course in Critical Thinking
What you need to know—and read—about one of the essential skills needed today..
Posted April 8, 2024 | Reviewed by Michelle Quirk
- In research for "A More Beautiful Question," I did a deep dive into the current crisis in critical thinking.
- Many people may think of themselves as critical thinkers, but they actually are not.
- Here is a series of questions you can ask yourself to try to ensure that you are thinking critically.
Conspiracy theories. Inability to distinguish facts from falsehoods. Widespread confusion about who and what to believe.
These are some of the hallmarks of the current crisis in critical thinking—which just might be the issue of our times. Because if people aren’t willing or able to think critically as they choose potential leaders, they’re apt to choose bad ones. And if they can’t judge whether the information they’re receiving is sound, they may follow faulty advice while ignoring recommendations that are science-based and solid (and perhaps life-saving).
Moreover, as a society, if we can’t think critically about the many serious challenges we face, it becomes more difficult to agree on what those challenges are—much less solve them.
On a personal level, critical thinking can enable you to make better everyday decisions. It can help you make sense of an increasingly complex and confusing world.
In the new expanded edition of my book A More Beautiful Question ( AMBQ ), I took a deep dive into critical thinking. Here are a few key things I learned.
First off, before you can get better at critical thinking, you should understand what it is. It’s not just about being a skeptic. When thinking critically, we are thoughtfully reasoning, evaluating, and making decisions based on evidence and logic. And—perhaps most important—while doing this, a critical thinker always strives to be open-minded and fair-minded . That’s not easy: It demands that you constantly question your assumptions and biases and that you always remain open to considering opposing views.
In today’s polarized environment, many people think of themselves as critical thinkers simply because they ask skeptical questions—often directed at, say, certain government policies or ideas espoused by those on the “other side” of the political divide. The problem is, they may not be asking these questions with an open mind or a willingness to fairly consider opposing views.
When people do this, they’re engaging in “weak-sense critical thinking”—a term popularized by the late Richard Paul, a co-founder of The Foundation for Critical Thinking . “Weak-sense critical thinking” means applying the tools and practices of critical thinking—questioning, investigating, evaluating—but with the sole purpose of confirming one’s own bias or serving an agenda.
In AMBQ , I lay out a series of questions you can ask yourself to try to ensure that you’re thinking critically. Here are some of the questions to consider:
- Why do I believe what I believe?
- Are my views based on evidence?
- Have I fairly and thoughtfully considered differing viewpoints?
- Am I truly open to changing my mind?
Of course, becoming a better critical thinker is not as simple as just asking yourself a few questions. Critical thinking is a habit of mind that must be developed and strengthened over time. In effect, you must train yourself to think in a manner that is more effortful, aware, grounded, and balanced.
For those interested in giving themselves a crash course in critical thinking—something I did myself, as I was working on my book—I thought it might be helpful to share a list of some of the books that have shaped my own thinking on this subject. As a self-interested author, I naturally would suggest that you start with the new 10th-anniversary edition of A More Beautiful Question , but beyond that, here are the top eight critical-thinking books I’d recommend.
The Demon-Haunted World: Science as a Candle in the Dark , by Carl Sagan
This book simply must top the list, because the late scientist and author Carl Sagan continues to be such a bright shining light in the critical thinking universe. Chapter 12 includes the details on Sagan’s famous “baloney detection kit,” a collection of lessons and tips on how to deal with bogus arguments and logical fallacies.

Clear Thinking: Turning Ordinary Moments Into Extraordinary Results , by Shane Parrish
The creator of the Farnham Street website and host of the “Knowledge Project” podcast explains how to contend with biases and unconscious reactions so you can make better everyday decisions. It contains insights from many of the brilliant thinkers Shane has studied.
Good Thinking: Why Flawed Logic Puts Us All at Risk and How Critical Thinking Can Save the World , by David Robert Grimes
A brilliant, comprehensive 2021 book on critical thinking that, to my mind, hasn’t received nearly enough attention . The scientist Grimes dissects bad thinking, shows why it persists, and offers the tools to defeat it.
Think Again: The Power of Knowing What You Don't Know , by Adam Grant
Intellectual humility—being willing to admit that you might be wrong—is what this book is primarily about. But Adam, the renowned Wharton psychology professor and bestselling author, takes the reader on a mind-opening journey with colorful stories and characters.
Think Like a Detective: A Kid's Guide to Critical Thinking , by David Pakman
The popular YouTuber and podcast host Pakman—normally known for talking politics —has written a terrific primer on critical thinking for children. The illustrated book presents critical thinking as a “superpower” that enables kids to unlock mysteries and dig for truth. (I also recommend Pakman’s second kids’ book called Think Like a Scientist .)
Rationality: What It Is, Why It Seems Scarce, Why It Matters , by Steven Pinker
The Harvard psychology professor Pinker tackles conspiracy theories head-on but also explores concepts involving risk/reward, probability and randomness, and correlation/causation. And if that strikes you as daunting, be assured that Pinker makes it lively and accessible.
How Minds Change: The Surprising Science of Belief, Opinion and Persuasion , by David McRaney
David is a science writer who hosts the popular podcast “You Are Not So Smart” (and his ideas are featured in A More Beautiful Question ). His well-written book looks at ways you can actually get through to people who see the world very differently than you (hint: bludgeoning them with facts definitely won’t work).
A Healthy Democracy's Best Hope: Building the Critical Thinking Habit , by M Neil Browne and Chelsea Kulhanek
Neil Browne, author of the seminal Asking the Right Questions: A Guide to Critical Thinking, has been a pioneer in presenting critical thinking as a question-based approach to making sense of the world around us. His newest book, co-authored with Chelsea Kulhanek, breaks down critical thinking into “11 explosive questions”—including the “priors question” (which challenges us to question assumptions), the “evidence question” (focusing on how to evaluate and weigh evidence), and the “humility question” (which reminds us that a critical thinker must be humble enough to consider the possibility of being wrong).

Warren Berger is a longtime journalist and author of A More Beautiful Question .
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes. Elements of Critical Thinking in Nursing To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
Critical Thinking. Nursing education has emphasized critical thinking as an essential nursing skill for more than 50 years. 1 The definitions of critical thinking have evolved over the years. There are several key definitions for critical thinking to consider. ... Applying Practice Evidence.
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient's cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the ...
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
Evidence-Based nursing practice, with its focus on empirical knowledge, relies on the features of critical thinking to provide an objective, goal-directed methodology for practice. A Delphi study of critical thinking in nursing2 identified skills integral to critical thinking in nursing practice. These include: analyzing, applying
Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student ...
The critical thinking concepts, identified in the Delphi study of nurse experts, were used to teach critical thinking in a continuing education course. 24 The objective of the course was to help nurses develop the cognitive skills and habits of the mind considered important for practice. The course focused on the who, what, where, when, why ...
Critical thinking makes the nurse a professional achiever who picks, integrates, analyzes, and utilizes knowledge. Nurses' actions in the caregiving process are realized with critical thinking skills. Critical thinking in nursing practice helps make an inclusive care plan with considerable potential for success.
Here are some examples of how nurses can apply critical thinking. Assess Patient Data: Critical Thinking Action: Carefully review patient history, symptoms, and test results. Example: A nurse notices a change in a diabetic patient's blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions ...
rience, and in nurturing and applying critical thinking skills in their formal academic and practical assessments. Readers are encouraged to engage with lots of interesting ... to further reduce the theory-practice gap by showing how skilled nursing practice incorporates critical thinking within person-centred care. In doing so Bob Price suc-
Nurses are critical thinkers. The characteristic that distinguishes a professional nurse is cognitive rather than psychomotor ability. Nursing practice demands that practitioners display sound judgement and decision-making skills as critical thinking and clinical decision making is an essential component of nursing practice.
The following inclusion criteria were examined: (a) clinical reasoning, clinical judgment, and critical thinking in nursing students as a primary study aim; (b) articles published for the last eleven years; (c) research conducted between January 2012 and September 2023; (d) articles published only in English and Spanish; and (e) Randomised ...
Abstract. Clinical reasoning is a multi-faceted and complex construct, the understanding of which has emerged from multiple fields outside of healthcare literature, primarily the psychological and behavioural sciences. The application of clinical reasoning is central to the advanced non-medical practitioner (ANMP) role, as complex patient ...
2002. TLDR. Nursing theories and frameworks as ways to enrich critical thinking in nursing practice; the inadequacy of the model of critical thinking as an individual, analytical process; and possibilities that are cocreated when critical thinking is conceived as a creative/constructive, relational/dialogical process. Expand.
Outcome of critical thinking in nursing practice; judgments begin with the end goal in mind; outcomes are met, involves evidence (Pesut, 2001) ... perseverance, and reflection. Critical thinkers in nursing practice the cognitive skills of analyzing, applying standards, discriminating, information seeking, logical reasoning, predicting and ...
The ability to perform thorough and focused assessments of patients' signs and symptoms combined with an objective examination of physiological and psychological systems to arrive at a diagnosis is a critical skill for nurse practitioners (NPs). Further, based upon the diagnosis, the NP must determine the best plan of care, often involving pharmacological and non-pharmacological strategies ...
The term 'critical' is used differently in social and clinical contexts. Nursing students need time to master the inquisitive and ruminative aspects of critical thinking that are required in academic environments. This article outlines what is meant by critical thinking in academic settings, in relation to both theory and reflective practice.
Nursing students need time to master the inquisitive and ruminative aspects of critical thinking that are required in academic environments. This article outlines what is meant by critical thinking in academic settings, in relation to both theory and reflective practice. It explains how the focus of a question affects the sort of critical ...
Background. The Institute of Medicine (IOM) has recommended that Evidence-Based Practice (EBP) be used in 90% of clinical decisions by 2020 [].EBP has become a popular buzzword in the healthcare industry [1, 2].This concept is defined as a problem-solving process in clinical decision making, which combines best research evidence with clinical expertise, patient preference, and clinical guidelines.
Promoting critical thinking is one of the primary objectives of nursing education programs all over the world. Using reliable and valid instruments to measure critical thinking is essential. The Nursing Critical Thinking in Clinical Practice Questionnaire (N-CT-4 Practice) is used internationally to assess critical thinking in nursing practice.
Applying critical thinking to nursing. This learning module outlines what is meant by critical thinking in academic settings in relation to theory and reflective practice. It explains how the focus of a question affects the sort of critical thinking required and offers two taxonomies of learning, to which nursing students can refer when ...
Neil Browne, author of the seminal Asking the Right Questions: A Guide to Critical Thinking, has been a pioneer in presenting critical thinking as a question-based approach to making sense of the ...